12 Thalassemia
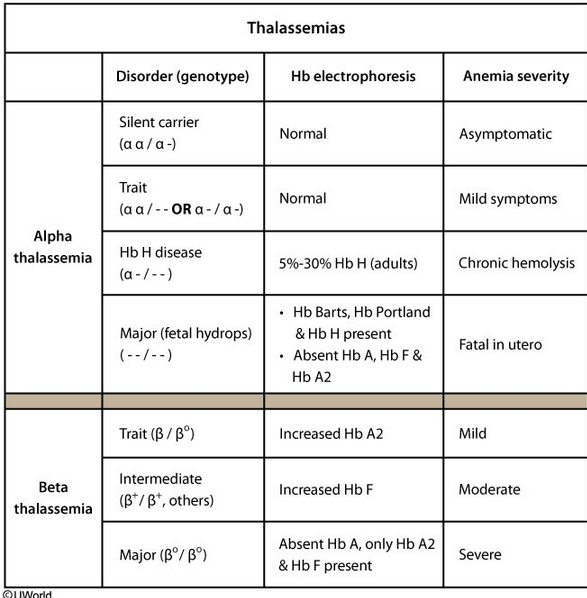
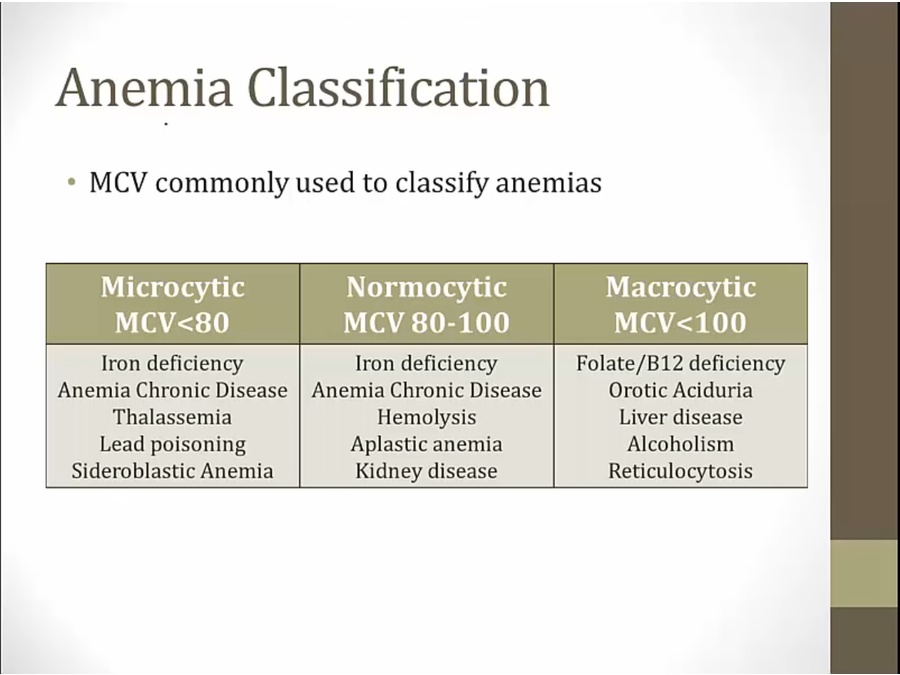
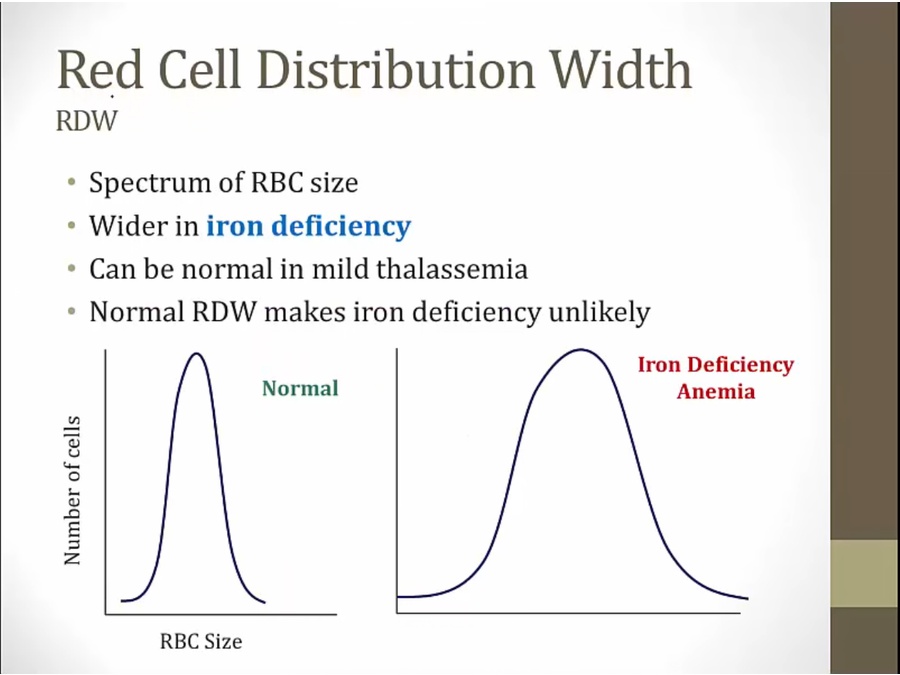
Alphaand beta-thalassemia traits usually have normal to increased total iron and ferritin due to high cell turnover; total iron-binding capacity is normal. Other findings include hematocrit > 30%, microcytic and hypochromic red blood cells (mean corpuscular volume < 75 fL), family history of microcytic anemia, and increased target cells on peripheral smear. In addition, the red cell distribution width (RDW) is normal as all red cells are microcytic and hypochromic.
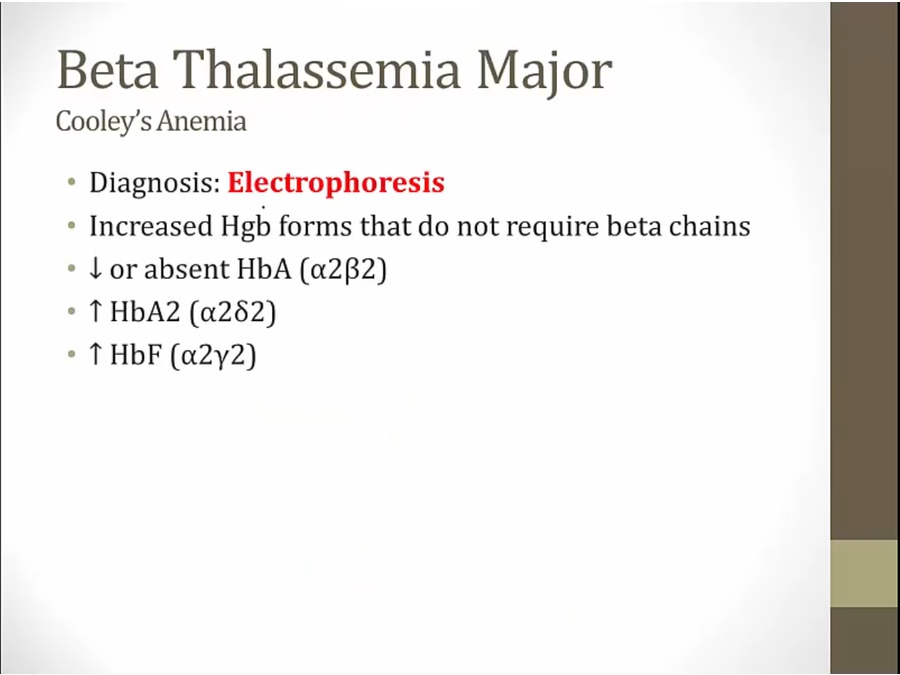
Hemoglobin electrophoresis is generally normal in alpha-thalassemia trait and requires no therapy as patients are generally asymptomatic. Iron supplementation is not required as patients are not iron deficient. Genetic counseling should be offered due to the complex inheritance patterns for thalassemia.
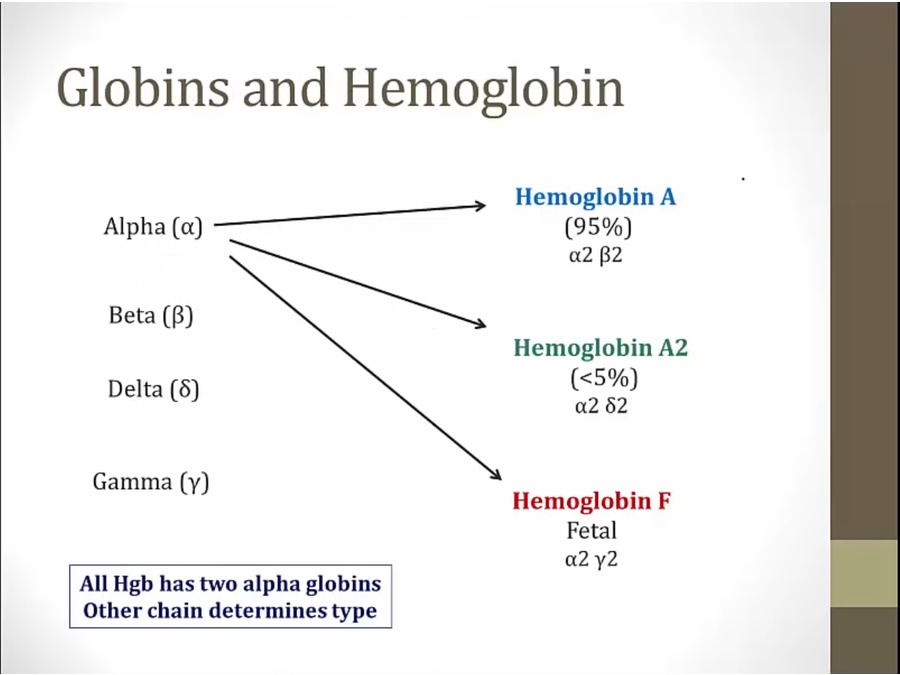
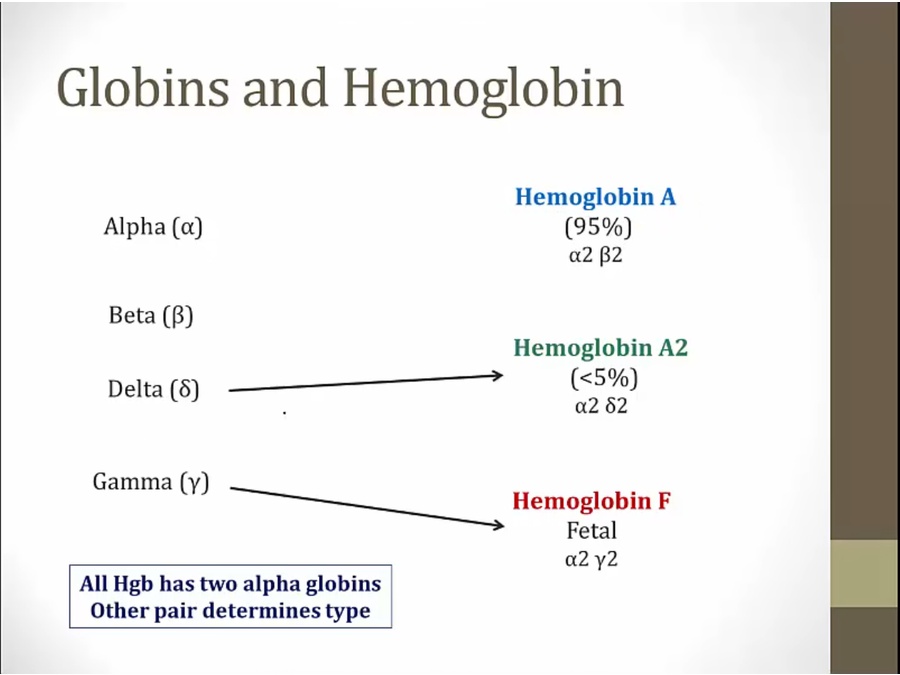
- alpha chain very important: component of all 3 types
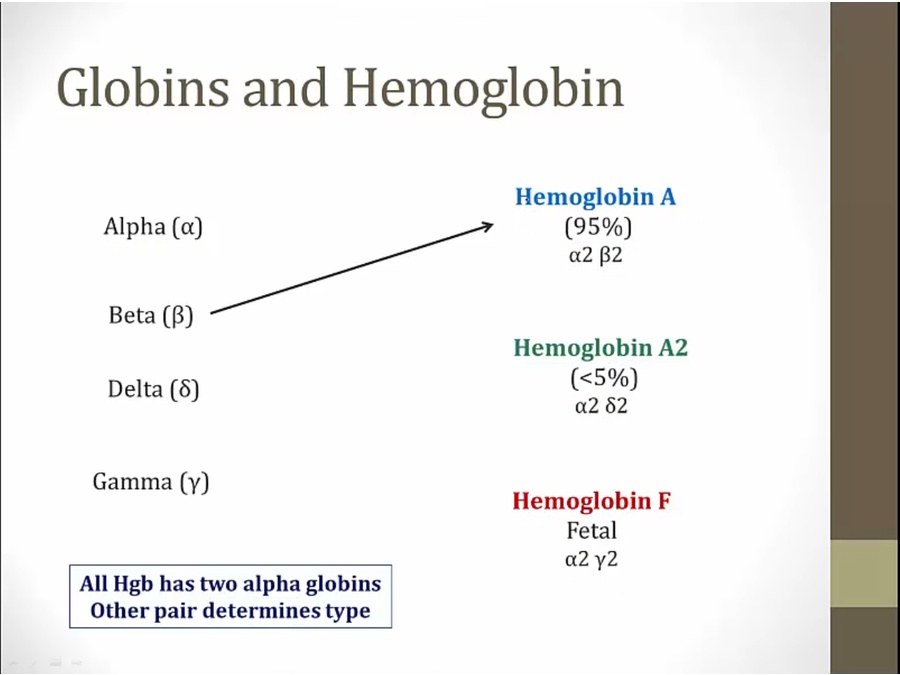
- beta thalassemia only affects A
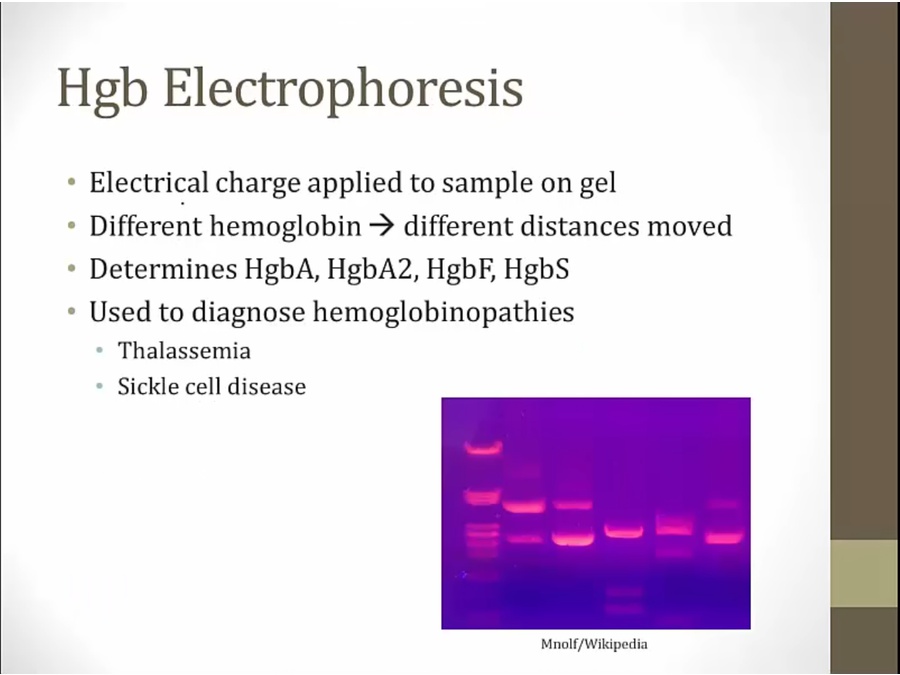
- sample from patient in gel with electrical charge
Thalassemia
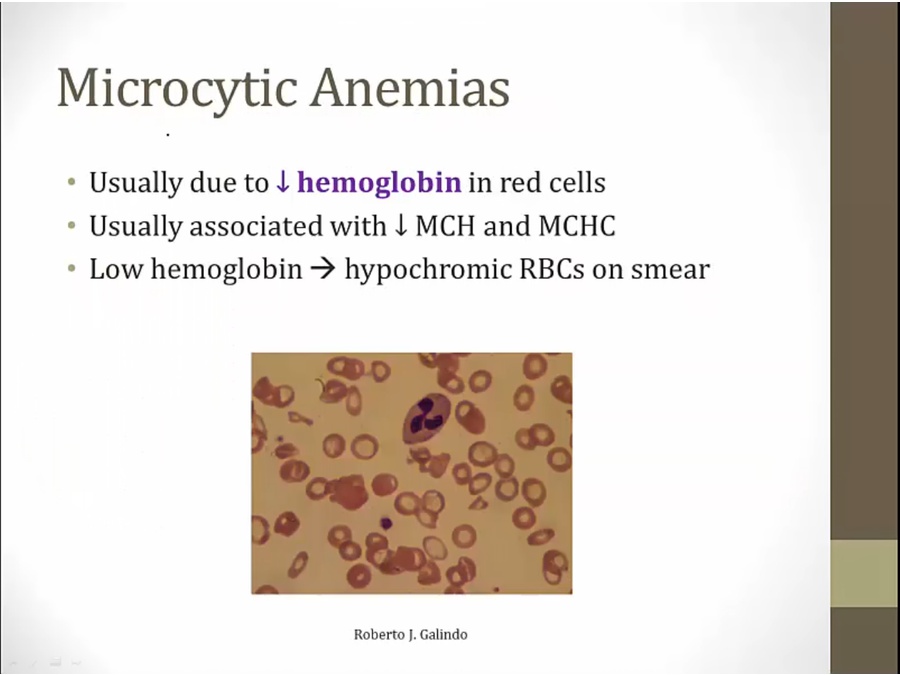
- decreased hemoglobin causes thalassemia
Alpha
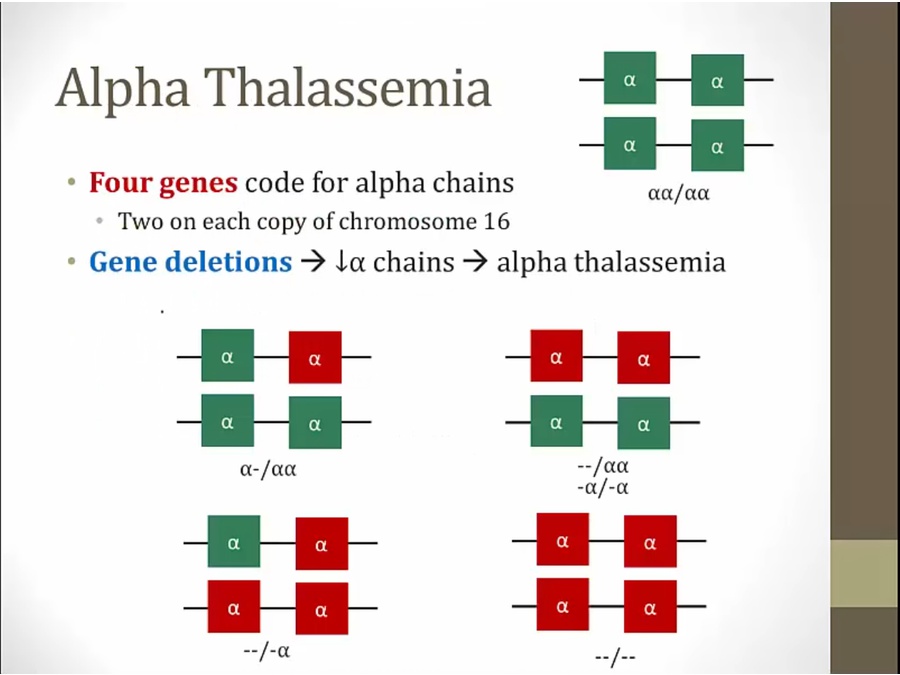
- top right: normal, 2 alpha on each copy of Ch 16
- alpha: gene deletion
- depending on number missing, severity
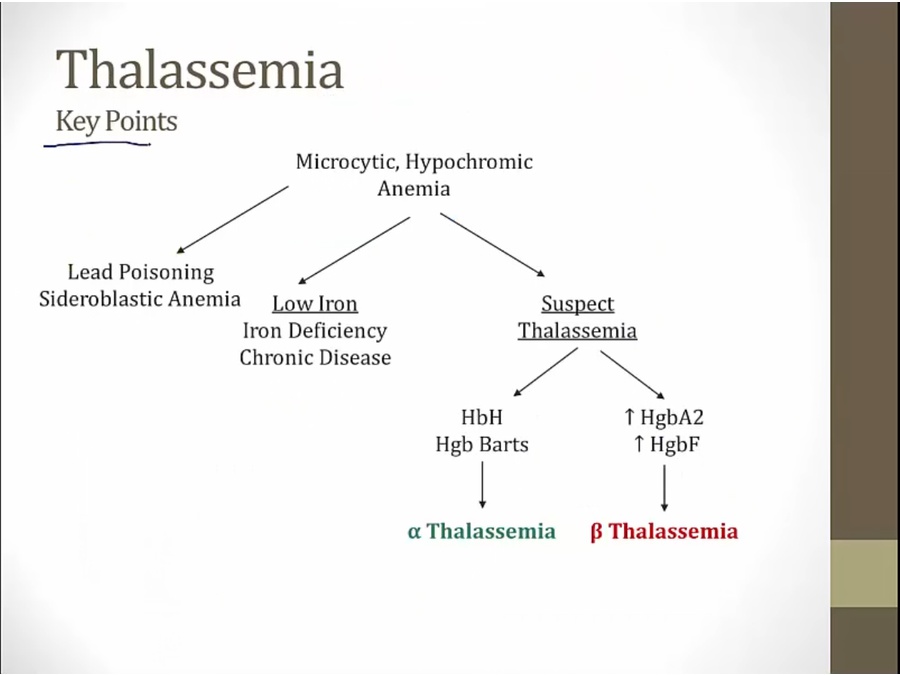
- if not lead poisoning, sideroblastic, or iron, suspect thalassemia
- use electrophoresis to determine alpha or beta
Minima
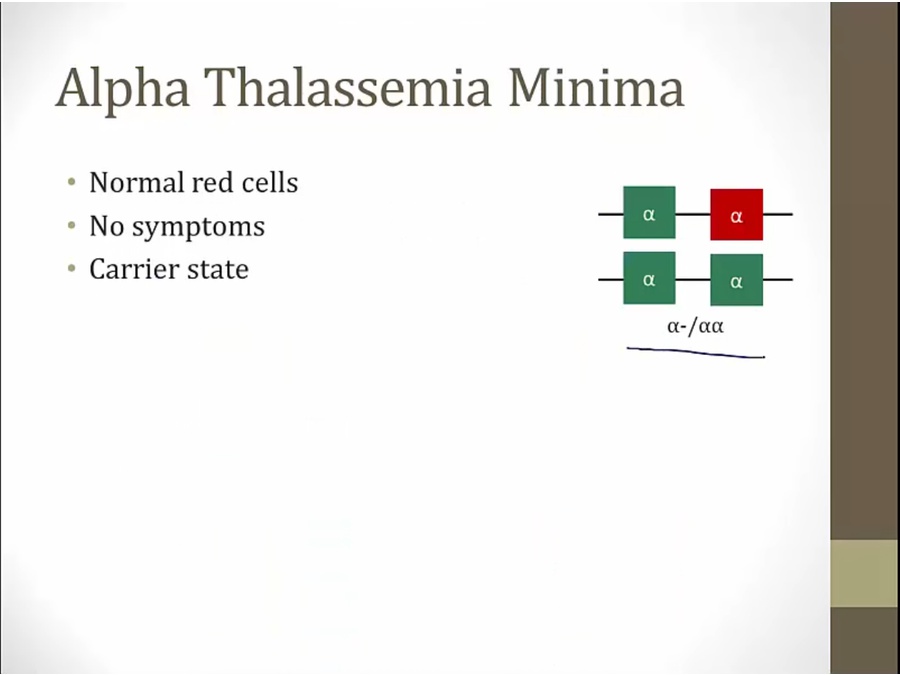
- only risk is pass to offspring
Minor
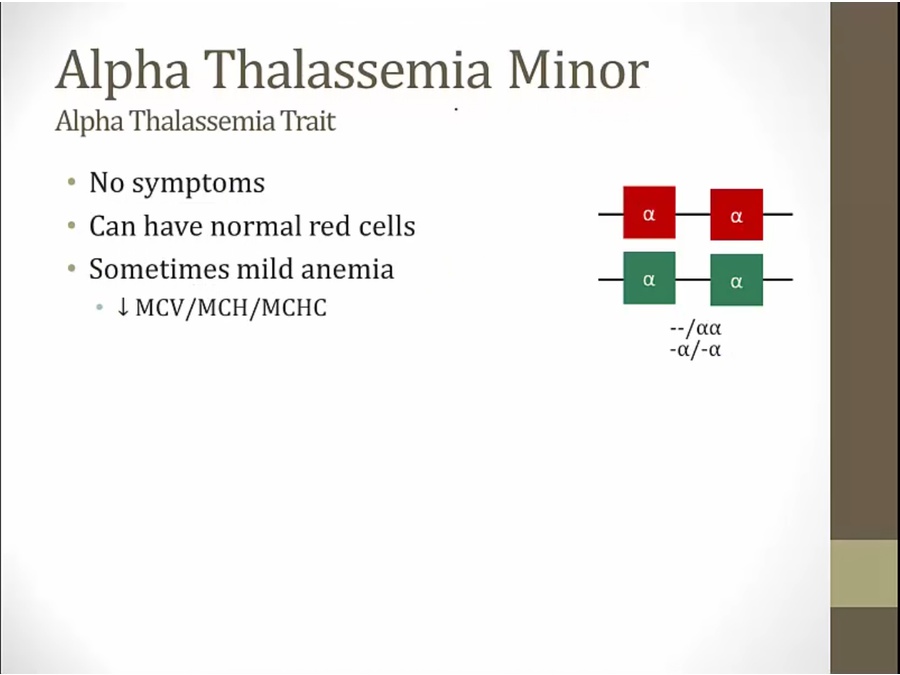
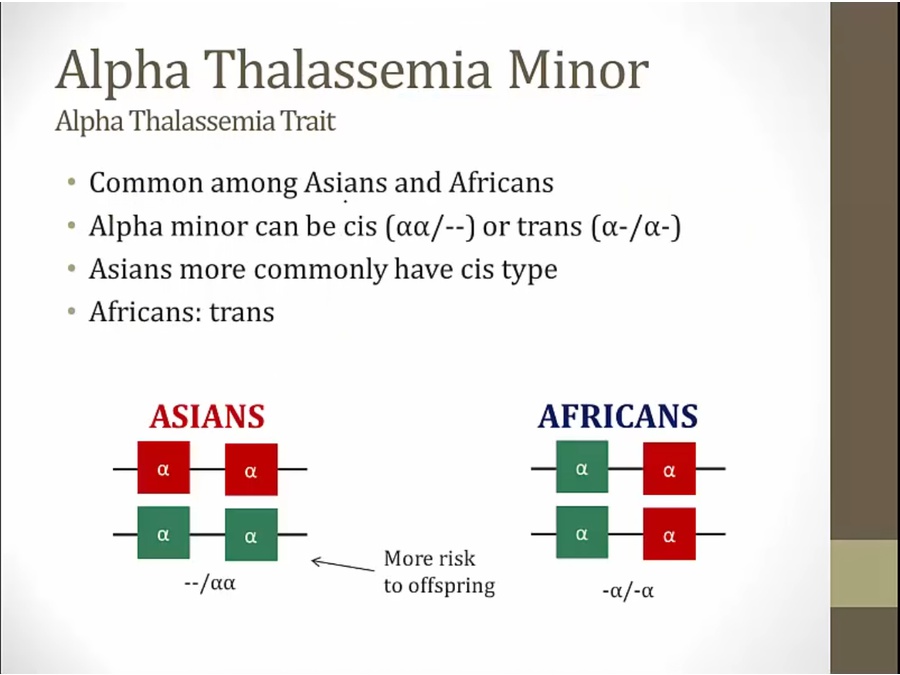
- cis more risk: parent can pass 2 deleted genes to offspring
- trans: can only pass on one deleted gene
HbH Disease
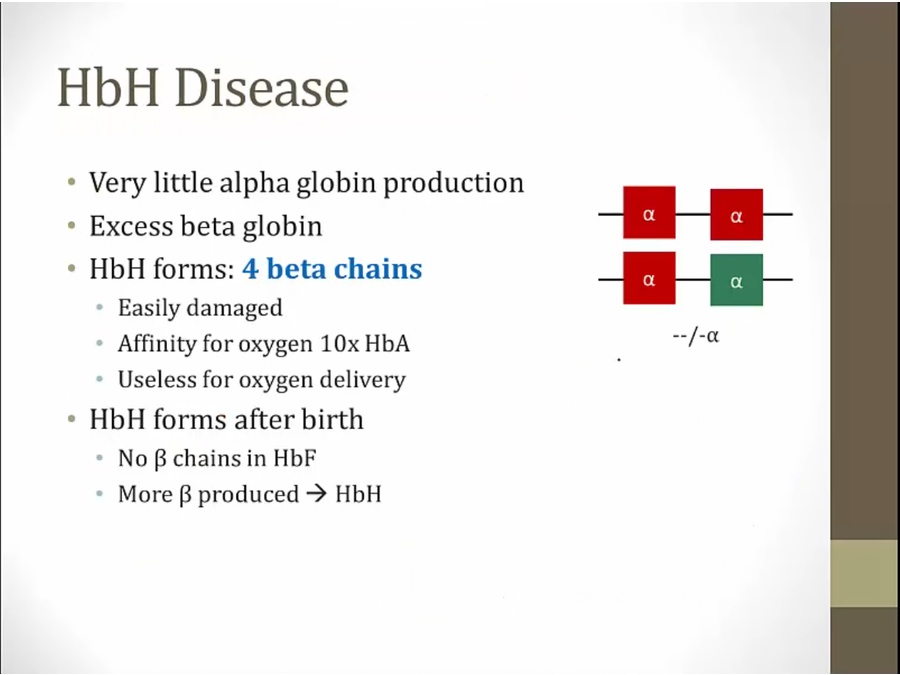
- excess beta globin but can’t combine with alpha globin
- binds O2 but won’t release
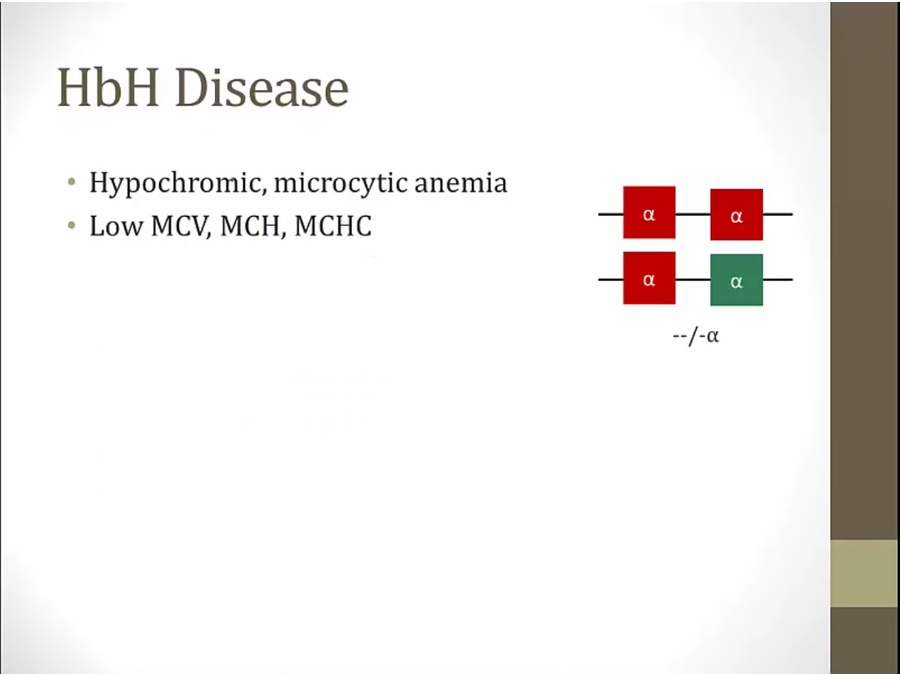
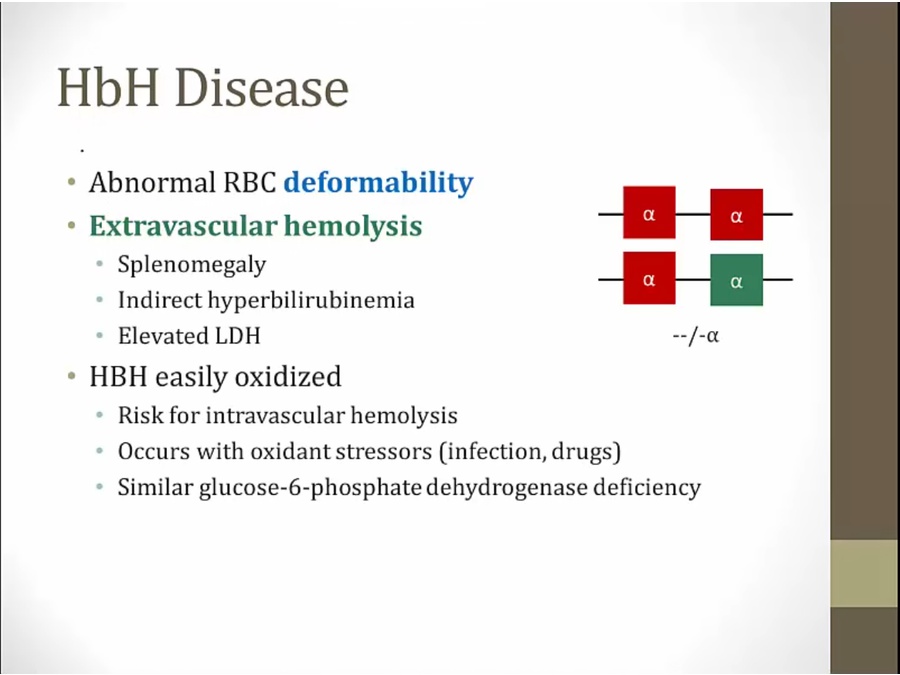
- cleared by spleen
- can look a lot like iron deficiency, but never see hemolysis (high bilirubin, splenomegaly) in iron deficiency
Bart
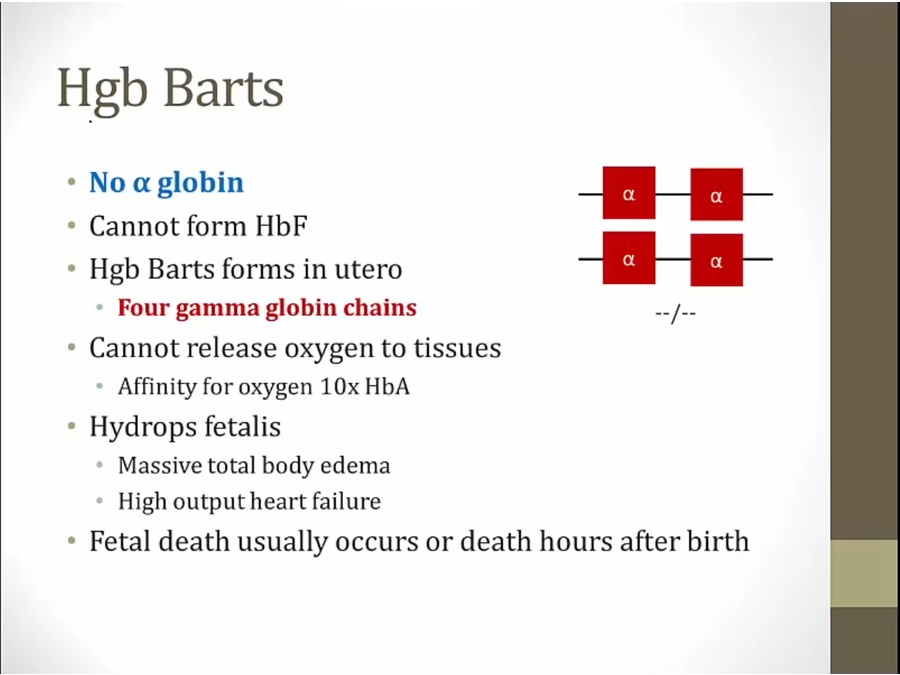
- negative coombs test, compared to erythroblastosis fetalis
Beta
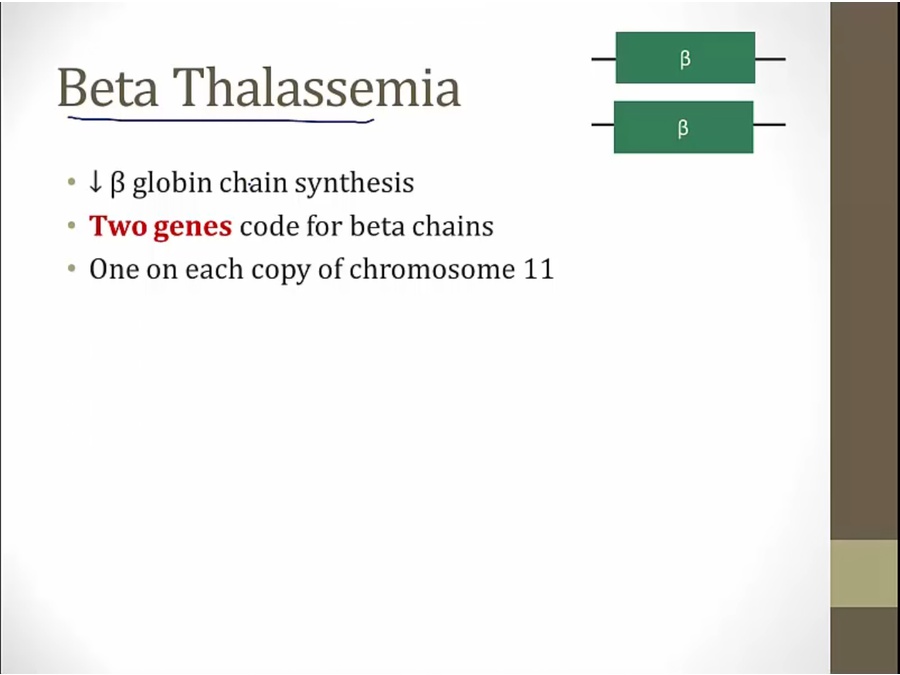
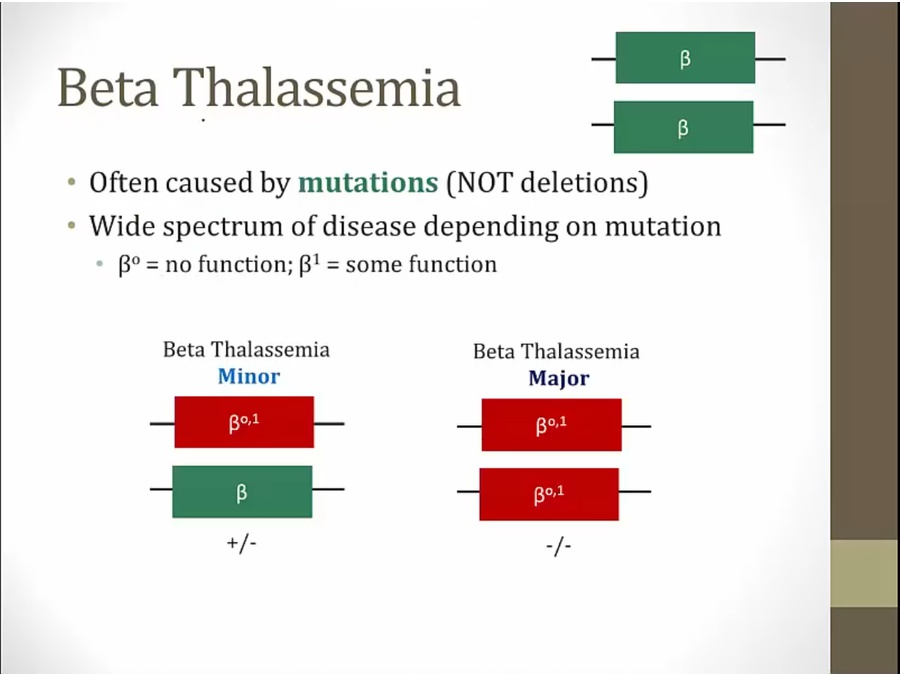
- mutation can result in no function or some function
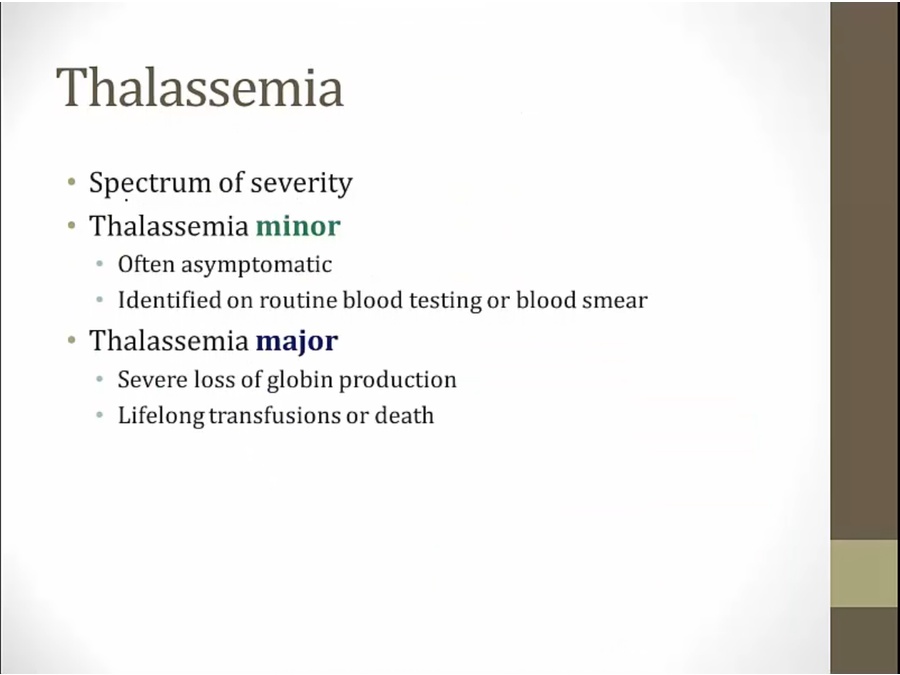
- minor: 1 mutated gene
- major: both genes mutated
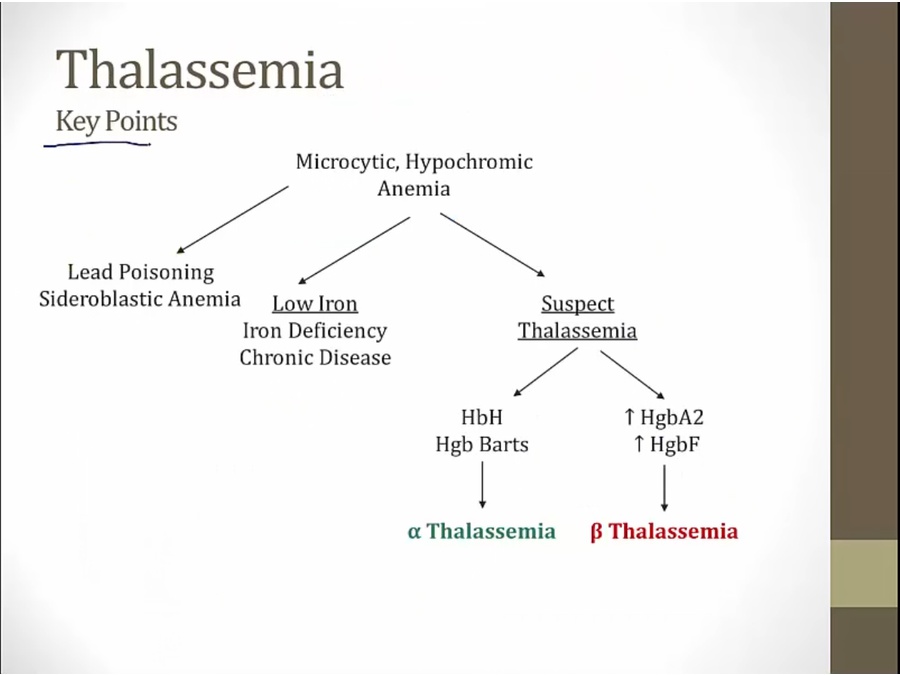
- if not lead poisoning, sideroblastic, or iron, suspect thalassemia
- use electrophoresis to determine alpha or beta

- mediterranean thalassemia
- italy/greece.
Minor
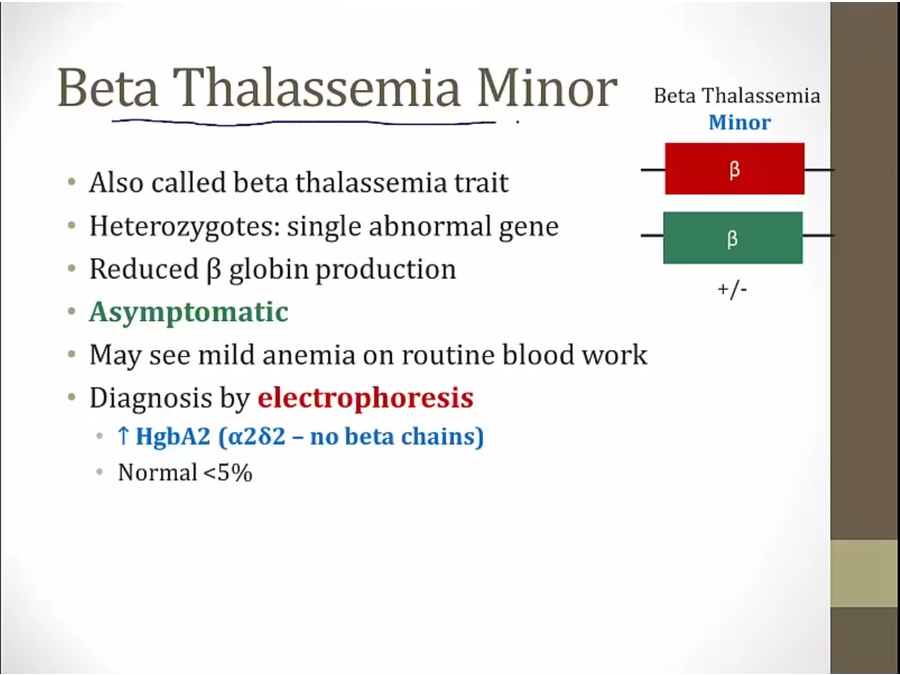
- still makes enough to be asymptomatic
- increased A2 is hallmark of minor
Major
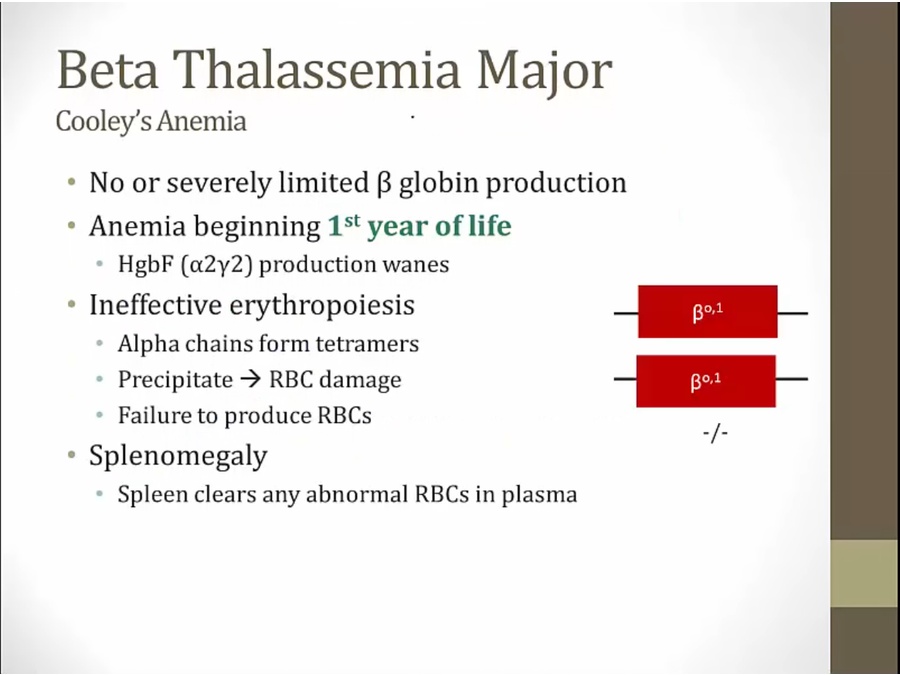
- severe anemia and reduced RBC count
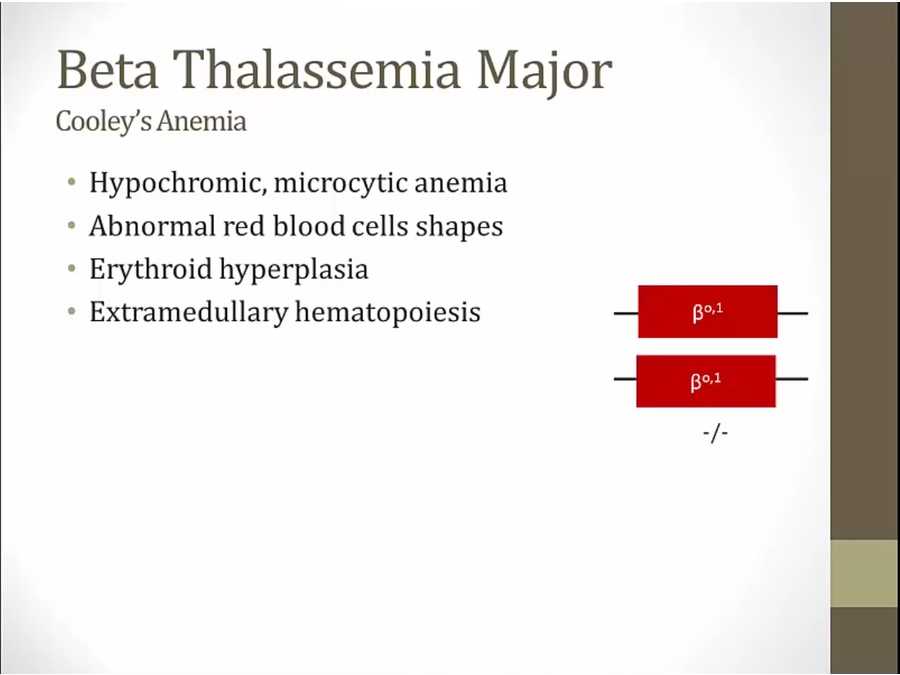
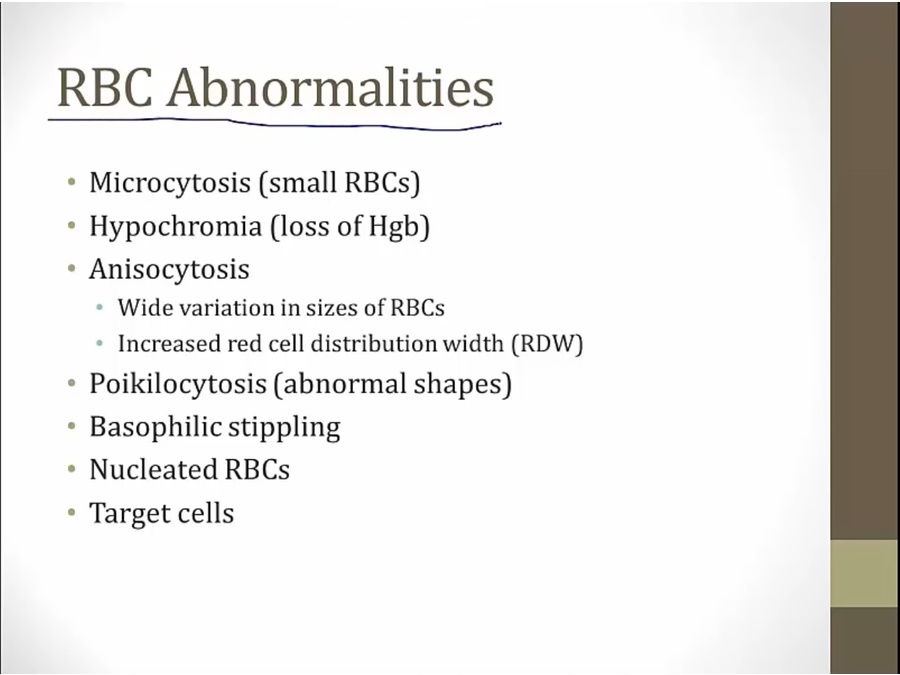
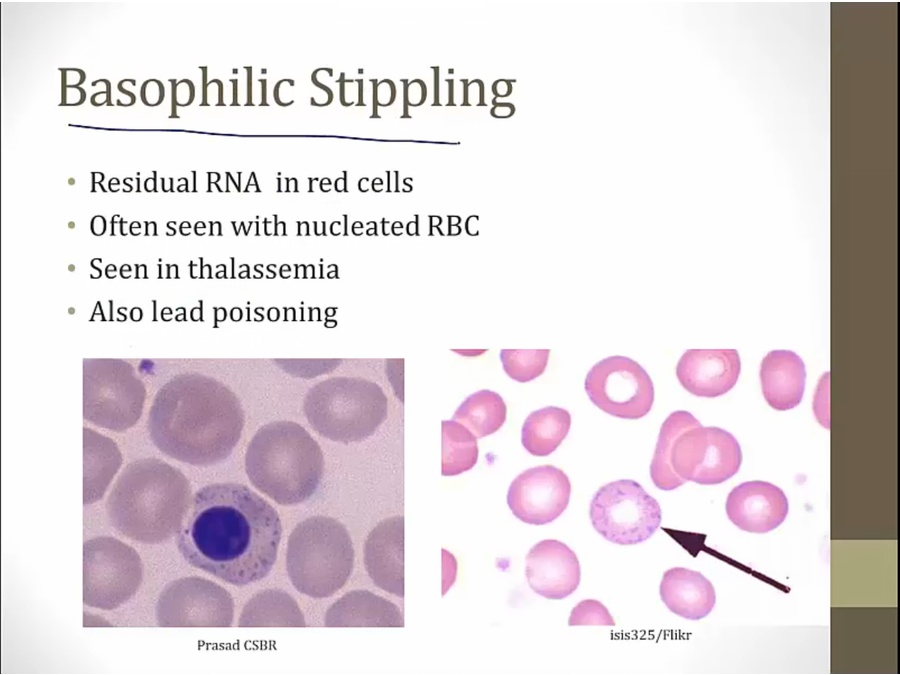
- lots of abnormalities on smear
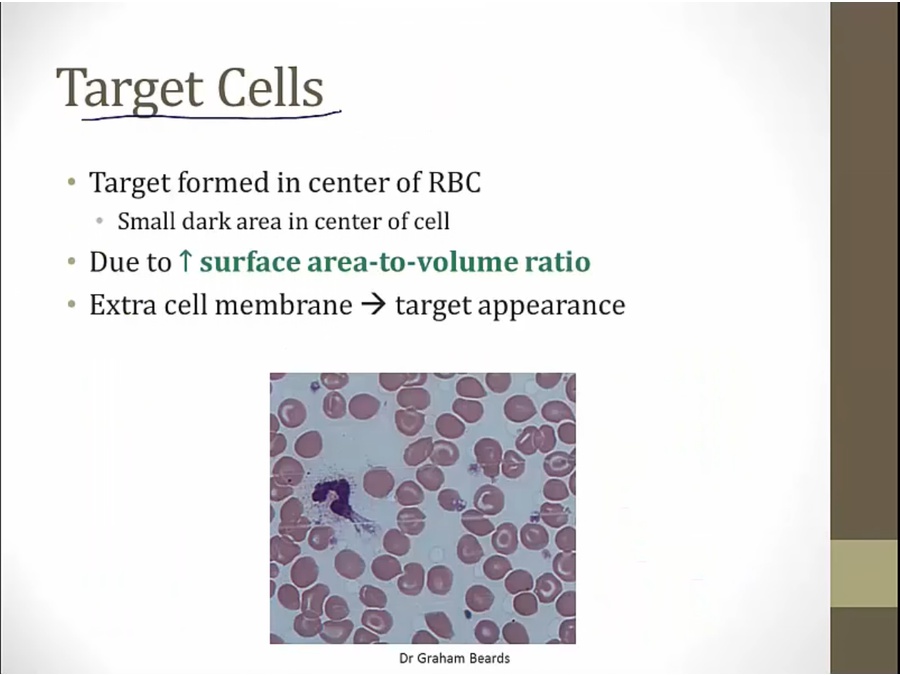
- extra cell membrane or shrink volume
- decreased volume with low Hb
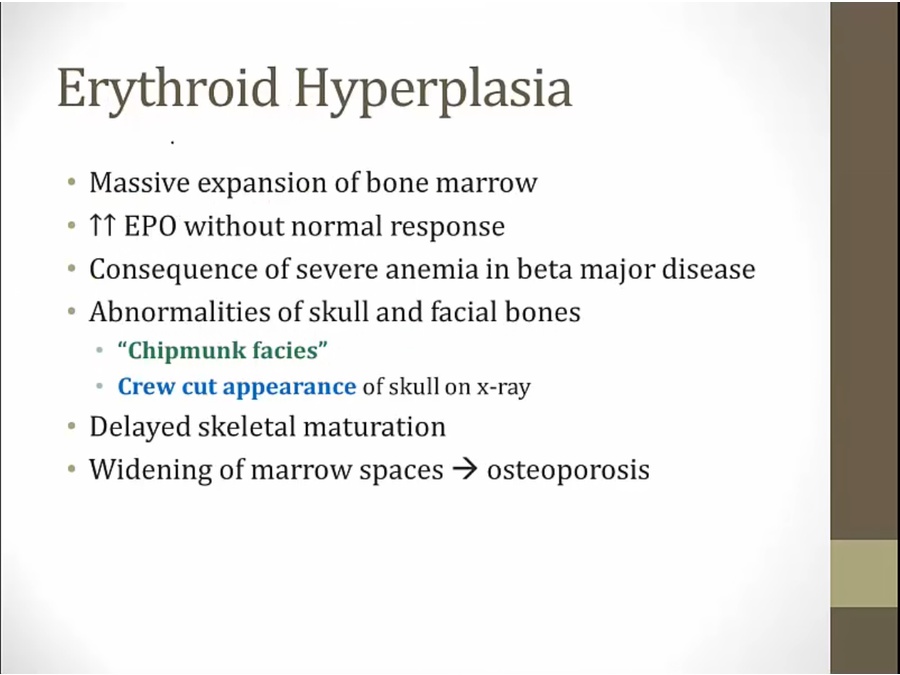
- bone marrow working so hard to make RBC: abnormal skull/face
- crew cut: skull with fine points sticking out of it
- liver/spleen make RBC with very high EPO
Intermedia
- symptoms of anemia but not severe enough to require transfusion
Misc
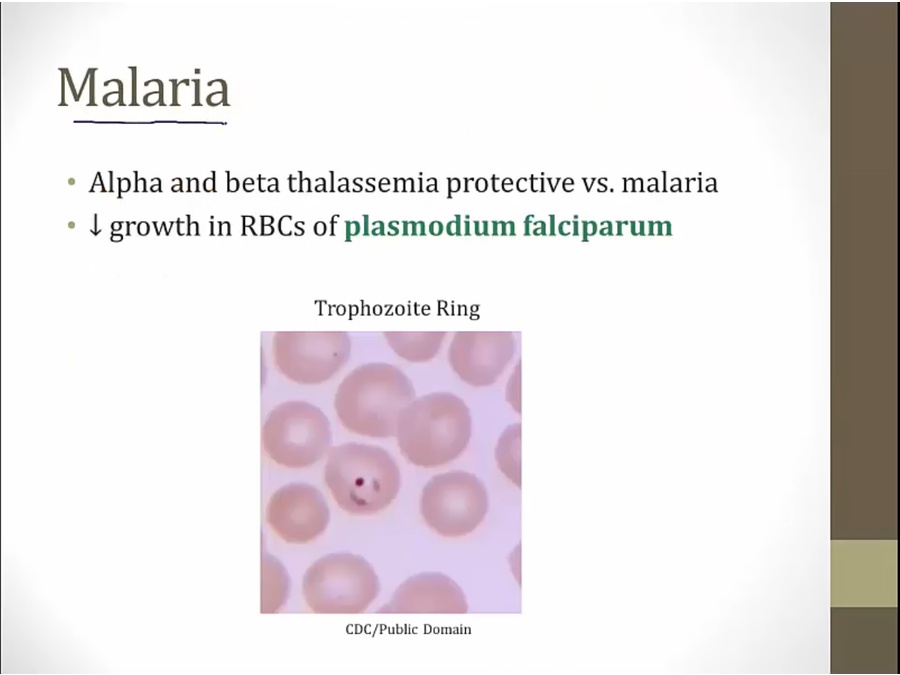
- just as likely to be infected as others, but less severe
- thalassemia: genetic disorder, all RBC affected
- only for mild, not major