10 Cardiac Ischemia
Ischemic Syndrome
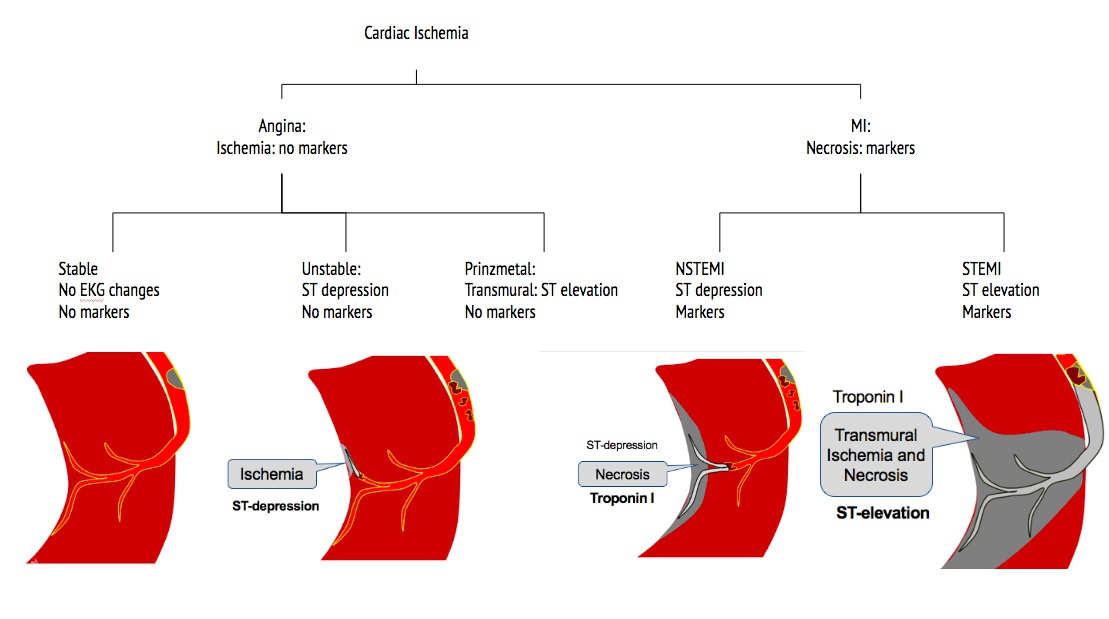
Angina vs MI:
- Angina: Symptoms relieved by NG; MI not relieved by NG
- stable: unruptured plaque, blocking blood flow. RBC squeeze through. Symptoms with exertion. May have ST depression during symptoms
- unstable angina: ruptured plaque, clot, subendothelial (ST depression) ischemia (no markers)
- prinzmetal: transmural (ST elevation) ischemia (no markers)
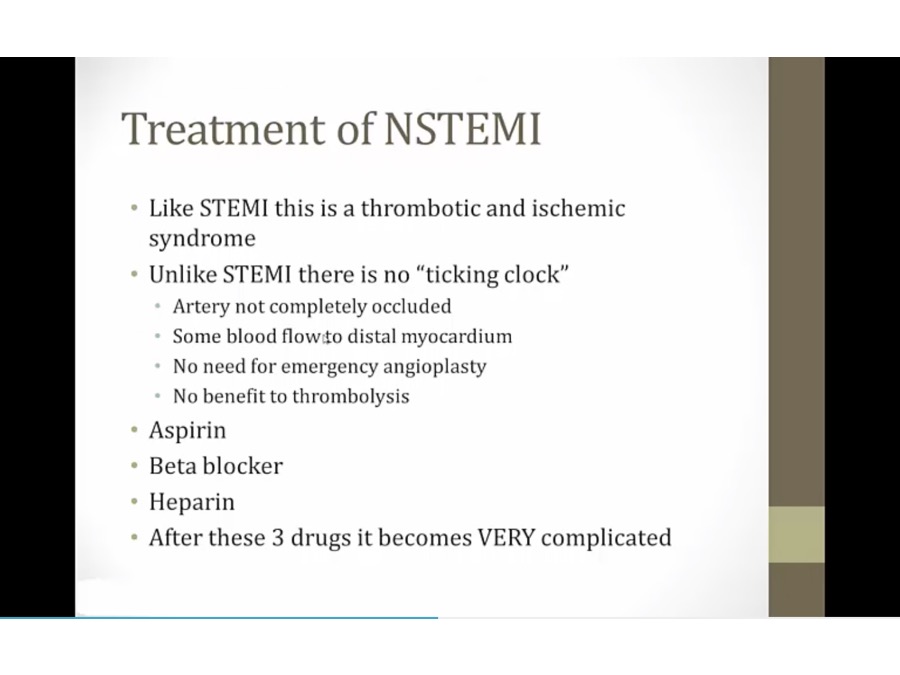
- NSTEMI: subendothelial necrosis, clot not completely obstruct artery (not transmural yet)
- STEMI: transmural necrosis, clot completely obstructs artery, transmural
- coronary ischemia most cause of sudden death, except with HCM in young people
Symptoms
- angina: squeezing type of chest pain
- lavigne sign: patient place hand over chest
- vagus run along inferior wall of heart, can be stimulated with inferior MI
Risks
- angina, MI in past highest risks
- other very high risks
Cardiac Markers
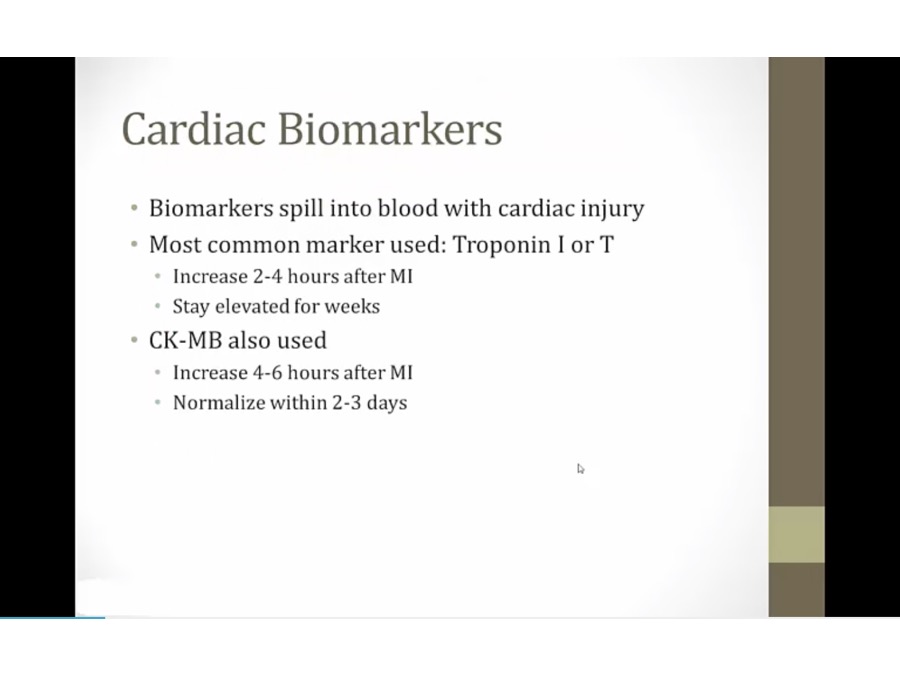
- 1 hour after chest pain: no cardiac marker, nl biomarkers
- pt with rhabdo will have very high CK, but mostly MM
- liver enzyme
EKG
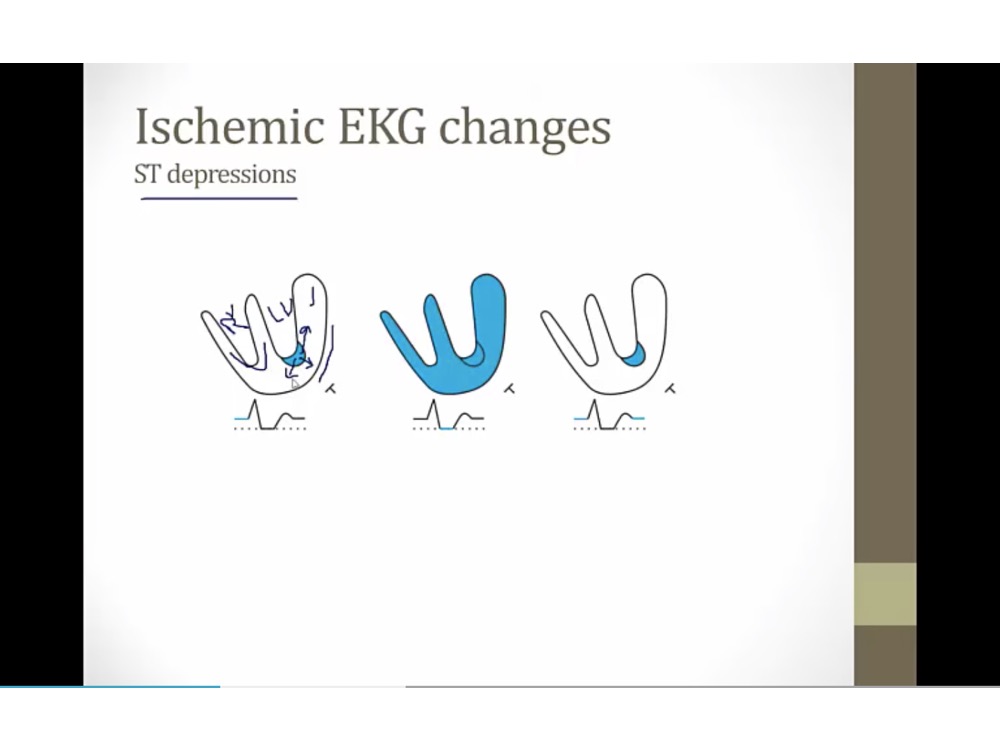
ST depression
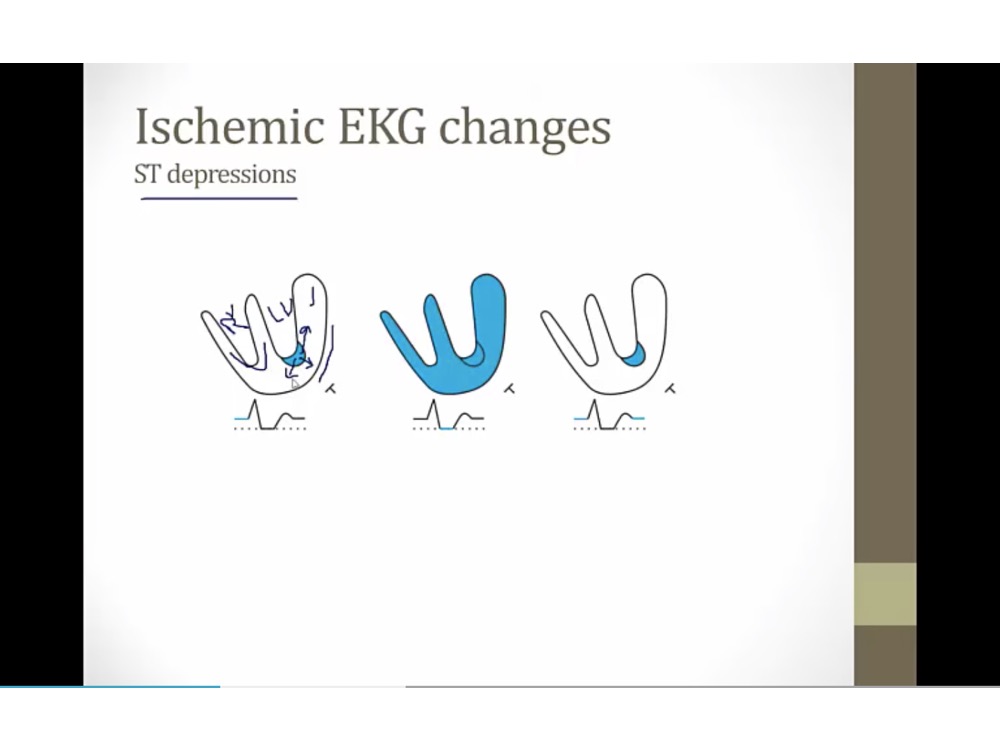
- blue: small area of subendocardial ischemia
- endocardium can get blood from ventricle. Subendo receive blood from epicardial vessels, most vulnerable to ischemia
- in mild ischemia: subendo ischemic first
- ischemic tissues create electric current going away from it
- T: EKG lead looking at LV
- At baseline: T sees current heading towards it (elevated ST baseline)
- Heart depolarize: everything at normal baseline
- repolarize: elevated baseline again
- Appears to have ST depression, in reality, baseline elevation
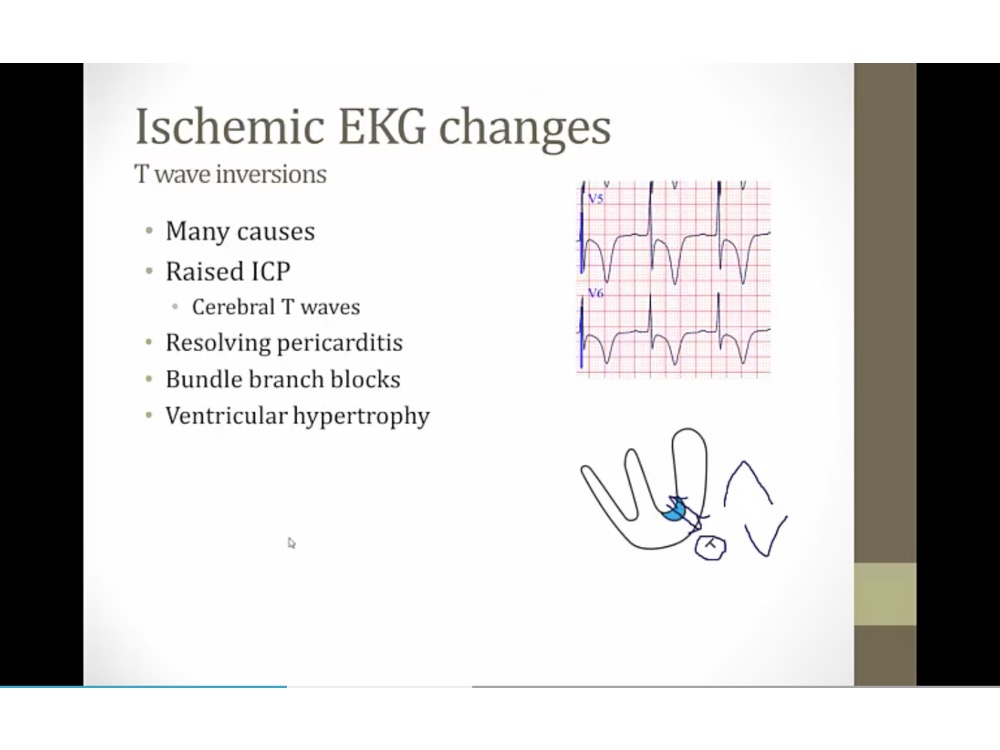
T inversion
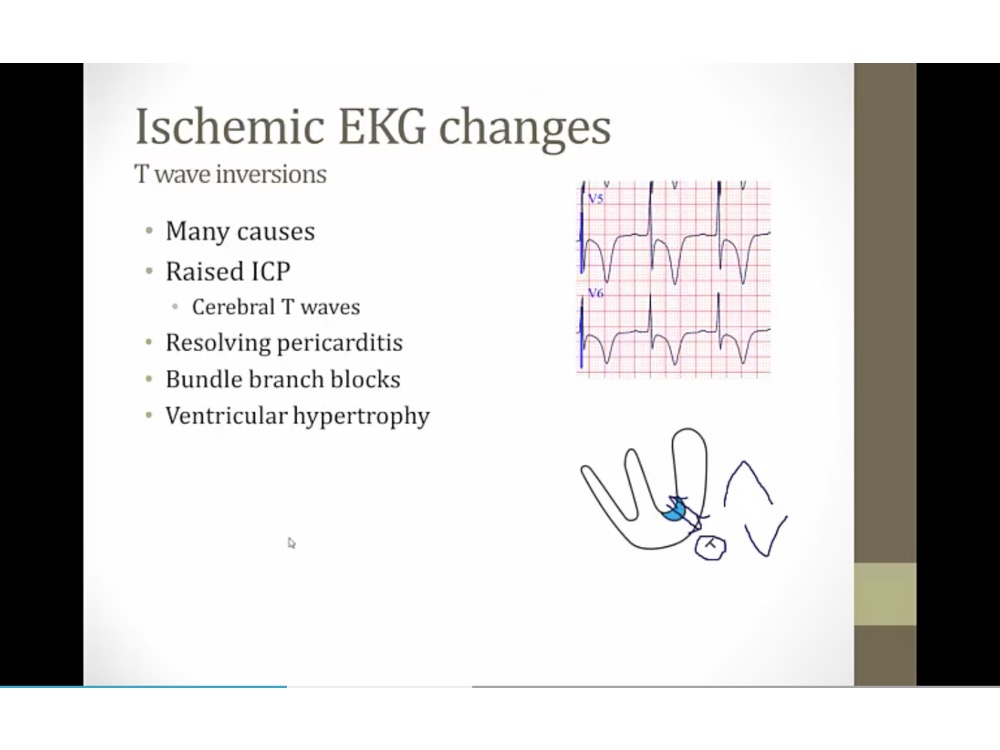
- normally: subendo repolarizes first, current goes to T, create upward T wave from current heading towards it
- subendo ischemia: subendocardium repolarizes last, reversing wave of repolarization, going away from T, inverted T
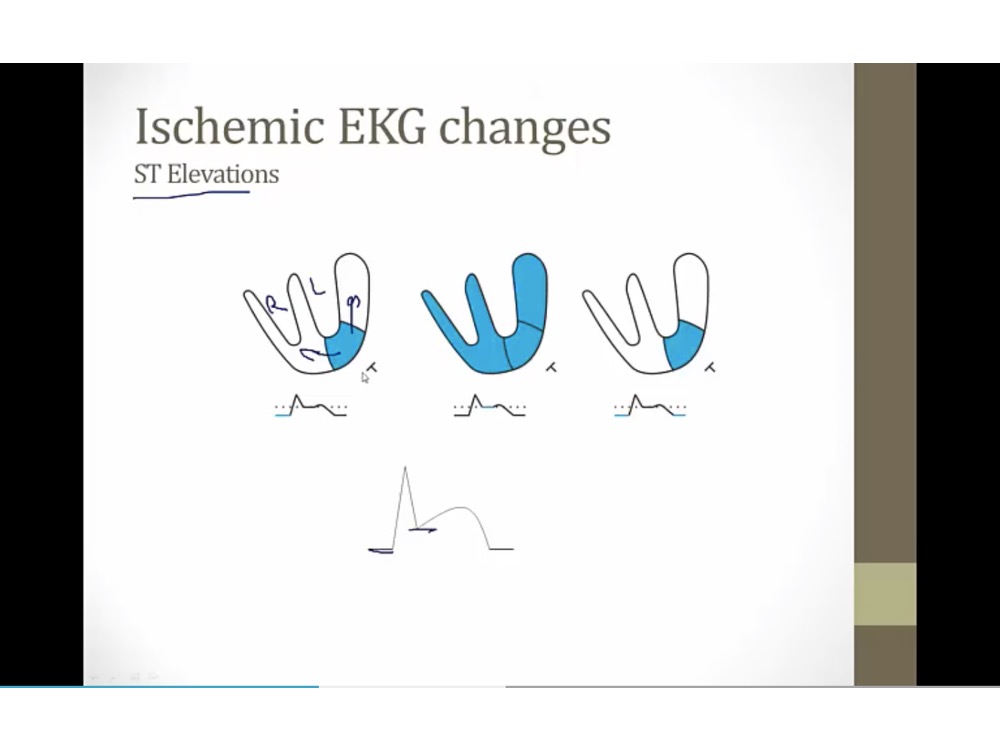
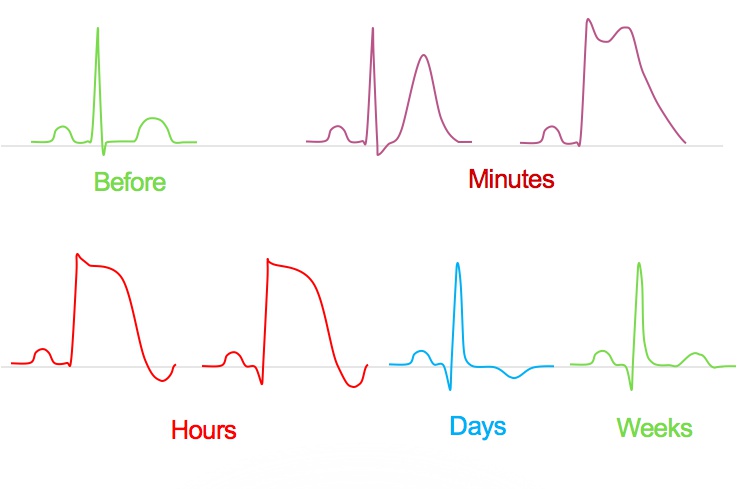
ST Elevation
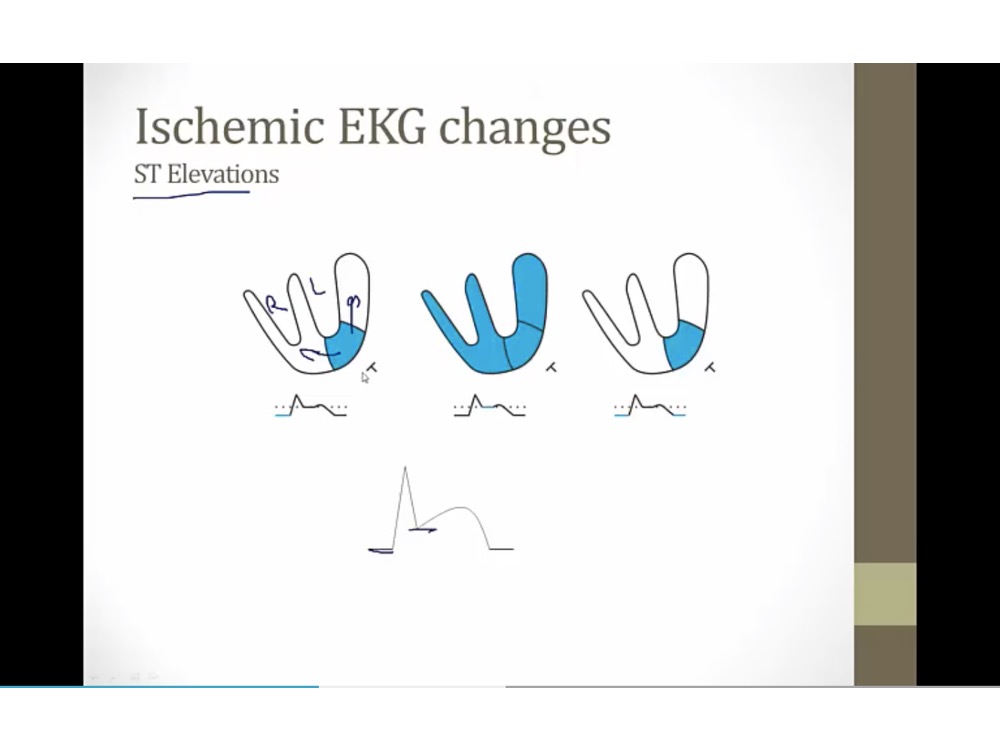
- transmural ischemia, current away from it
- baseline: T sees current heading away, depressed baseline
- depolarizes: everything at baseline
- repolarizes: depressed baseline again
- ST elevation = baseline ST depression
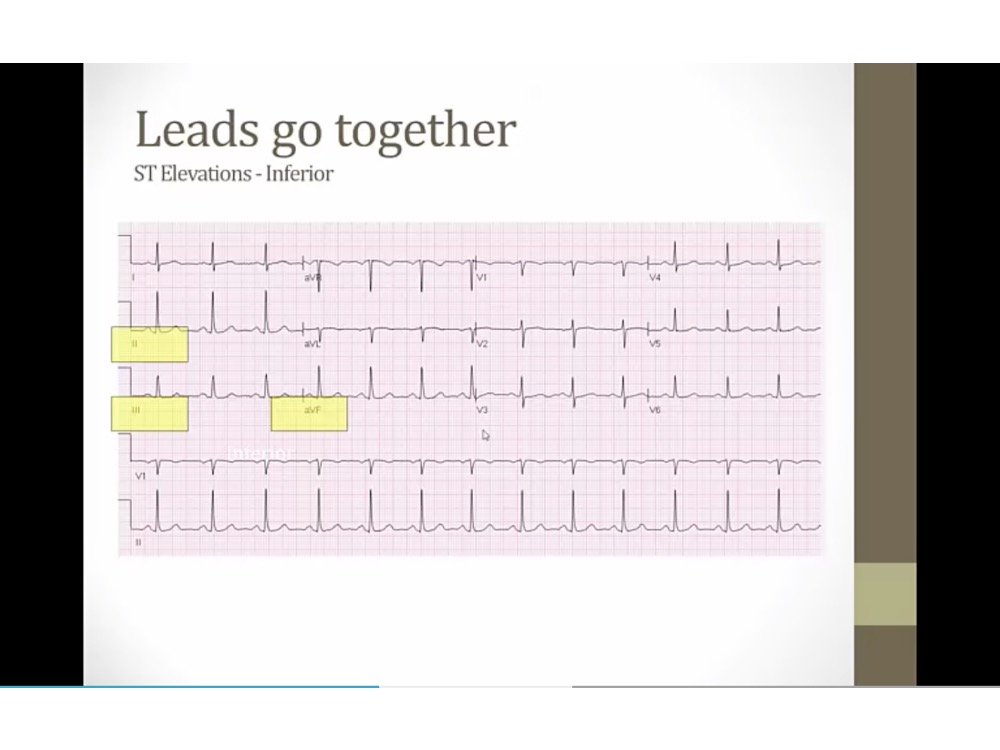
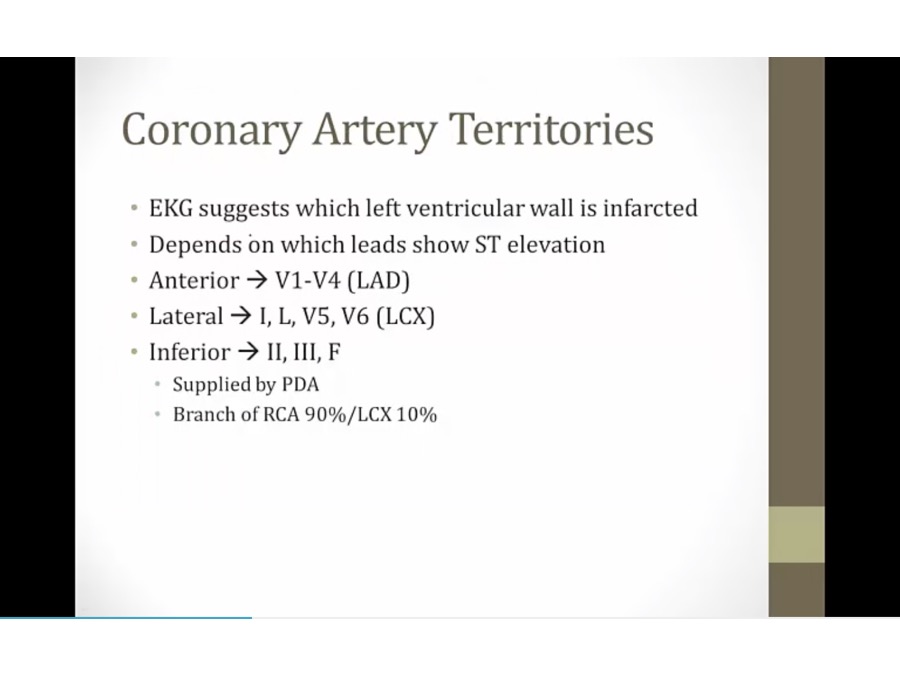
STEMI
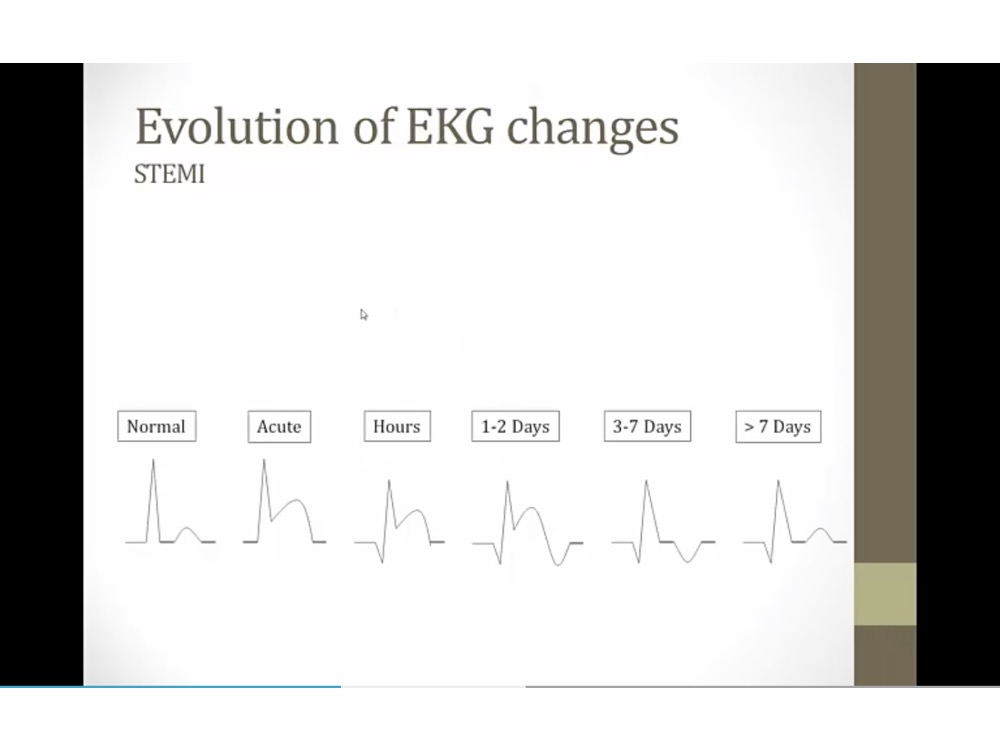
- transmural MI progression
- Q wave after a few hours, but also represent old infarction
- T wave invert after few days
- normal ST
- T wave normal, Q wave remain
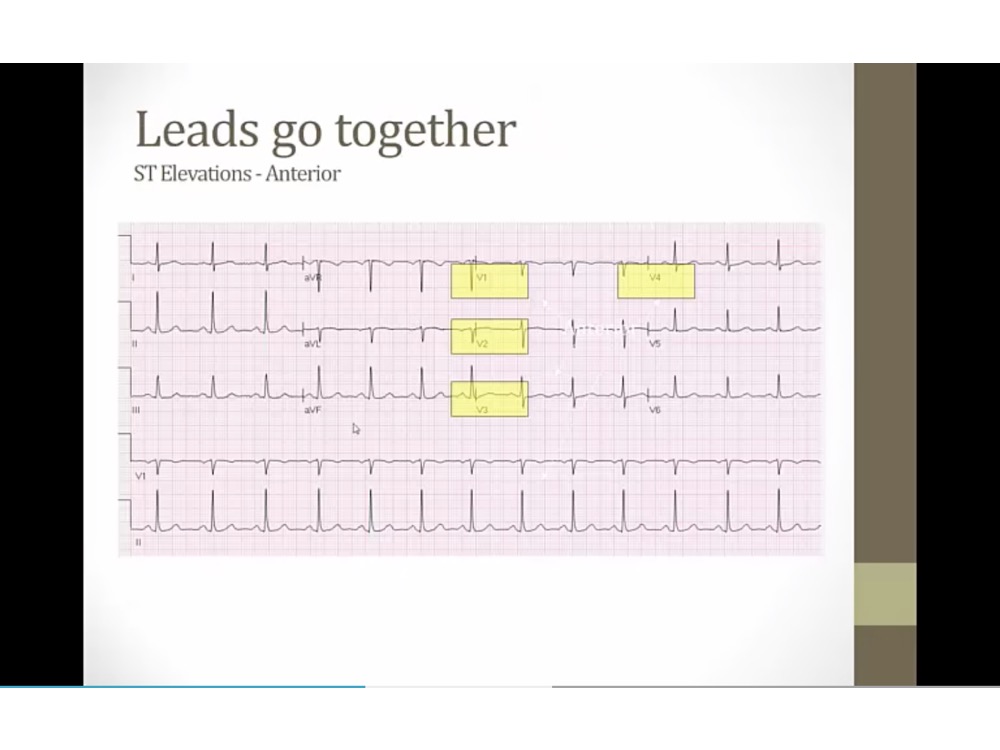
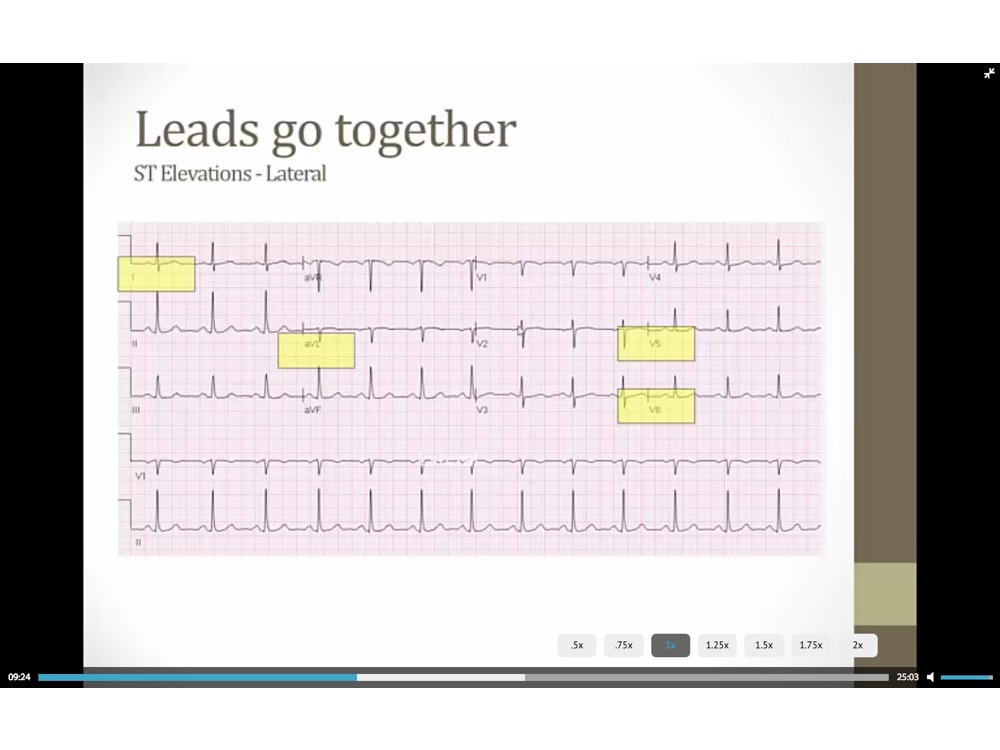
- tell which leads ischemic with transmural infarct
- anterior wall
Progression and Complications
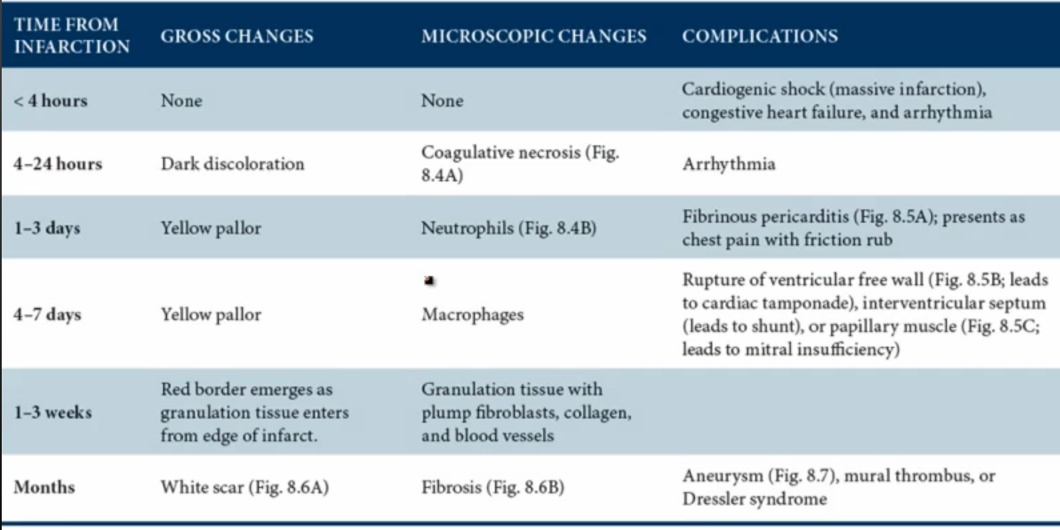
Overview:
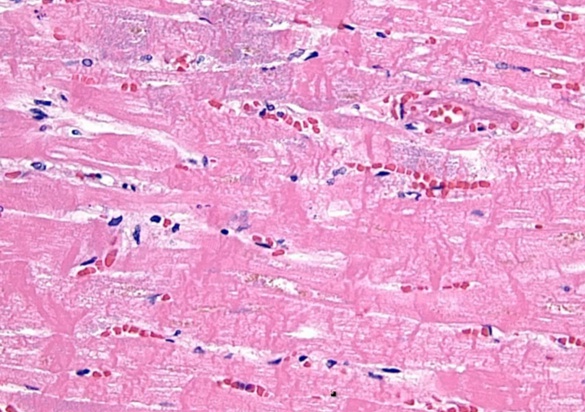
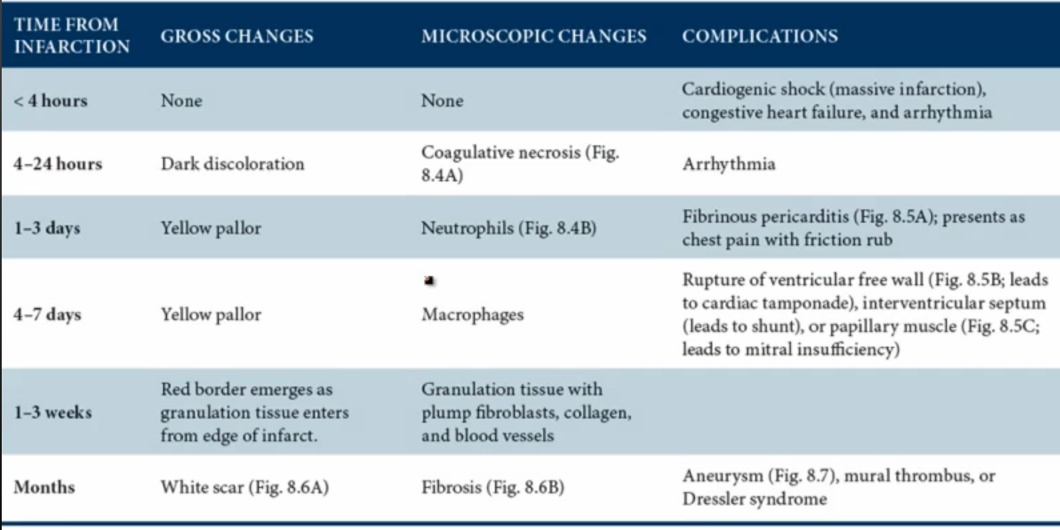
- 1st thing: coagulative necrosis: removed nucleus from cells
- 2nd: acute inflammation with neutrophils/macrophages
- 3rd: healing, granulation, then conversion to scars
< 4 hours:
- congestive heart failure: blood back up and can’t pump
- arrythmia from damaged conduction
1-7 days:
- WBC gives yellow pallor gross color
- complication depends on whether neutrophil or macrophages
- neutrophil: transmural inflammation, exudate leak to pericardium, pericarditis. Only with transmural inflammation
- macrophage: eat up all dead debris, wall = weakest, rupture
1-3 weeks:
- granulation: blood vessels, red border from outside, from normal tissues
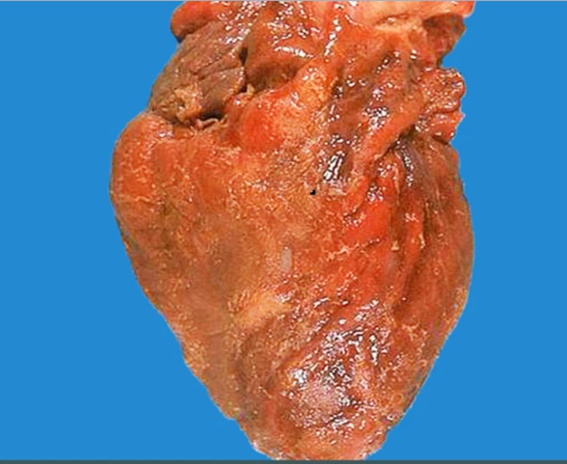
months:
- scar: not as strong as myocardium, not good movement, stasis, aneurysm/thrombus
- 1 day, 1 week, 1 month
- 1st day: coagulative necrosis
- after 1st day: inflammation up to 1 week, neutrophil then macrophage
- after 1 week: granulation
- 1 month: scar
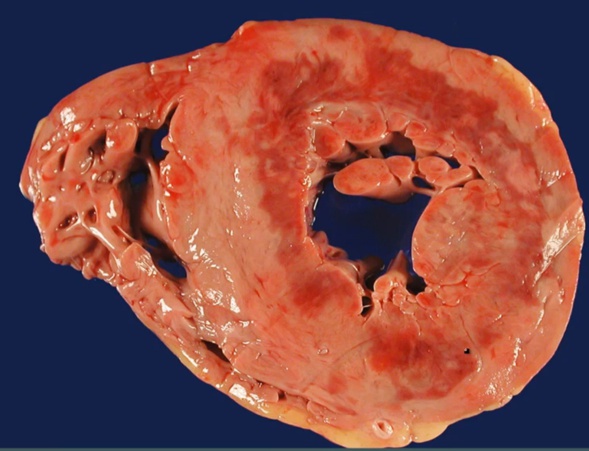
- subendo, mottled color
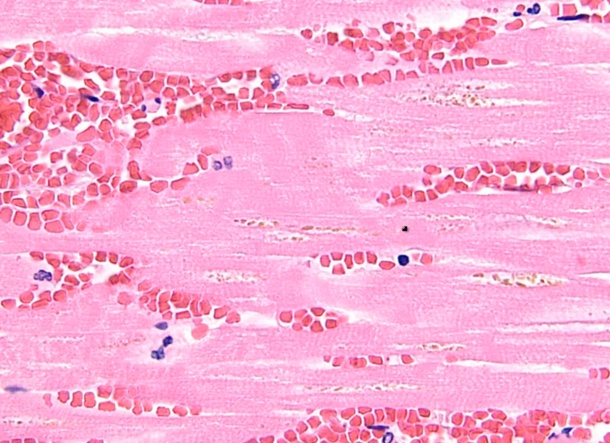
- coagulation necrosis
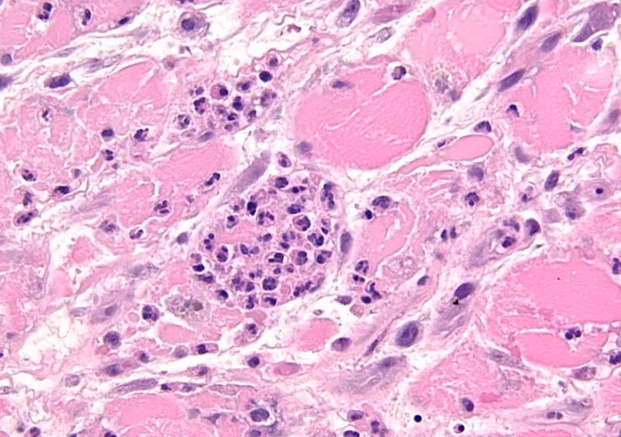
- inflammation
- pericarditis

- rupture
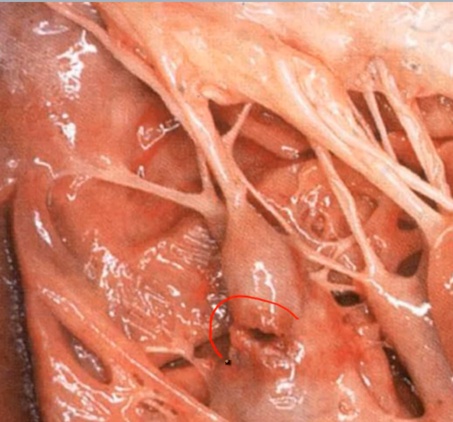
- papillary muscle

- scar
- collagen, CT, type 1
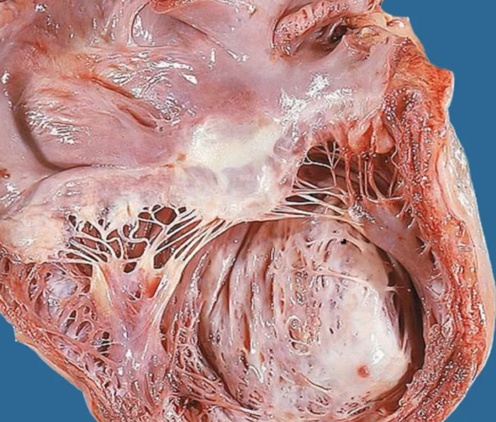
- aneurysm
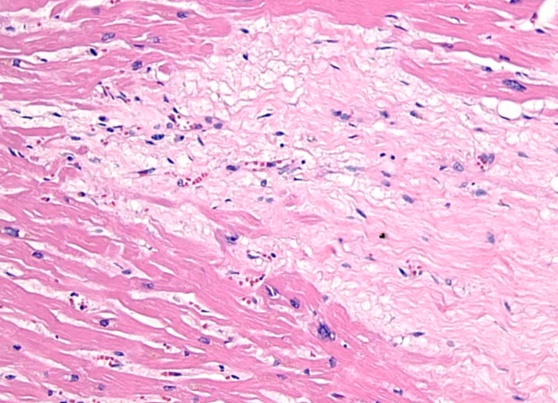
- return of blood flow: contraction band
- return blood flow, Ca inflow into dead cells, contraction of muscle fibers, dense contraction bands
- reperfusion: free radicals from O2 coming back. Cardiac enzyme continue to rise after open up clot
Complications
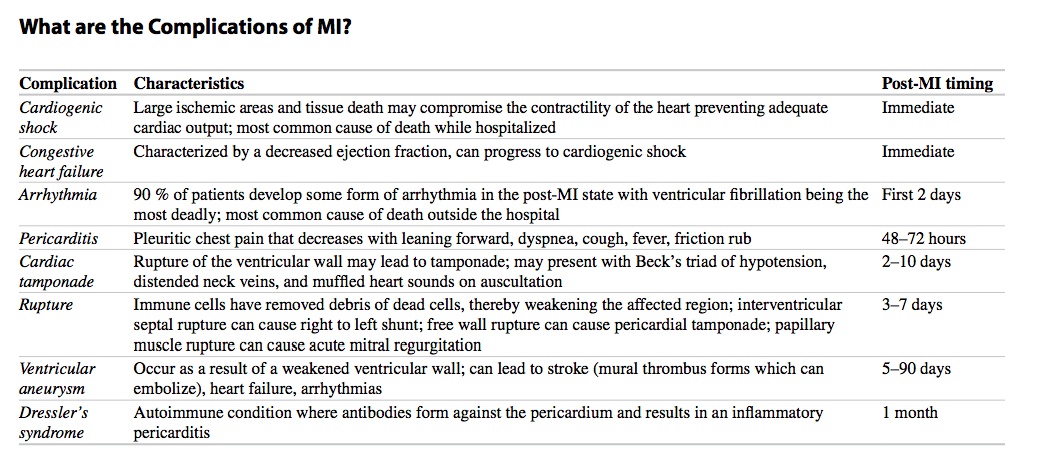
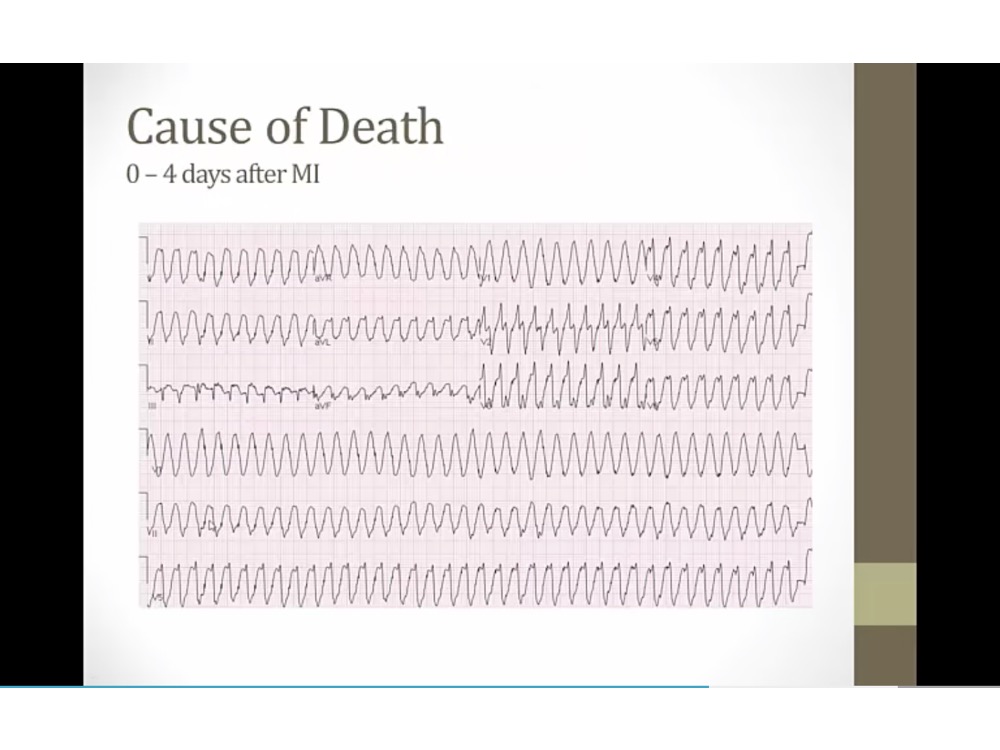
- VTACH, can deteriorate into cardiac arrest
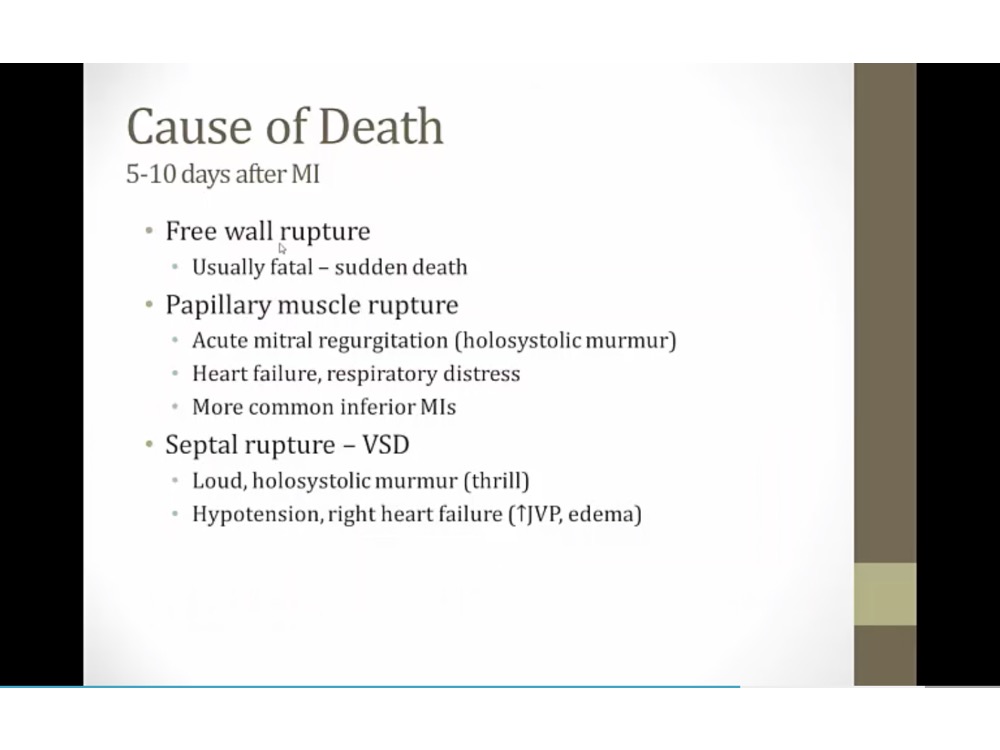
- can cause tamponade if accumulation of fluid
- inferior wall: papillary muscle with single supply from RCA
- thrill: feel with hand
- hypotension: blood leaks from left to right
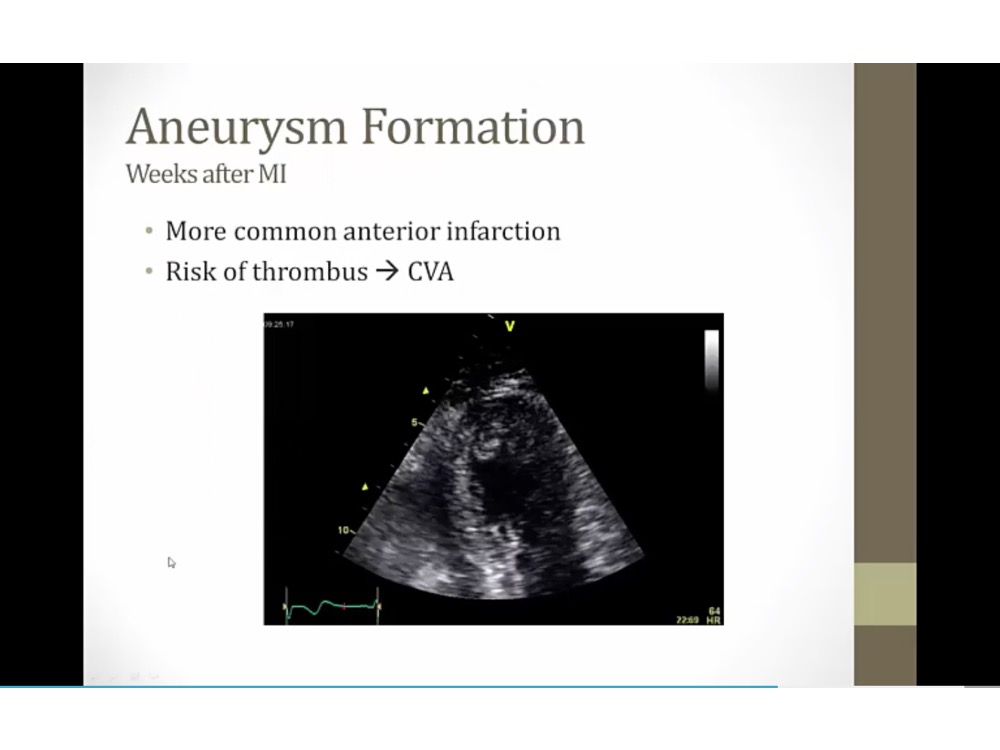
- US: apex with akinetic tissue, aneurysm with stasis of blood on left side
- can have stroke if a piece breaks off
- anterior infection: most common
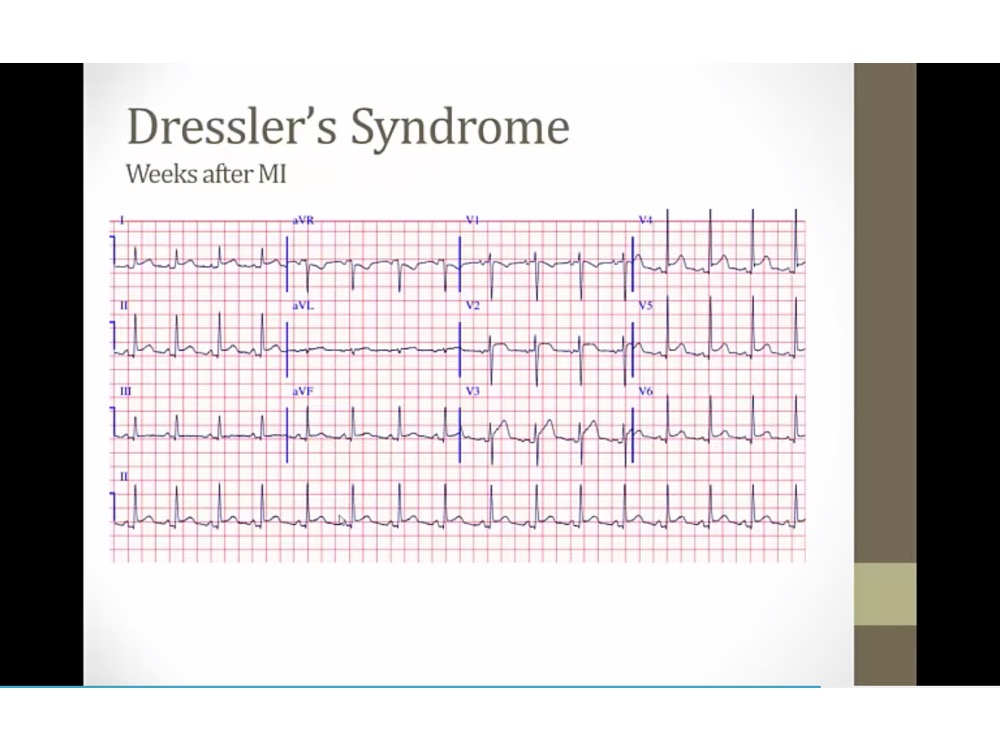
- EKG with pericarditis
- diffuse ST elevation
- PR depression, down going
- autoimmune
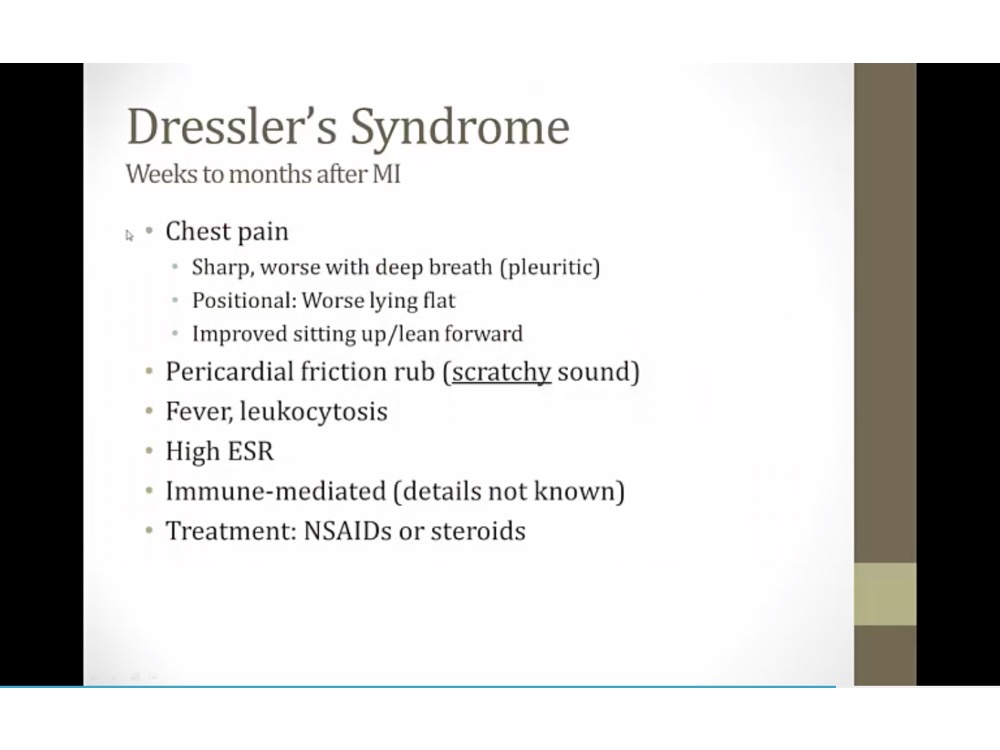
- like sand paper
- extension of inflammation into pericardium
Treatment
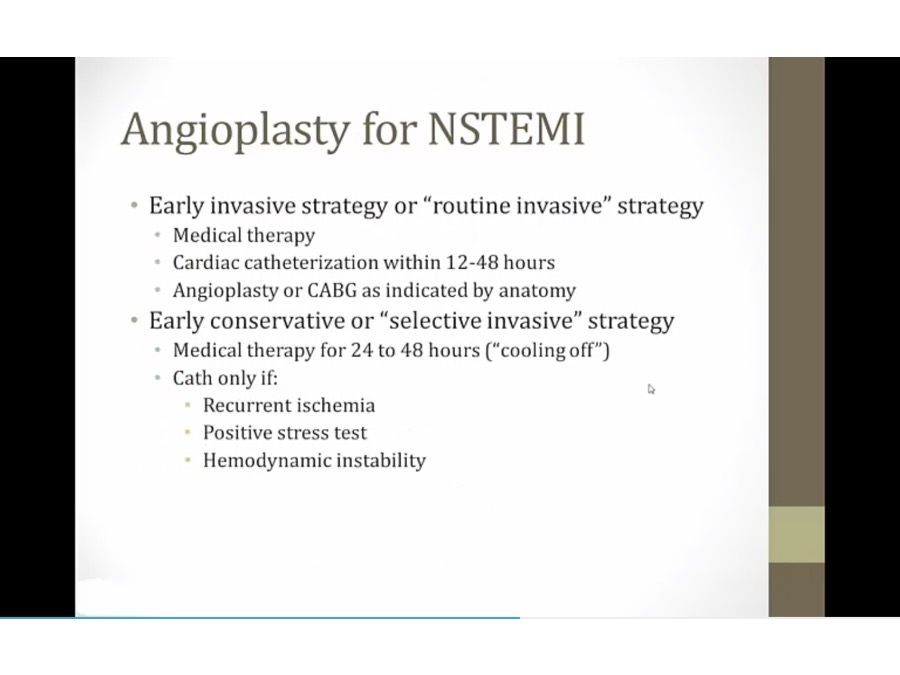
Revascularization
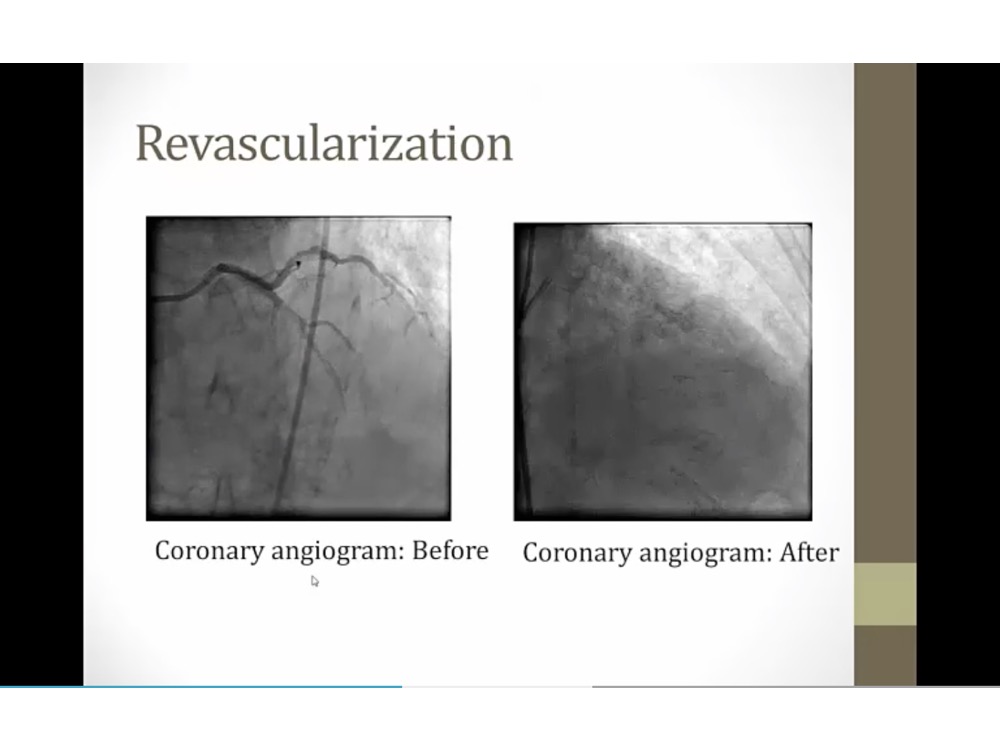
- dye with fluoroscope
- put in stent
- balloon first to push the plaque, then leave stent (chickenwire) in
- PCI: going across skin to access artery
- PTCA: lumen of artery to get to coronary artery
- PCI: within 90 min of symptoms onset
- more than 90 min: tpa
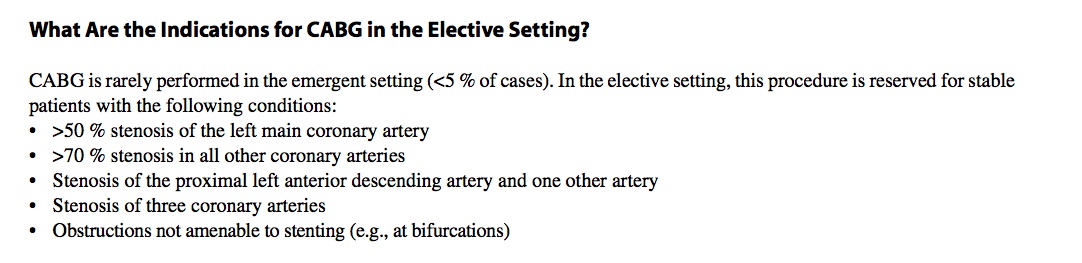
- PCI unsuccessful: emergency CABG
- systolic dysfunction: cardiomyopathy with reduced LV EF
- hibernating myocardium: myocardium so little flow that going into hibernation
- in valve surgery: treat blocked artery at same time
Bypass
- bypass backup option
Medication
Prevention
- trigger inflammation when put in
- drug: sirolimus/tacrolimus to prevent stenosis
- thrombosis: complete closure of stent by blood clot inside
- endothelialization: scar tissue grew over stent
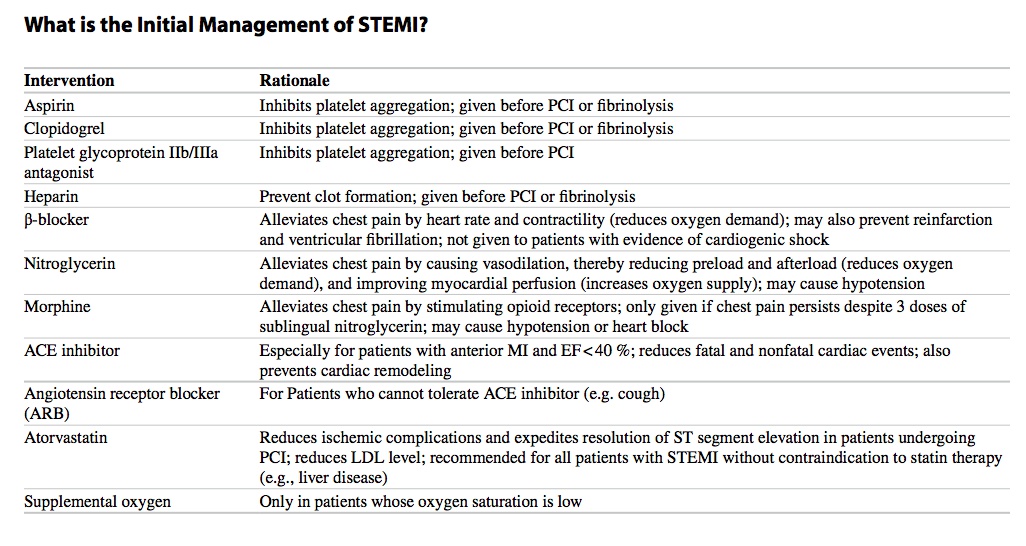
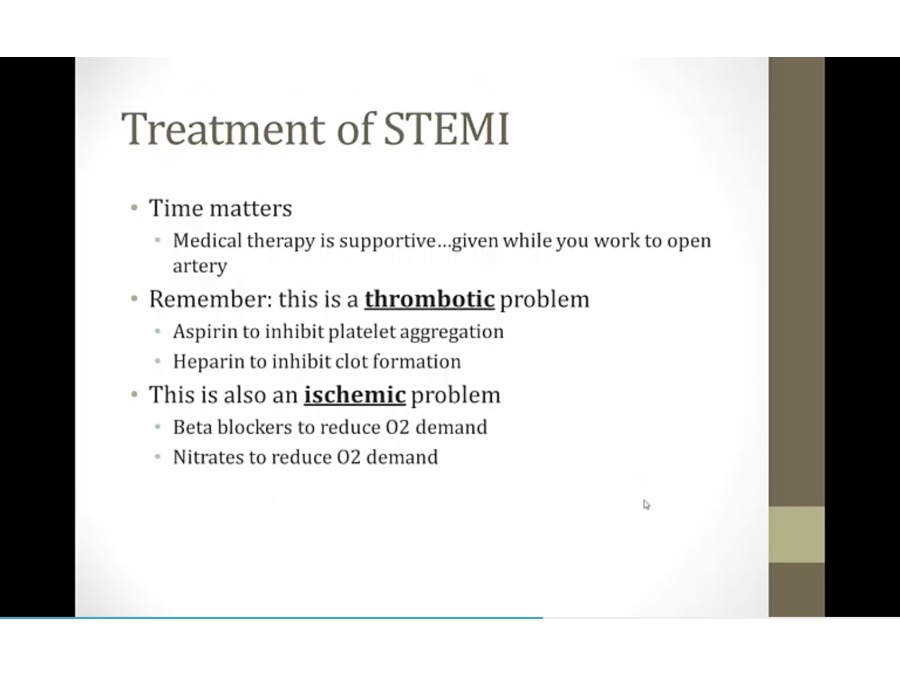
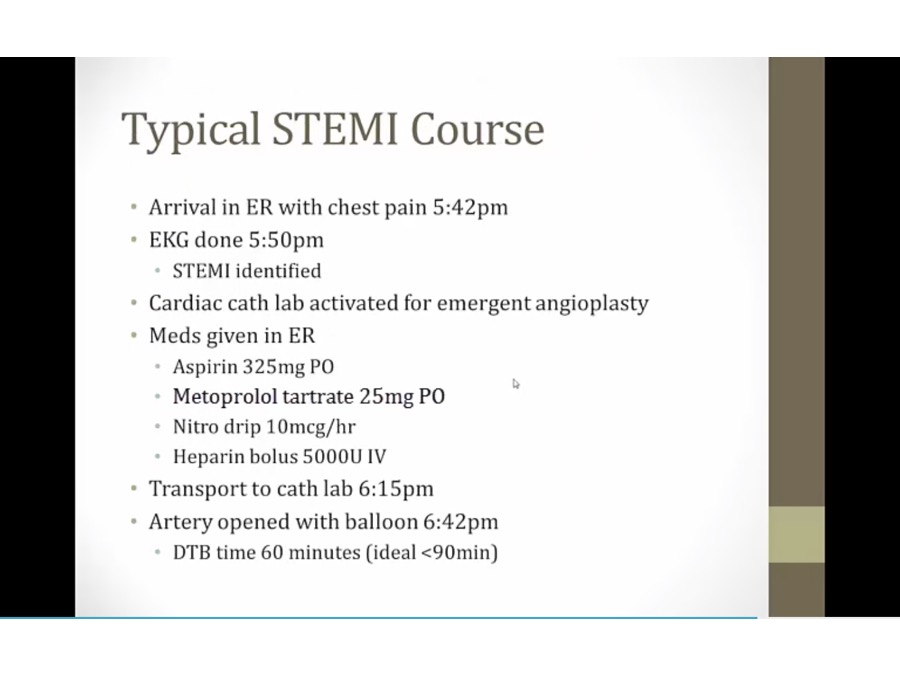
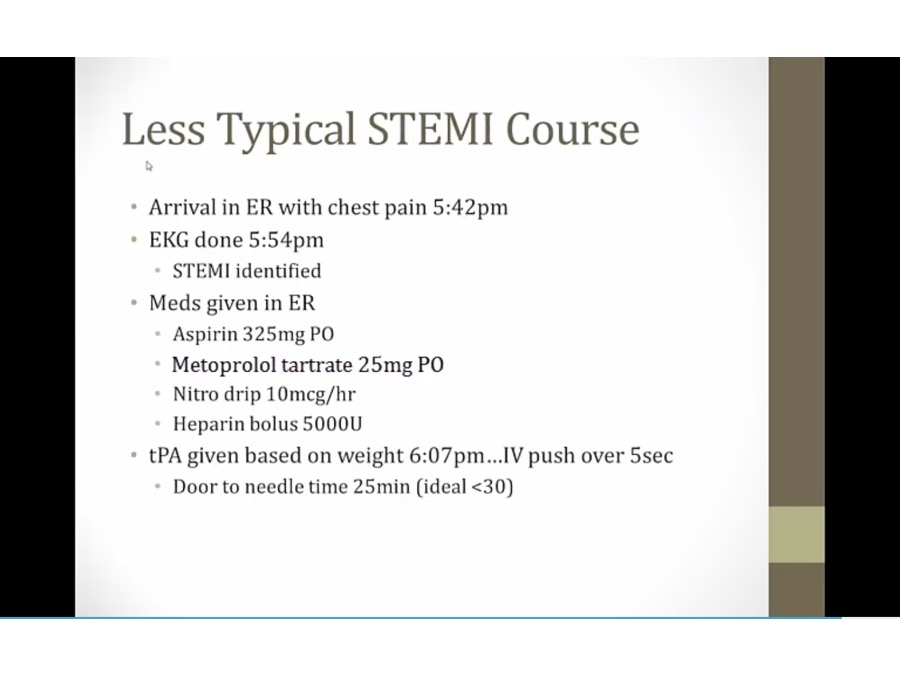
STEMI Treatment
- 1: catheter
- time it takes: door to balloon or needle
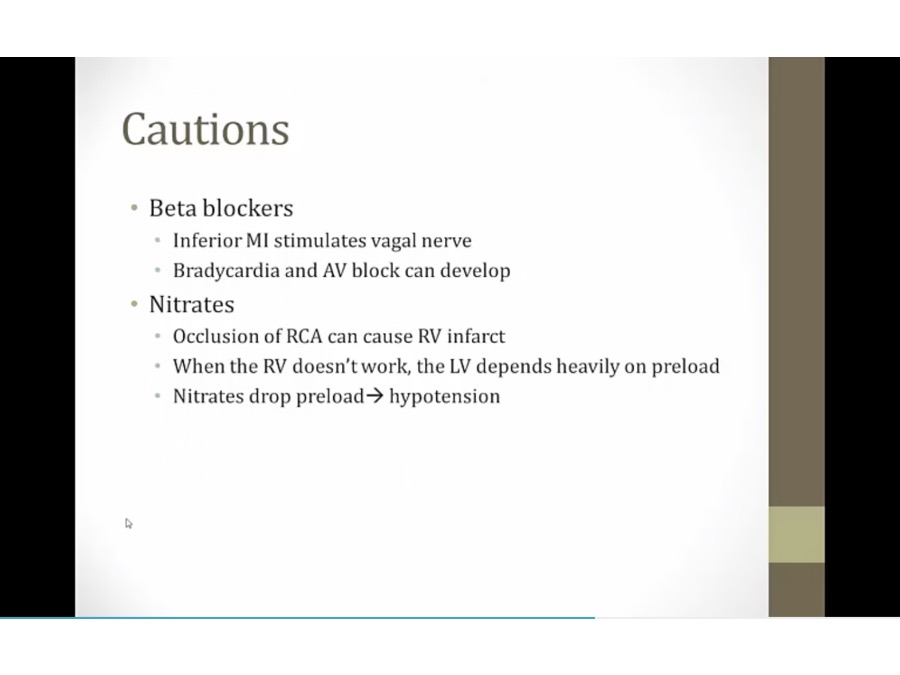
- inferior MI: bradycardia and AV block already from parasympathetic stimulation. Adding beta blocker make it worse
- usually LV infarct, RV sometimes can be infarcted
- hypotension and then cardiac arrest
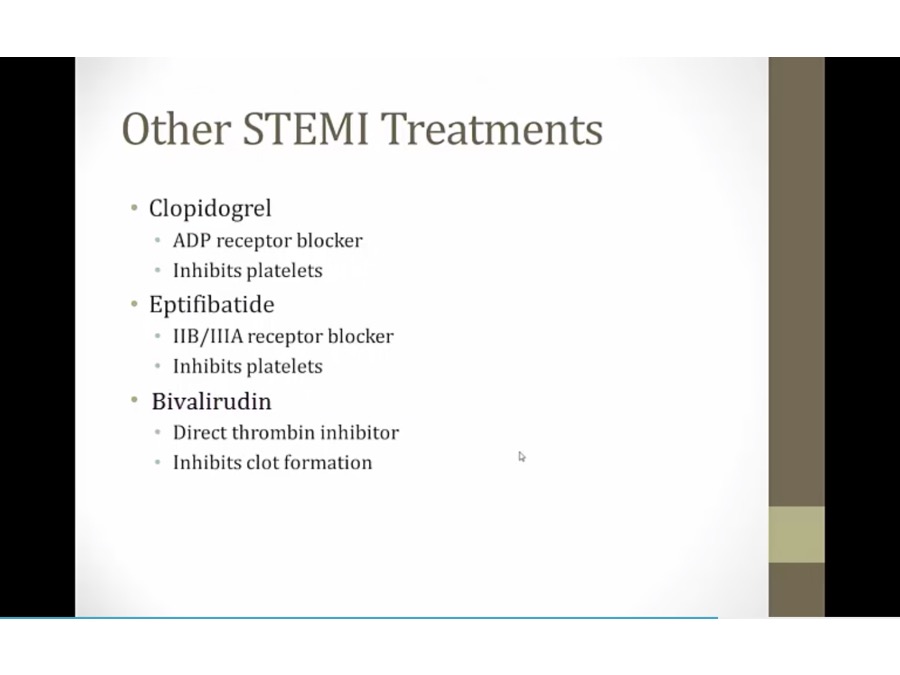

- No intRUDIN: bivaliRUDIN is a direct thrombin inhibitor
- Big GATOR: arGATROban and dabiGATRAN are direct thrombin inhibitors

- ABC sportscaster grabbing fries: abciximab blocks the GP IIb/IIIa receptor preventing platelet aggregation
- Antibody-shaped microphones: abciximab is a monoclonal IgG antibody
- Tied game: eptifibatide and tirofiban block the GP IIb/IIIa receptor to prevent platelet aggregation
- Broken plates: GP IIb/IIIa inhibitors can cause thrombocytopenia
- Ketchup time: antiplatelet therapy increases bleeding time (measure of platelet function)
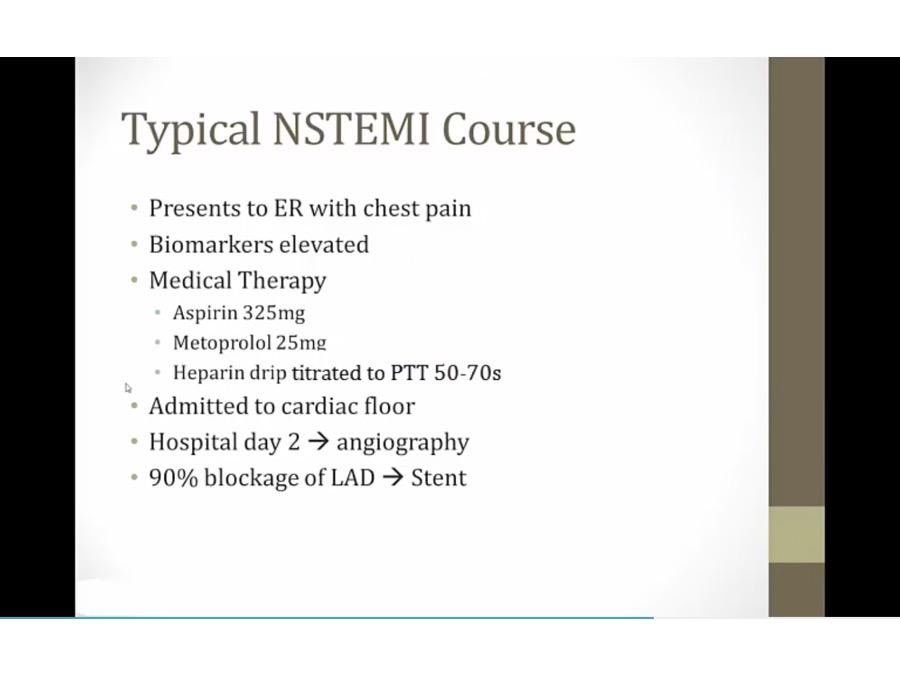
NSTEMI
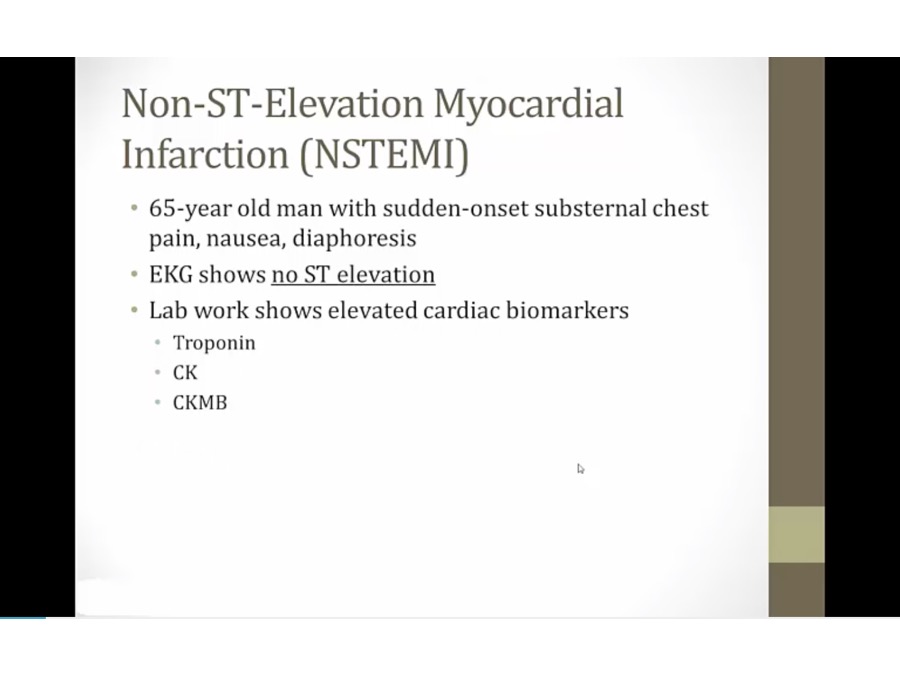
- damage to heart tissues but absence of EKG elevation
- not important
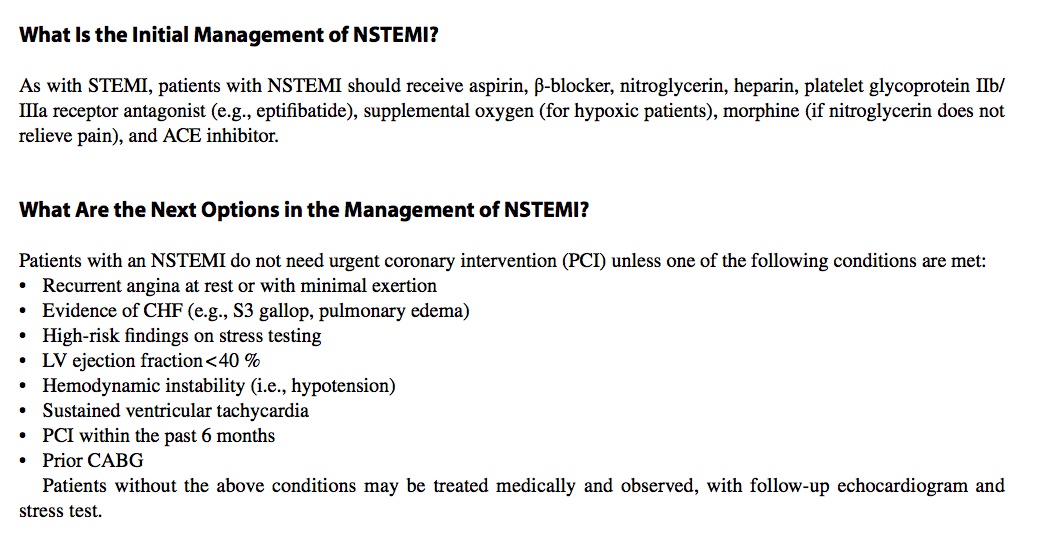
Unstable Angina
- treated just like NSTEMI