08 Pituitary pathology
Pituitary Adenoma
 ..
..
Symptoms
 .
.
Bitemporal hemianopsia
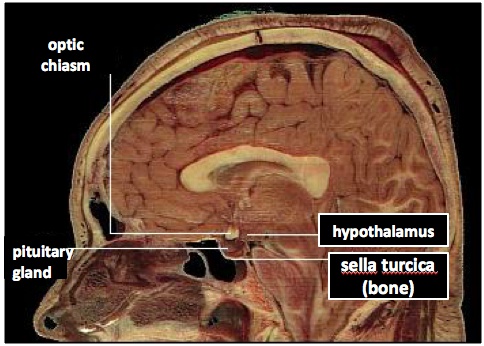
Pathogenesis:
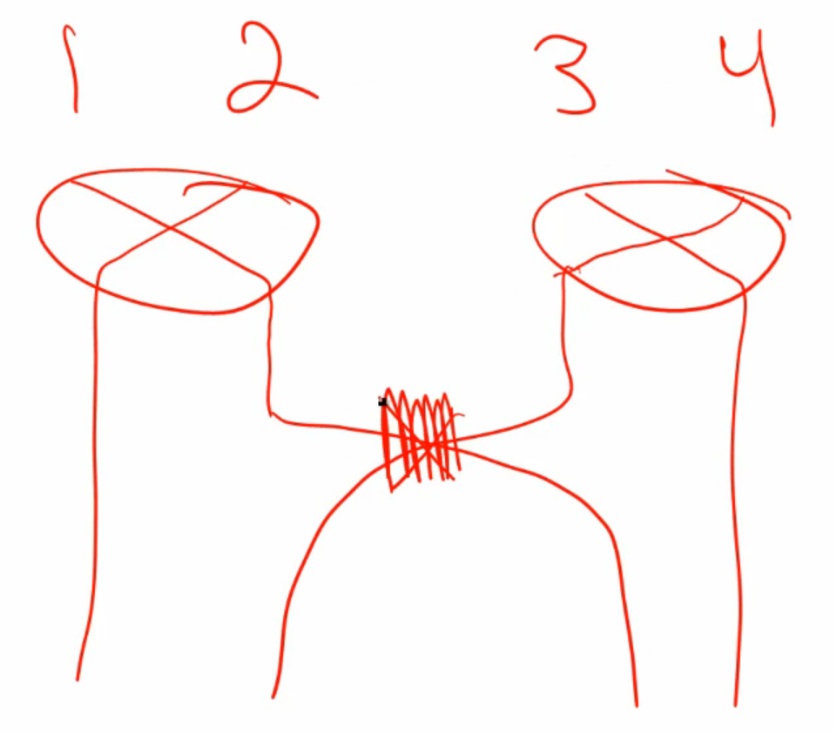 .
.
- Pituitary is next to optic chiasm. Enlargement of pituitary can cause vision problems.
Include:
- Prolactinoma: common
- GH adenoma
- ACTH adenoma: Cushings
- TSH, LH, FSH: rare.
Prolactinoma
- Benign tumor of lactotroph. Inhibits GnRH, thus LH/FSH
- Male: no breast lobular unit for milk
 .
.
Dopamine antagonists such as the antipsychotic risperidone and haloperidol. Antiemetics, metoclopramide. All of these block D2 receptors..
Treatment
- Dopamine agonists: bromocriptine or cabergoline to shrink tumor
- Surgery.
Dopamine agonists drugs.
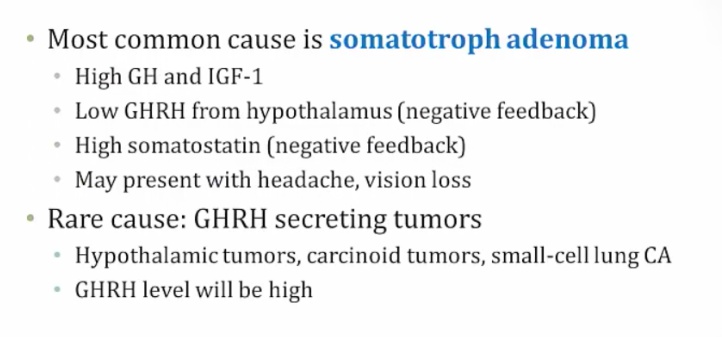
GH Excess
Causes are usually due to tumor. Presentation can be different depending on where the tumor is. If the tumor secretes GHRH and is in the hypothalamus or the sytem, there would be a high GHRH level. If the tumor is in the anterior pituitary, there would be a low GHRH and high somatostatin level.
.
Symptoms
.
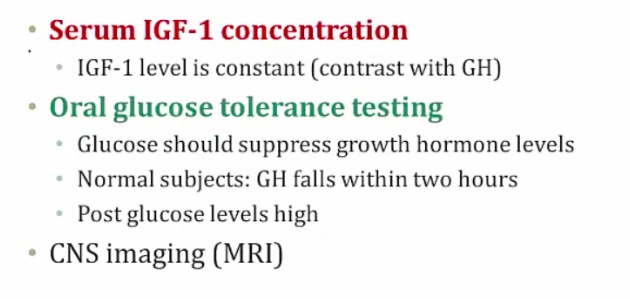
Diagnosis
.
Treatment
- pegvisomant: a GH receptor antagonist that effectively blocks IGF-1 production
 ..
..
Acromegaly
- Insidious onset, 12 yrs average: difficult to diagnose
- Enlarged features
- jaw, corse faces (enlarged nose, frontal bones)
- tongue
- hands and feet (rings no longer fit)
- larynx (voice deepens)
- Enlarged visceral organs
- Cardiac failure
- Enlarged joints: joint pain
- Secondary diabetes from GH induced liver gluconeogenesis
- Increased risk of colon cancer


.
Hypopituitarism
Describes the insufficient secretion of pituitary hormones resulting from diseases of the hypothalamus or the pituitary. .
The majority of cases are secondary to destructive processes directly involving the anterior pituitary. This includes:
- Tumors, such as nonfunctional pituitary adenomas (adnomas not producing hormones) or craniopharyngiomas(exert pressure on adjacent pituitary cells)
- Pituitary surgery or radiation
- Traumatic brain injury and subarachnoid hemorrhage
- Pituitary apoplexy (sudden hemorrhage into the pituitary gland)
- Sheehan syndrome (postpartum necrosis of the anterior pituitary secondary to infarction precipitated by obstetric hemorrhage or shock)
- Empty sella syndrome (presence of an enlarged, empty sella turcica due to a condition that partially or totally destroys the pituitary gland; classically affects obese women with a history of multiple pregnancies).
 ..
..
The clinical manifestation of hypopituitarism depends on the specific hormone(s) that are lacking. For example, a deficiency of melanocyte stimulating hormone (MSH) may manifest as hypopigmentation, due to MSH’s stimulatory effects on melanocytes.
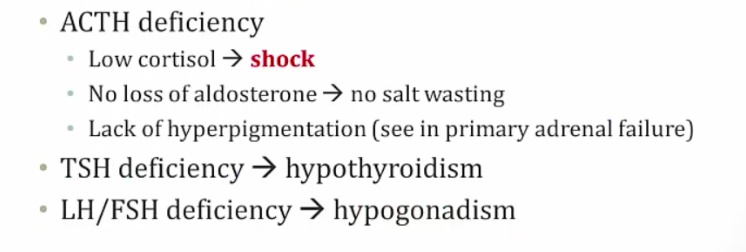
Aldosterone part of RAAS system, not adrenal system…
The treatment for hypopituitarism includes hormone replacement therapy, including:
- Corticosteroid
- T4 (thyroxine)
- Sex steroids
- Human growth hormone
- Pulsatile GnRH (for patients that desire fertility)..
Empty Sella Syndrome
- Arachnid and dura matter around sella. Pia matter around pituitary
- Herniation of arachnoid and CSF into sella compresses and destroys pituitary: hypopituitarism
- Sella filled with CSF, which is clear on imaging..
 .
.
Pituitary Apoplexy
.
Sheehan’s Syndrome
Pituitary gland enlarged in preglancy as result of increased prolactin. However, the blood supply is not increased. In postpartum hemorrhage, pituitary is at risk of infarct from hypotension…
Can present as shock after delivery from low cortisol levels if severe. If not severe, present as failure to lactate from loss of prolactin
Other symptoms:
- Absent menstruation from low FSH/LH
- Loss of pubic and axillary hair from low FSH/LH
- Cold intolerance from low TSH
- Fatigue from low GH
- Anorexia
.
Posterior Pituitary Pathology
DI
Is due to:
- Central DI: a lack of antidiuretic hormone (ADH)
- Nephrogenic DI: a **lack of ADH functionality **in the collecting tubules..
Is characterized by:
- Dilute urine (even after water restriction)
- Intense thirst
- Polyuria.
Labs:
- hypernatremia
- Urine specific gravity < 1.006
- Serum osmolarity > 290 mOsm/L..
A water restriction test is used to diagnose central and nephrogenc DI:
- Water intake is restricted for 2-3 hours, and urine volume, urine osmolality, plasma Na+ concentration, and plasma osmolality are measured hourly.
- In healthy individuals, water deprivation leads to a urine osmolality 2-4 times greater than plasma osmolality.
- In patients with central or nephrogenic DI, urine osmolality will be less than 300 mOsm/kg after water deprivation..
- Central: low ADH
- Nephrogenic: high ADH
DDAVP (desmopressin, an ADH analog) is administered to differentiate between central and nephrogenic DI:
- In central DI, DDAVP administration will result in a 50% or greater increase in urine osmolality.
- In nephrogenic DI, DDAVP administration will lead to no change in urine osmolality..
Central Diabetes Insipidus
- radiation, surgery, trauma
.
Treatment: Desmopressin.
Nephrogenic Diabetes
Is due to the inability of the kidney to respond to ADH. This may be due to an inherited mutation in the V2 receptor or secondary to:
- Lithium (drug-induced nephrogenic DI)
- Demeclocycline (reduces responsiveness of kidney tubules to ADH) (treats SIADH)
- Hypercalcemia (causes natriuresis and water loss)
- Hypokalemia (decreases responsiveness of kidney tubules to ADH)
- Sickle cell disease (impairs renal response to ADH)..
Treatment involves:
- Adequate hydration
- Hydrochlorothiazide (see below)
- Indomethacin
- Amiloride.
Why treat a water-wasting disease with a thiazide diuretic? Thiazides increase renal Na+ excretion, which leads to extracellular fluid volume contraction. This decreased volume will decrease GFR, and increase proximal tubular reabsorption of water and Na+. Therefore, ultimately less water and Na+ are lost as urine.
SIADH
Occurs when too much ADH is secreted by the posterior pituitary. Common CNS causes of SIADH include:
- Brain infections (encephalitis)
- Tumors of the pituitary, or tumors that impinge on the pituitary
- Head trauma
- Psychiatric illness
Non-CNS causes of SIADH include:
- Medications (chlorpropamide, carbamazepine, cyclophosphamide and SSRIs)
- Ectopic production by lung tumors (especially small cell carcinoma)
- Pulmonary infection (viral, bacterial or tuberculous pneumonia)..
Patients will generally present with euvolemic hyponatremia. Total body water is increased, but near-normal blood volume is maintained due to the body’s compensatory response (decreased thirst, suppressed aldosterone release). Peripheral edema does not develop.
If asymptomatic, the treatment of SIADH is free water restriction.
Treatment of SIADH includes:
- Demeclocycline, an antibiotic (tetracycline) used to treat SIADH because it induces a state of nephrogenic diabetes insipidus by inhibiting the actions of ADH in the kidney. This allows for diuresis and less retention of water.
- Vaptans (conivaptan, tolvaptan), which are vasopressin antagonists
- Hypertonic (5%) saline should also be administered if severe CNS changes (e.g. seizures) are present.
It is important that hyponatremia be corrected slowly. A rapid correction of hyponatremia can lead to central pontine myelinolysis (aka osmotic demyelination syndrome)..
Damage to the myelin sheath of the pons leads to the patient becoming “locked in”, with intact cognitive function but total muscle paralysis, with the exception of eye blinking..
In SIADH, urine osmolarity is greater than serum osmolarity..