gout
- related: Rheumatology
- risks: obesity, alcohol, DM, men, aging
- premenopausal women don’t have gout
- not every one with increased uric acid has gout
- hyperuricemia >7 for male, >6 for female
- if > 10, risk increases to 30-50%
- goal < 6 if diagnosed with gout
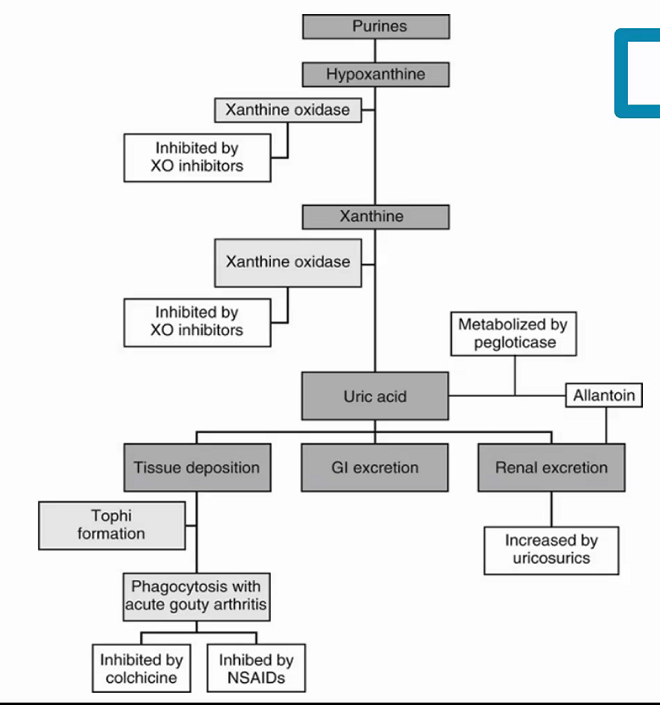
Pathogenesis
- pathogenesis: over producer or under excretor
- can do 24 hour collection. > 800mg in urine = overproducer. <800 = underexcretor (90% of problem)
- stages:
- asymptomatic hyperuricemia: decades
- acute intermittent gout: 8-15 years
- tophus: chronic
- nephrolithiasis
- time shortened or renal transplant pts on immunosuppresants
- triggers:
- alcohol
- hemorrhage
- dietary excess of purines
- stress: infections/trauma/surgery/exercise
- drugs: CANT LEAP, levodopa, theophylline, starting allopurinol
- cyclosporine
- alcohol
- nicotinic acid
- thiazides
- lasix
- ethambutol
- aspirin
- pyrazinamide
- can help: losartan, amlodipine, fenofibrate
- radiation
- fructose drink ingestion
- suggested diet:
- moderate calorie restriction
- increase in proportional protein intake
- increase low fat dairy products
- limit high fructose
- limit organ meats, seafoods
Diagnosis
- clinical findings: suspected vs probable
- imaging confirmation
- MSU crystals, negative birefringent, yellow when parallel
- inflammatory synovial fluid, neutrophil predominant
- septic synovial fluid may contain urate crystals
- intracellular crystals more confident to be gout than extracellular (phagocytosed). If only extracellular, think about infections
- during acute attack, serum uric acid level can be low or high
Treatment
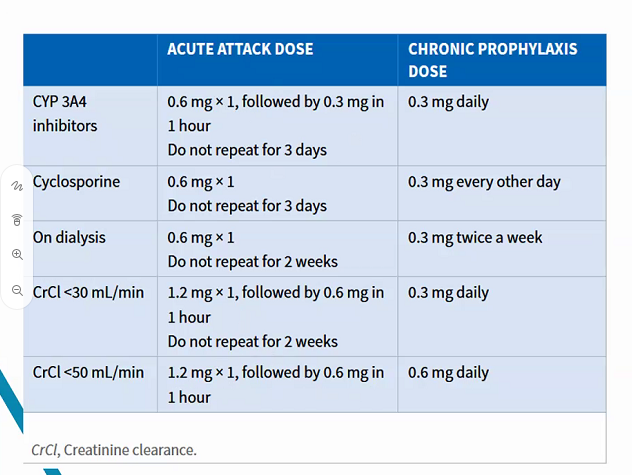
Colchicine is effective for acute gouty arthritis, but is limited by frequent gastrointestinal side effects and is a second-line agent. Colchicine is less effective than corticosteroids. Chronic administration in CKD patients can lead to colchicine accumulation in the blood and cause significant neuromyopathy.
Prevention
Allopurinol
- starting dose: no greater than 100mg/day
- CKD4 or worse: start at 50mg/day
- max dose: 800mg
- titrate 2-5 weeks to max dose. Can increase above 300mg daily, even with renal impairment
- toxicity: hypersensitivity reaction, elevated hepatic enzymes
- don’t use with azathioprine/mercaptopurine = pancytopenia
- may potentiate warfarin
- gout with tophi: even with goal uric acid, likelihood of gout flare up is higher than normal, 6 months colchicine with allopurinol
Urloric
- feboxostat Urloric
- dose once a day, can increase to 80mg
- advantage: can be used in Cr < 30, if allergic to allopurinol
- if gout flare occurs, does not need to be discontinued
- really used when CI to allopurinol
- colchicine: 6 months therapy when starting chronic ppx. 0.6mg BID
- Can also use NSAID or prednisone < 10mg
- don’t use colchicine with clarithromycin/CYP
- probenecid: excretes uric acid, CI in CKD pts or kidney stones
- start treating tout:
- tophus
- frequent attacks, 2 or more a year
- CKD 2 or worse: 1 gout attack
- hx of urolithiasis
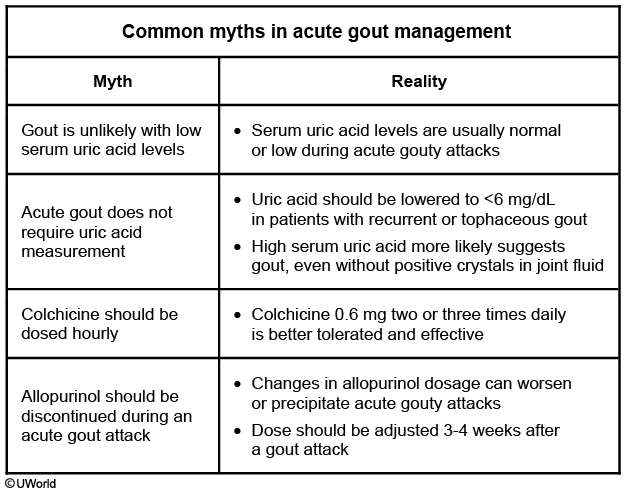
The allopurinol dose is increased until the patient’s serum uric acid level is < 6 mg/dL. Prophylactic colchicine is usually given for 6 months after the uric acid level normalizes. Patients who develop an acute gouty attack while taking allopurinol should not stop the drug or have their dose adjusted, since this can worsen the acute attack. The allopurinol dose may be adjusted 3-4 weeks after the acute inflammation subsides.