heart failure 9-2 lecture
- related: Medicine, Cardiology, heart failure
Definition
- HFrEF: <EF < 40%
- HFpEF: EF > 50%,
- Intermediate: HF with intermediate ejection 40-50%
- EF normal does not mean CO is normal. Can have preserved EF but low CO
Classifications
- NYHA: functional classification
- 1: no sx
- 2: sx with normal activity
- 3: sx with reduced activity
- 4: sx at rest
- ACC/AHA staging: more structural elements
- A: high risk of HF but no functional or structural. Hx CAD/HTN
- B: structural disorder, no sx
- C: previous or current HF sx with underlying structural disorder. Managed medically
- D: advanced requiring hospital support, transplant, palliative care
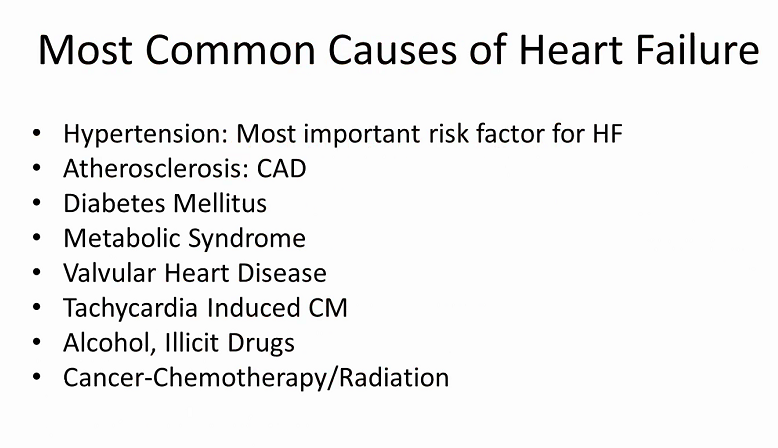
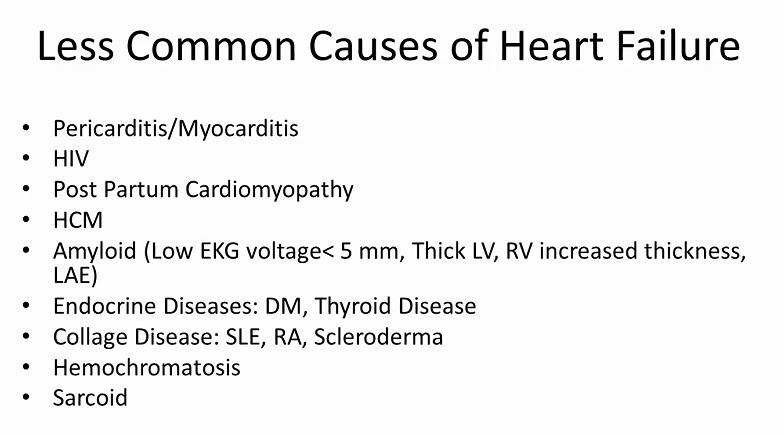
Causes
Labs
BNP:
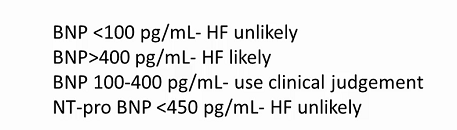
- For obese patient and pts with bad lungs: could be normal
Outpatient management
Define etiology
- Echocardiogram: HFpEF vs HFrEF, chamber size, wall thickness, wall motion, valve function
- Labs: HIV, TSH, toxicology, A1C, iron studies, BNP
- Ischemic evaluation
- cardiac MRI: sarcoid, myocarditis, viability, pericardial disease, amyloid
- PET scan: active sarcoid
- exercise test: cardiac vs non cardiac causes of sx. Sx out of proportion to HF
- endomyocardial biopsy: only for rapidly worsening dysfunction despite medical therapy (concern for giant cell myocarditis) or for infiltrative cardiomyopathy
Maintain euvolemia
- Euvolemia: JVP is flat and collapsing, no peripheral edema, no crackles, no sx, at dry weight
- Decongestion scores
- Lucas score: 3-5 has high mortality risk after discharge
- Everest score: absolute increase in death at discharge if >3
- Outpatient diuresis
- mildly overloaded, no significant AKI, no O2 requirement, no arrythmia
- Labs: BMP, mag
- Diuresis: double loop, consider metolazone/HCTZ if starting Lasix > 120mg
- goal 1-2 lb weight loss a day. Pt should call if not at goal
GDMT
- Uptitrate all to target doses
- SBP usually in 90s systolic
- Do not down titrate or stop with asymptomatic hypotension
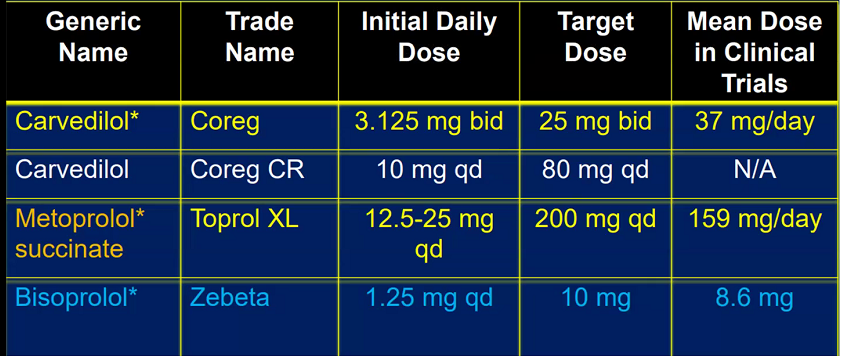
BB
- recommended for Stage B or worse
- start this dose, call in 10 days
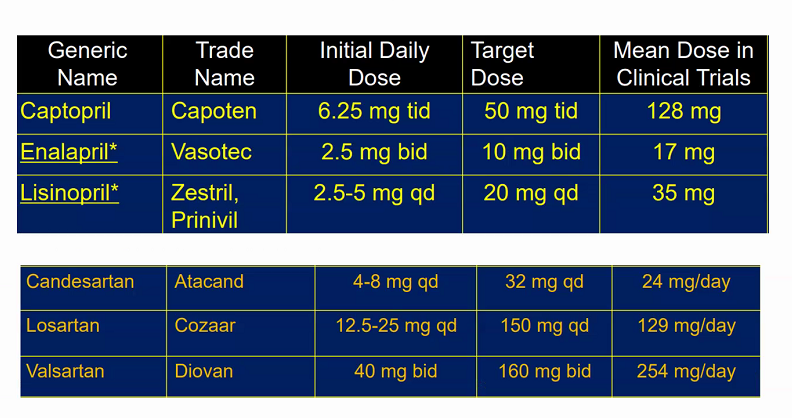
ACE/ARB
- Stage B or onward
Aldosterone antagonist
- Stage C and onward
- Do not start if K>5, Cr > 2 in women and >2.5 in men
Hydralazine/Nitrates
- C and worse
- In AA only
- Persistently symptomatic on ace/bb or intolerant due to Cr/K
ARNI, angiotensin receptor, neprilysin inhibitor
- Stage C, NYHA 2-4 HFrEF
- need to tolerate ACEI with good dose of BB
- Stop ACEI and washout 36 hours before starting
- Reduce diuretics as sacubitril has diuretic properties
Ivabradine
- no mortality benefit but decreases hospitalization
- Stage C, NYHA 2-4, resting HR > 70 despite being on max tolerated med
AICD
- NYHA 2-3
- EF < 35%
- survival expectancy > 1 year
CRT or CRTD
- CRT: resynchronization. CRTD both CRT and AICD
- NYHA 2-4
- EF < 35%
- EKG QRS > 150ms with LBBB
- Decreases mortality, hospitalization
HFPEF
- control BP, maintain euvolemia, revasculariation, manage afib
- aldosterone antagonists to decrease hospitalizations
Example questions
- newly reduced EF 25% with focal wall motion abnormalities, highest yield test is LHC
Inpatient Management
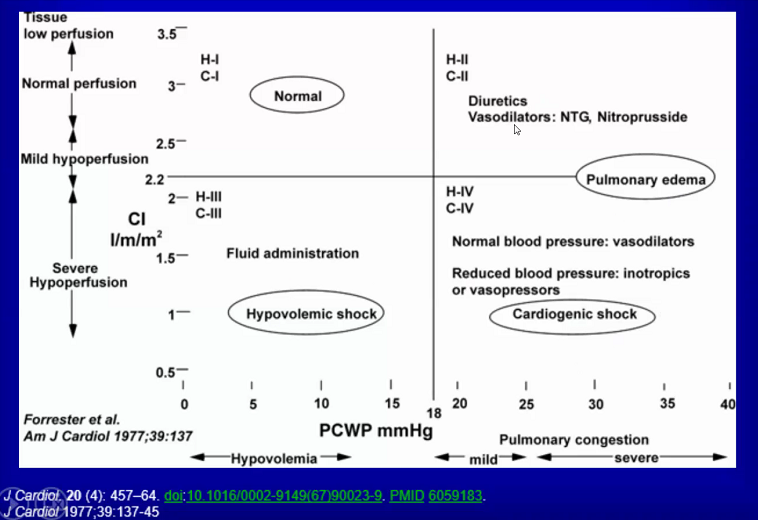
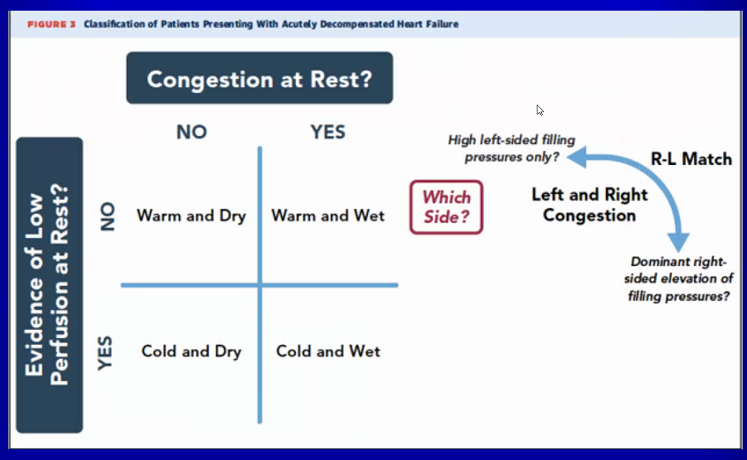
- Find if someone has low CO state. Try to catch them before they get into cardiogenic shock, when they are normotensive with low JVP instead at later stages with high PCWP and low CO.
- Do not continue BB in patient if decreased CO or symptomatic low BP
- increased lactate, abn liver function, symptomatic bradycardia
- continue ACE/ARB