multifocal atrial tachycardia
- related: Medicine, Cardiology, tachycardia
- tag: #literature #cardiology
- irregularly irregular like afib but has P waves
- automatic and triggered
- resides in atrium, so adenosine doesn’t work
- not reentry and not circle, so doesn’t respond to cardioversion
- amiodarone and procainamide can still be used
- MI, digoxin toxicity, CAD
- just stressful situations
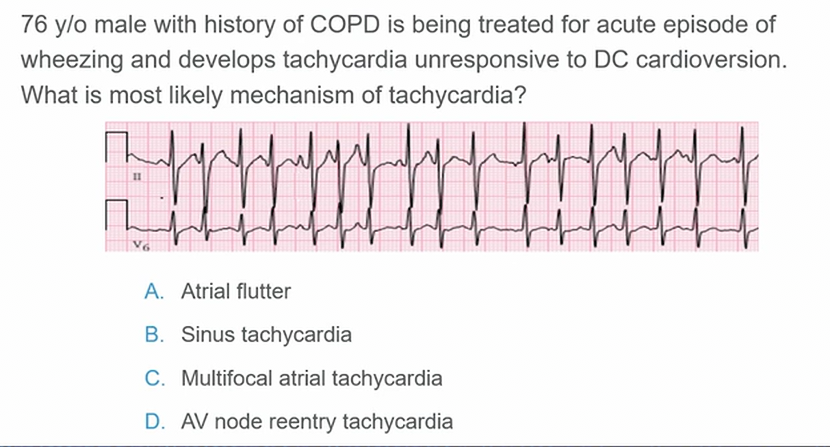
Multifocal atrial tachycardia (MAT) is an irregularly-irregular supraventricular tachycardia (SVT) characterized by the presence of 3 or more ectopic atrial pacemaking foci.
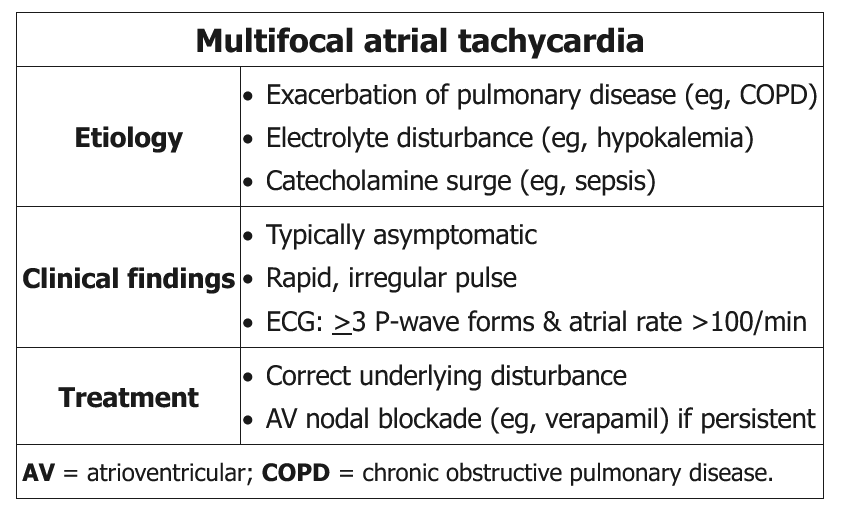
MAT occurs more commonly in patients with COPD, hypoxemia, and underlying pulmonary dysfunction. Other Less common etiological factors include hypokalemia, hypomagnesemia, sepsis, and theophylline or digitalis toxicity.
Most patients found to have MAT present with symptoms of an underlying pulmonary condition (e.g. shortness of breath, productive cough, chest pain). Only rarely do patients present with primary complaints of palpitations or syncopal episodes.
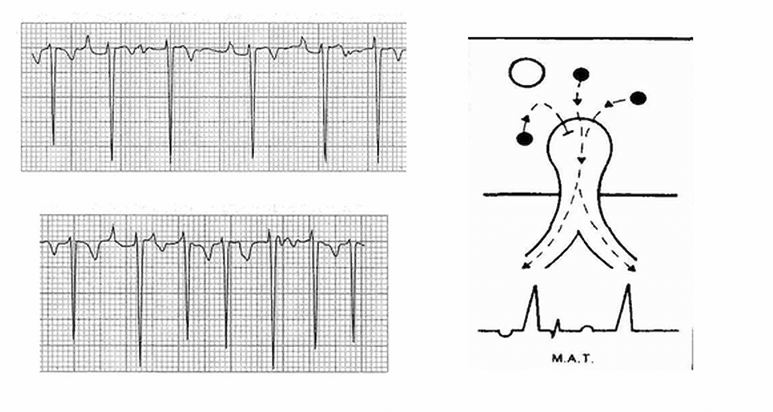
The best diagnostic test is an electrocardiogram (ECG), which will show an (irregularly) irregular rhythm with an atrial rate greater than 100 bpm and at least 3 morphologically distinct P waves on the same lead.
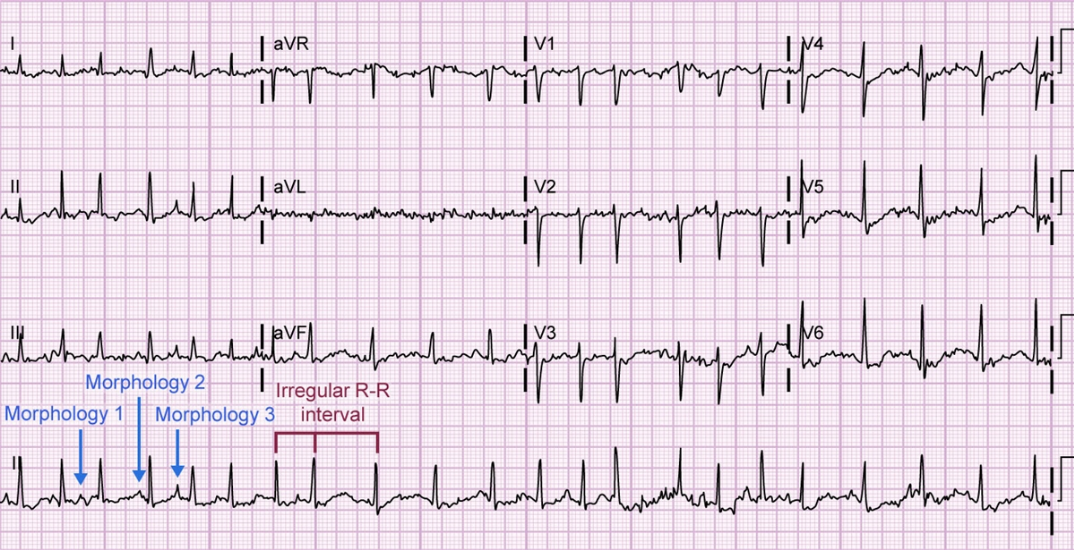
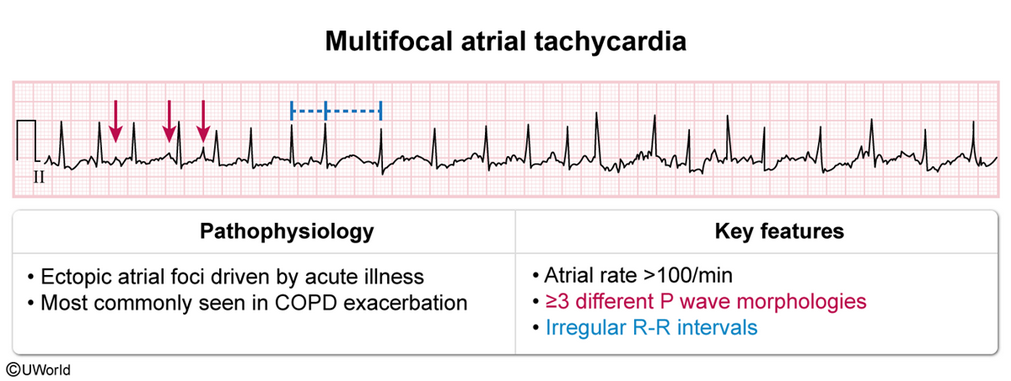
An ECG of MAT has the following defining features:
- An atrial rate of 100-200 BPM
- At least three morphologically distinct P waves occurring on the same lead
- P waves return to baseline
- P-P intervals, P-R duration, and R-R intervals vary
- Some P waves may not be conducted, but every QRS complex is preceded by a P wave
MAT can be suspected in patients with an irregular, rapid pulse and a history of pulmonary disease.
- Treatment
- Underlying condition: COPD, remove offending medications, correct electrolytes (especially K and Mg)
- Symtomatic tachycardia: rate control with verapamil or cardioselective BB (metoprolol, esmolol)
- For patients with ongoing, symptomatic MAT who cannot tolerate pharmacologic rate control, radiocatheter ablation of the AV node and concomitant pacemaker placement provide a final means of relief.