14 Parathyroid
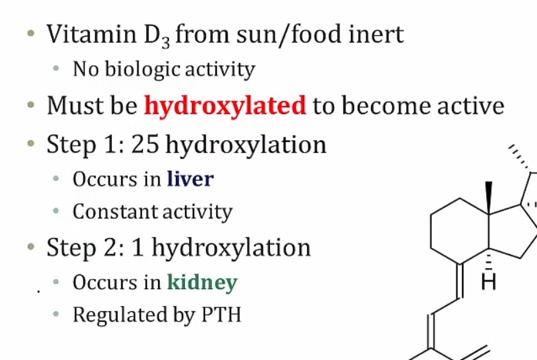
Vitamin D
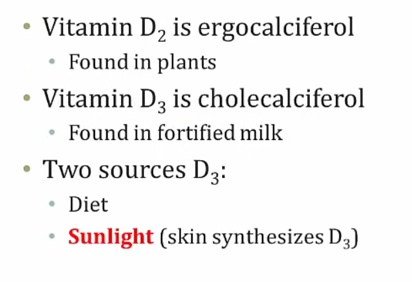
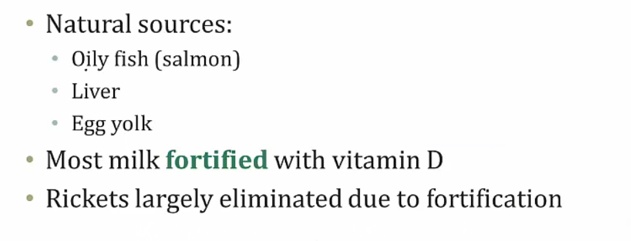
Endogenous vitamin D is produced by photoconversion of 7-dehydrocholesterol to vitamin D3 in sun-exposed skin in the stratum basale (most important source)
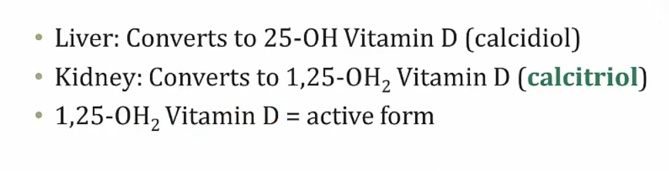
- 25-OH storage form
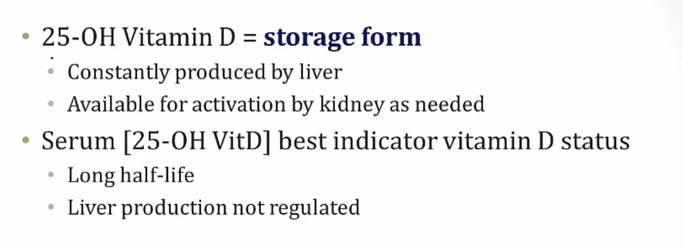
- constant production
- long half life
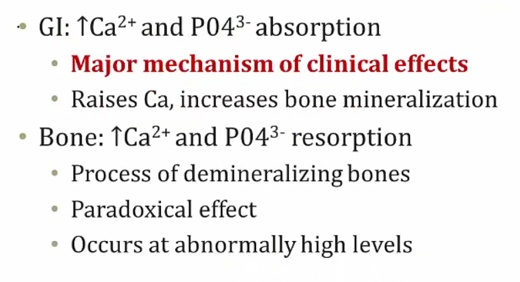
- Mostly increase Ca and bone mineralization (add Ca to bone). At very high levels can cause bone resorption.
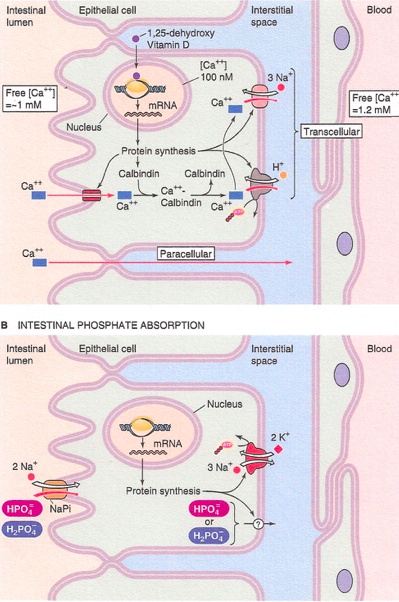
The effects of vitamin D in the intestines include increasing the absorption of Ca 2+ via induction of vitamin-D dependent Ca2+-binding protein (calbindin-D-28K), and increasing the absorption of phosphate by upregulating Na-Pi symporter..
Deficiency
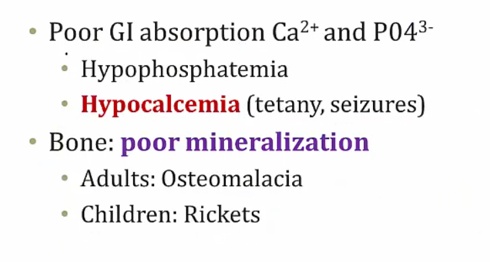
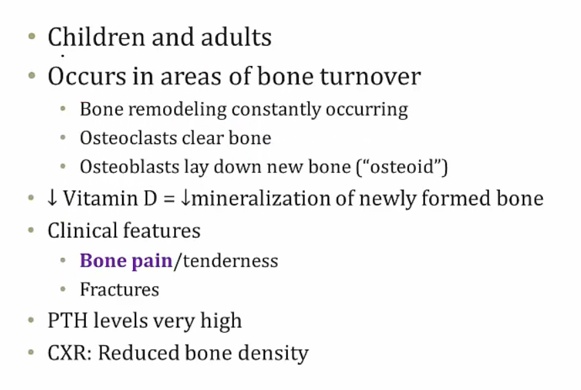
Osteomalacia
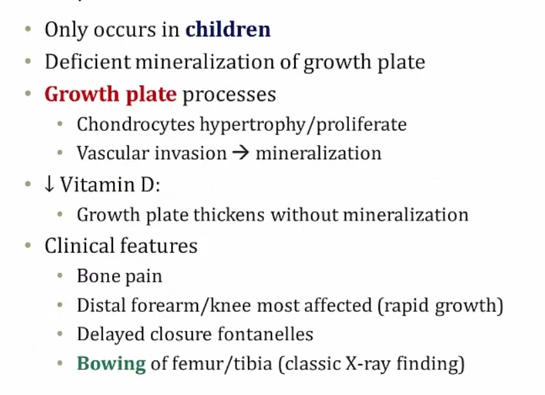
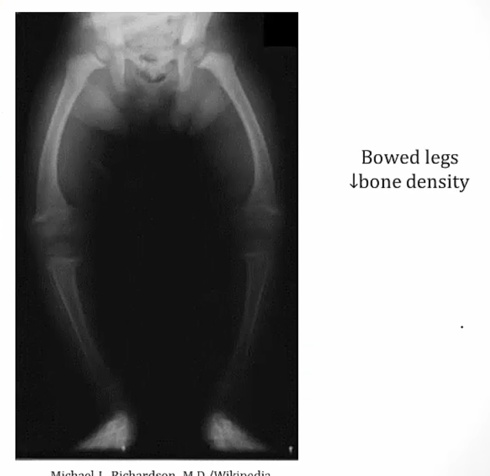
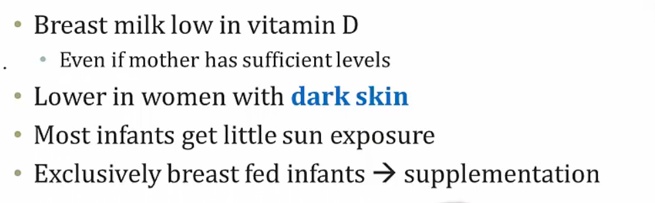
Rickets
Excess
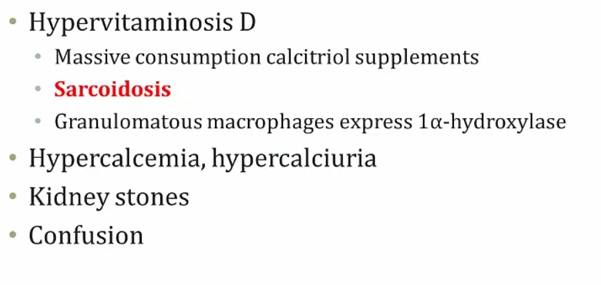
- loss of appetite and stupor (unconsciousness)
Osteoporosis drugs
Bisphosphonates
The first-line treatment for osteoporosis. They induce apoptosis and inhibit differentiation and activity in osteoclasts (block osteoclast binding and the formation of the osteoclastic ruffled border). Bisphosphonates also appear to bind to the hydroxyapatite of the bone, stabilizing it against recognition by the osteoclasts.
Examples include the “-dronate” drugs:
- Medronate
- Clodronate
- Alendronate.
Uses:
- Osteoporosis
- Hypercalcemia
- Bone malignancy
- Paget disease of the bone.
SE include:
- Esophagitis (patients are advised to take with water and remain upright for 30 minutes)
- Dysphagia
- Gastric ulcers
- Osteonecrosis of the jaw.
SERMS
selective estrogen receptor modulators.
Have tissue specific effects. In some tissues they behave as estrogen agonists whereas in other tissues they behave as estrogen antagonists.
Include tamoxifen and raloxifene.
Raloxifene
Inhibits bone resorption by acting as an estrogen agonist in the bone. It can be successfully combined with bisphosphonates to prevent osteoporosis in postmenopausal women.
Iinhibits bone resorption in postmenopausal women by inhibiting osteoclasts. However because of the increased risk of endometrial hyperplasia and cancer, is NOT considered a first-line SERM for the treatment of osteoporosis.
Some common side effects include:
- Edema
- Hot flashes
- Arthralgias
Note that both cause decreased bone density in premenopausal women, so they should NOT be used to treat or prevent osteoporosis in this population.
Serious adverse effects include:
- Venous thromboembolism
- Fatal stroke in patients with cardiovascular disease
- Endometrial cancer.
Teriparatide
Has been shown to increase bone density and bone mass.
In postmenopausal women, decreases osteoporosis-related fractures.
Should not be used in patients with previous bone radiation or other predispositions to osteosarcoma.
Denosumab
A human monoclonal anti-RANKL antibody used for the treatment of:
- Osteoporosis
- Treatment-induced bone loss
- Bone metastases
- Multiple myeloma
- Giant cell tumor of bone.
Adverse effects include:
- Joint and muscle pain in the arms or legs
- Increased risk of infection
- Hypocalcemia
- Osteonecrosis of the jaw
- Atypical hip fractures (from too little bone turn over).
Calcium
Plasma Ca2+ exists in three forms:
- Free ionized (45%)
- Bound to albumin (40%)
- Bound to anions (15%)
Free, ionized Ca2+ is biologically active.
Ionized calcium binds to negatively charged sites on protein molecules, competing with hydrogen ions for the same binding sites on albumin and other calcium-binding proteins.
This binding is pH dependent and alters the level of ionized calcium in the blood. An increase in pH, alkalosis, promotes increased protein binding (less H+ competing), which decreases free calcium levels. Acidosis, on the other hand, decreases protein binding, resulting in increased free calcium levels..
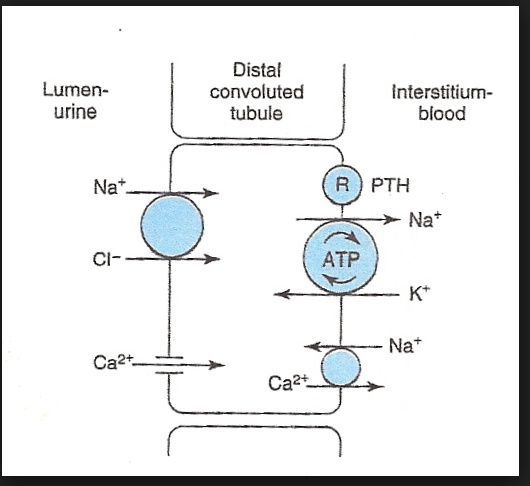
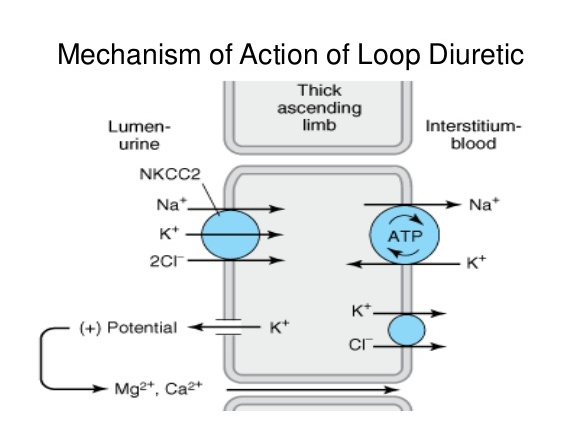
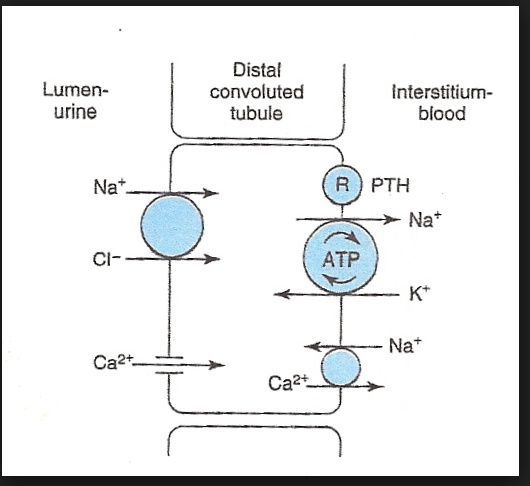
Diuretics can alter calcium levels. Loop diuretics decrease calcium reabsorption in the thick ascending limb of the nephron, while thiazides increase its reabsorption in the distal convoluted tubule. To remember this difference, use the mnemonic “The loop loses calcium”
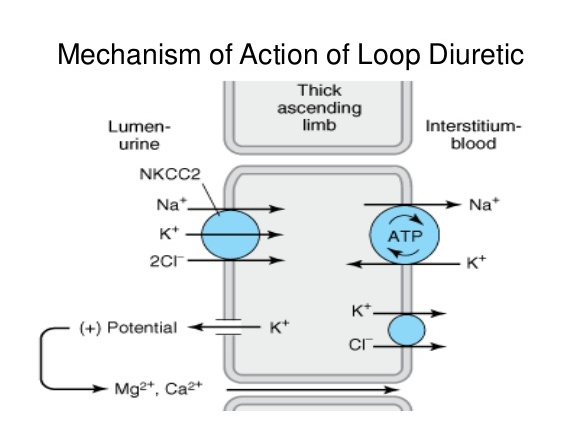
Active reabsorption by the Na+/K+/2Clcotransporter leads to a backleak of K+. The positive lumen potential created by this backleak will induce paracellular reabsorption of Mg2+ and Ca2+. Blocking the Na+/K+/2Clcotransporter with a loop diuretic will decrease calcium reabsorption into the blood.
Thiazide diuretics block the apical Na+/Clsymporter, and as a result intracellular sodium is reduced. This ramps up the activity of the basolateral Ca2+/Na+ exchanger (to increase Na+ pumped into the tubular cell), which will increase calcium reabsorption into the blood.
Cinacalcet
Increases the sensitivity of the Ca2+-sensing receptor (CaSR) in the parathyroid gland to circulating Ca2+. This decreases the secretion of parathyroid hormone.
Is indicated in the treatment of:
- Hypercalcemia due to primary hyperparathyroidism (e.g. parathyroid carcinoma)
- Secondary hyperparathyroidism in chronic kidney disease patients
Cinacalcet may cause hypocalcemia.
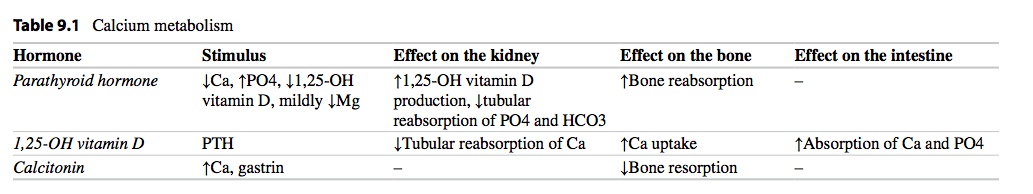
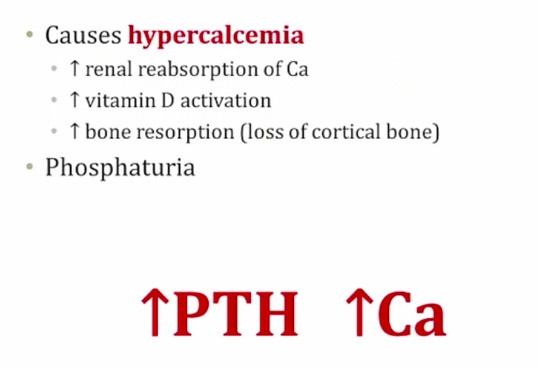
PTH

- Soluble in water.
Effects
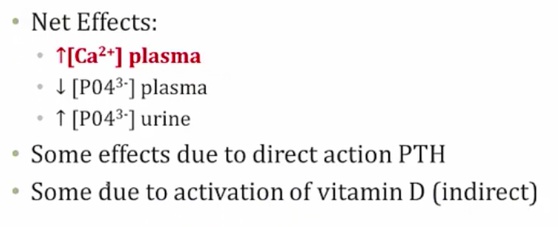
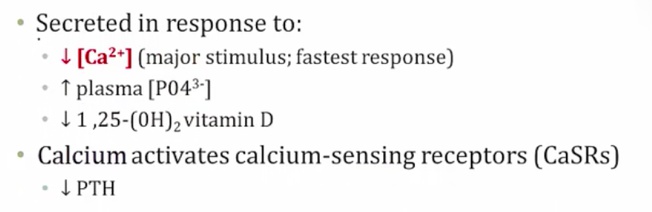
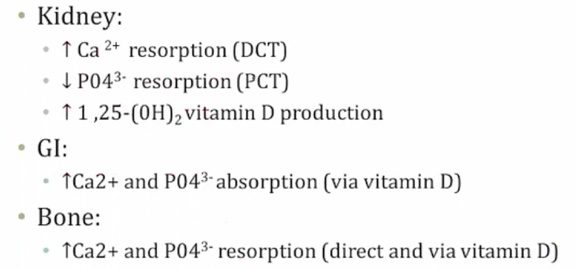
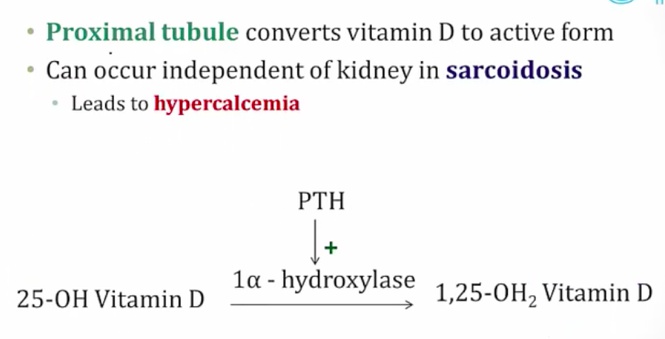
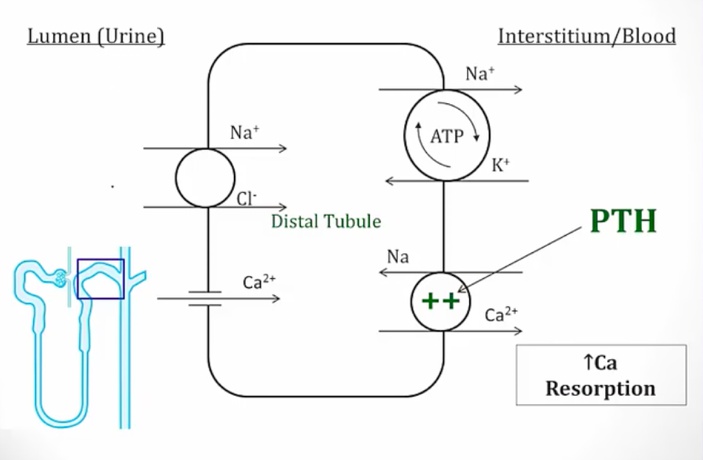
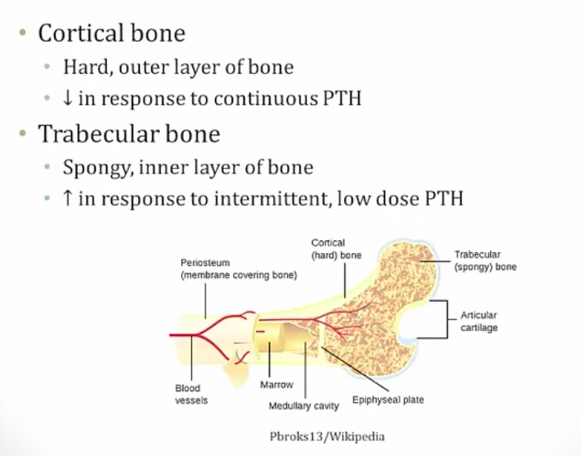
- 1, 25 OH2 Vit D is active form
- Overall effect: decreased phosphate in serum
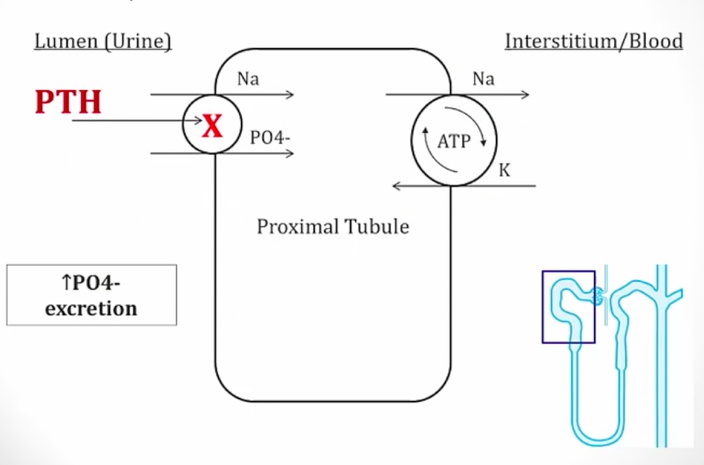
- Decreased phosphate in serum
- Increased phosphate secretion
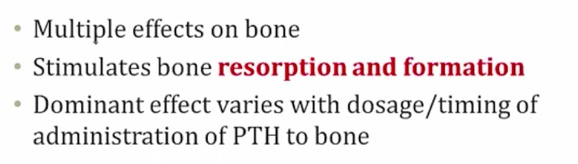
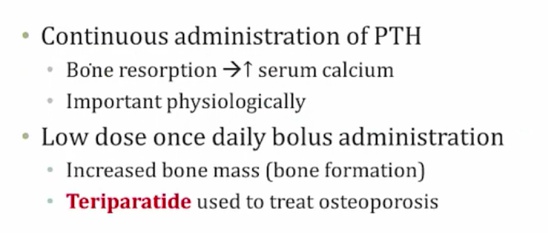
Parathyroid analog used to treat osteoporosis.
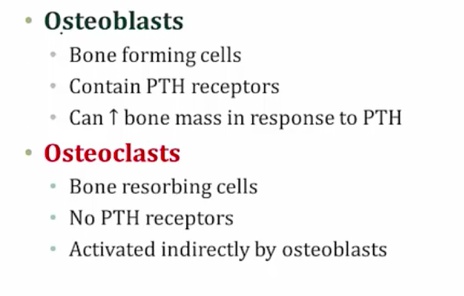
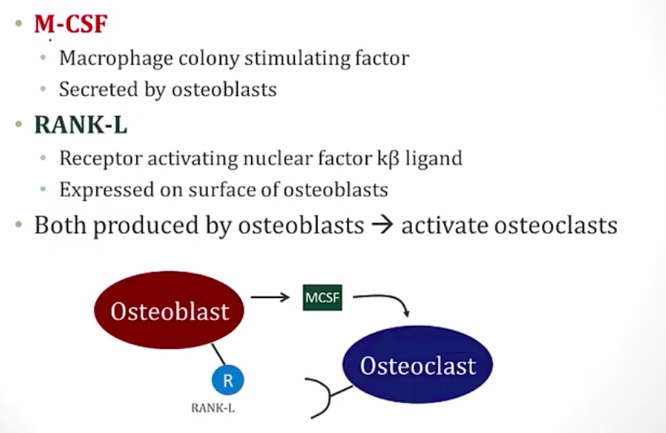
- OPG is secreted by osteoblast. It’s a soluble RANk that inactivates RANK-L
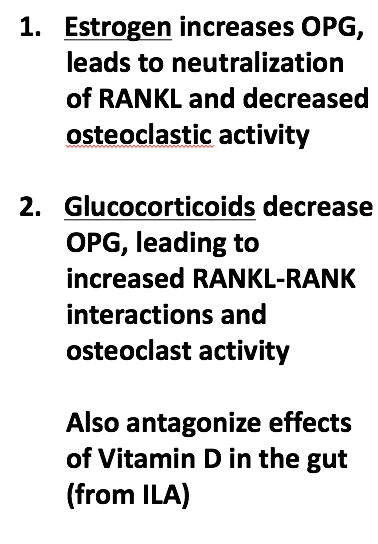
- pregnancy: increased estrogen and bone density
- stress: increased glucocorticoids and decreased bone density
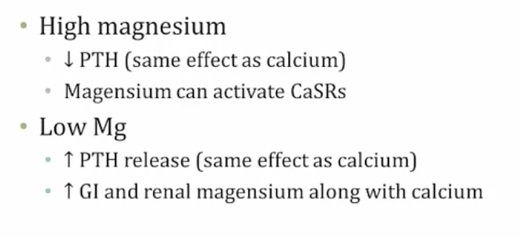
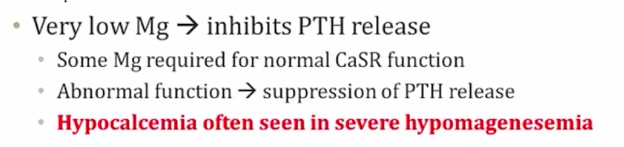
- Low Mg leads to increased GI/renal absorption
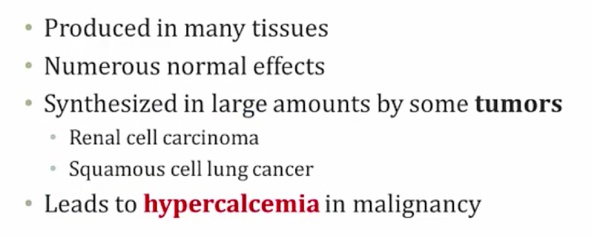
PTHrp
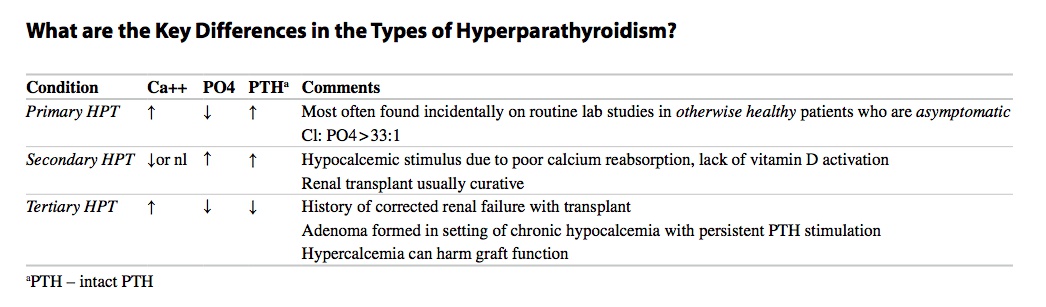
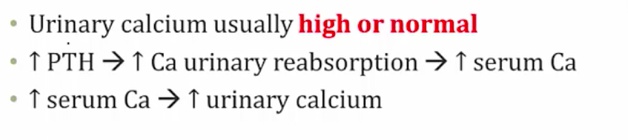
Hyperparathyroidism
Primary Hyperparathyroidism
Cause:
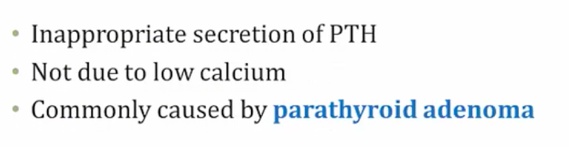
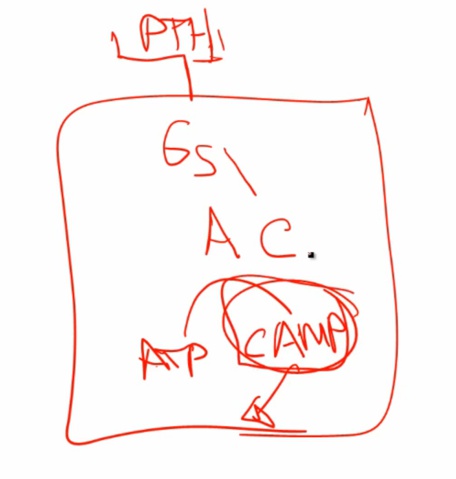
- Increased cAMP
- Increased Alk Phos: alkaline environment needed to lay down Ca in bone. Increased osteoblast > increased laying down bone and produce alk phos (sign of osteoblast activity)
Symptoms:
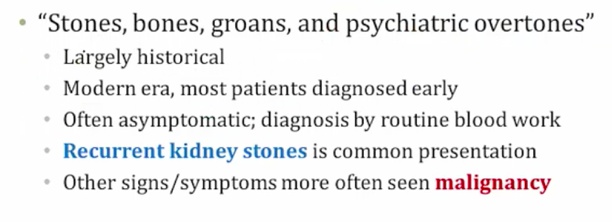
- malignancy: symptoms happens earlier
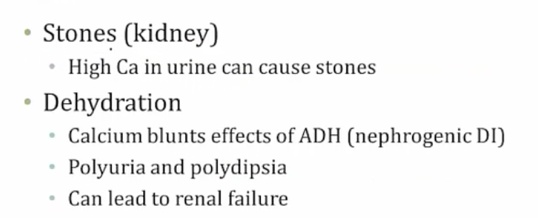
- metastatic calcification of renal tubules
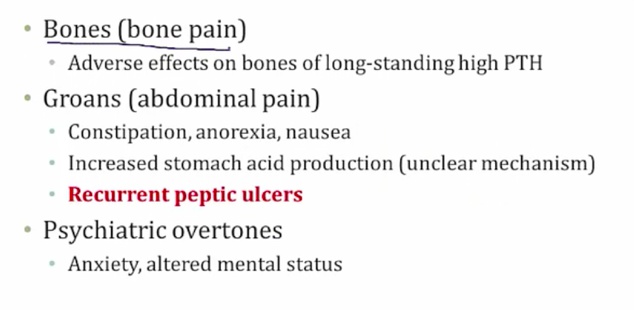
- classic: pancreatitis
- nephrocalcinosis:
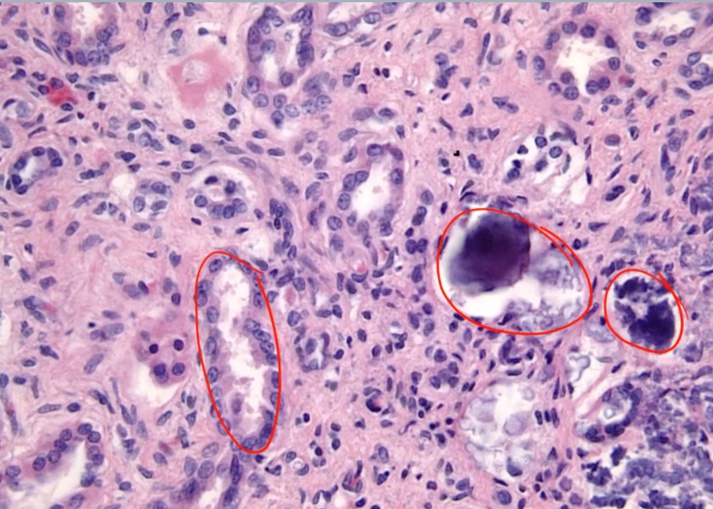
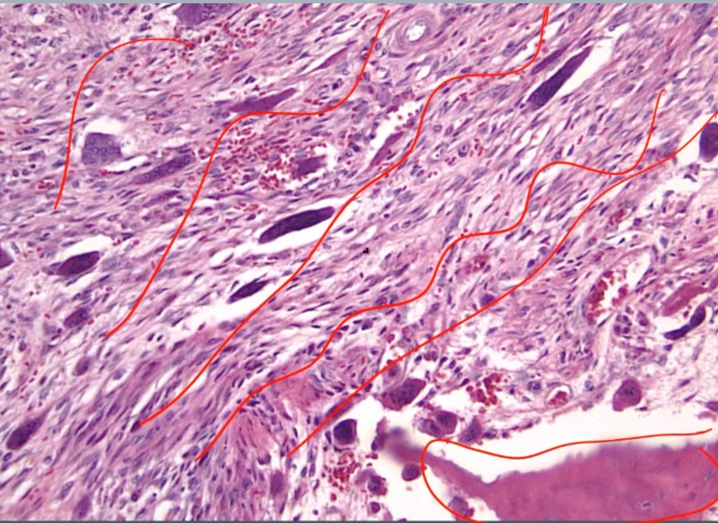
Osteitis Fibrosa Cystica
.
- Cystica means bone change
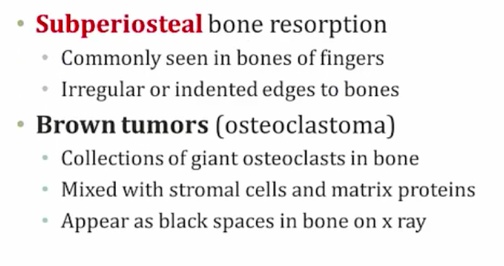
- Periosteum: membrane surrounding the bone

.
Histology shows fibrosis and bone spicules
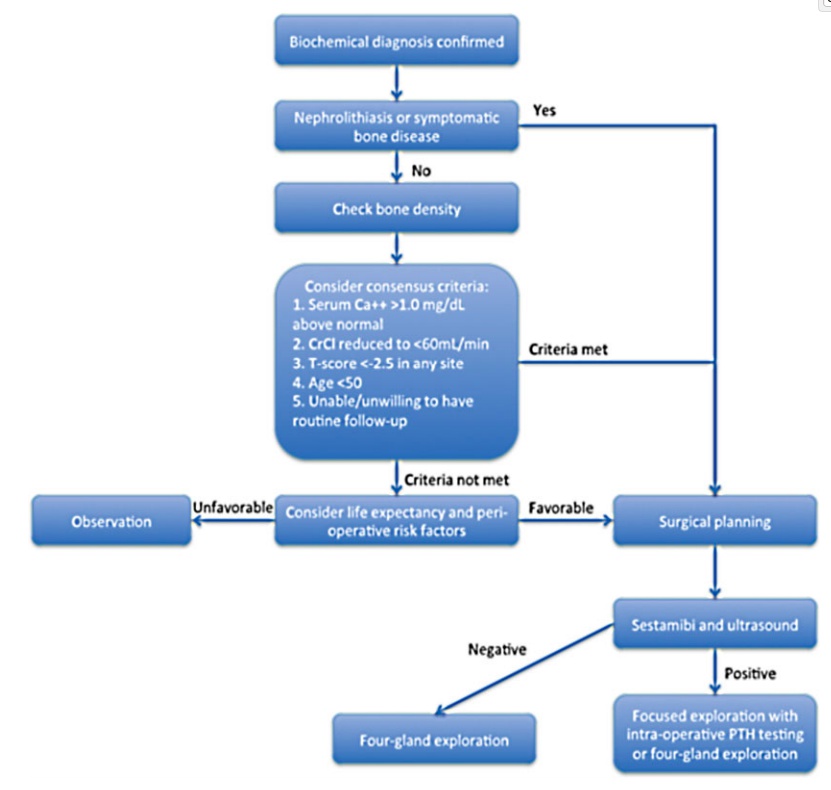
Primary hyperparathyroidism treatment
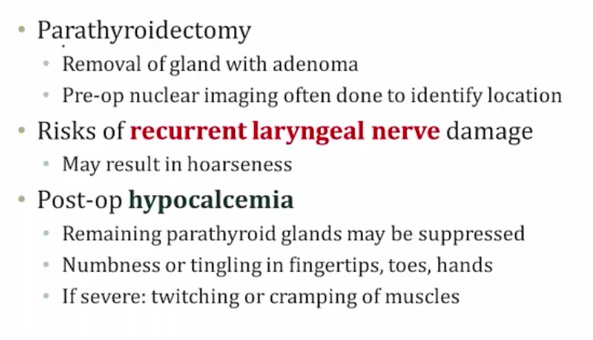
- post-op: takes time for remaining glands to start working.
Secondary
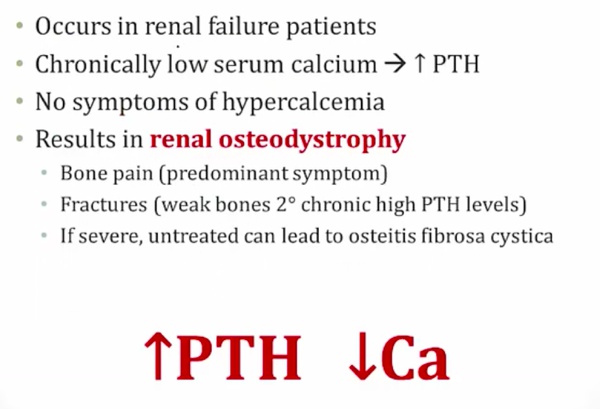
- bone pain from PTH
- high alk phos
Tertiary
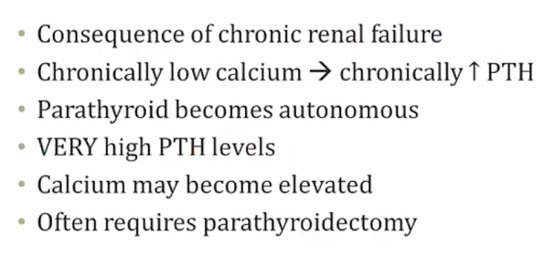
- parathyroid independent of Ca
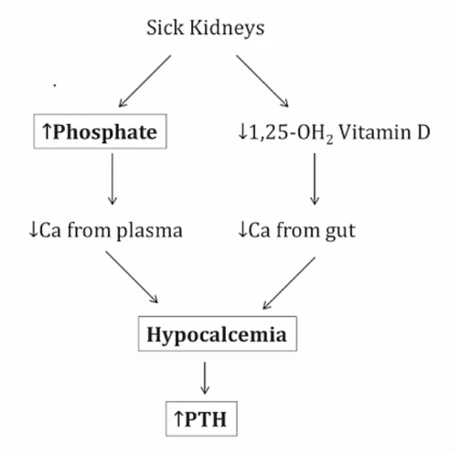
- Can’t excrete phosphate > more binding with Ca
- Can’t activate Vit D > Less Ca reabsorption
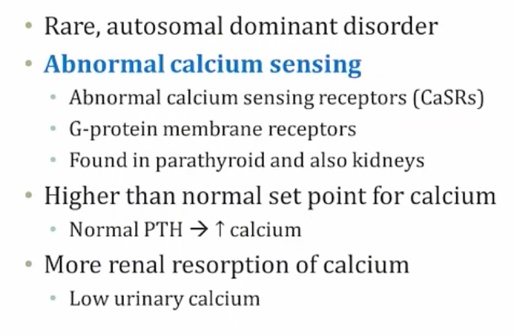
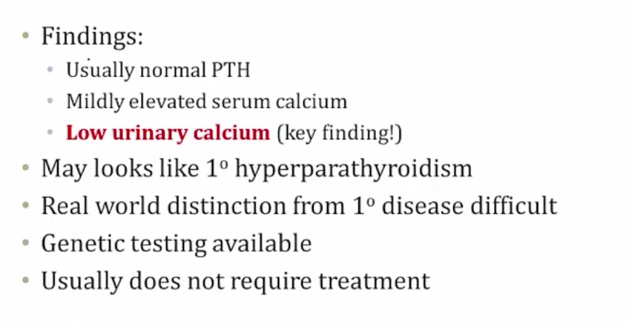
Familial hypocalciuria hypercalcemia
Hypoparathyroidism
- Autoimmune
- Congenital: DiGeorge
- Radiation
- post-op: days/weeks later
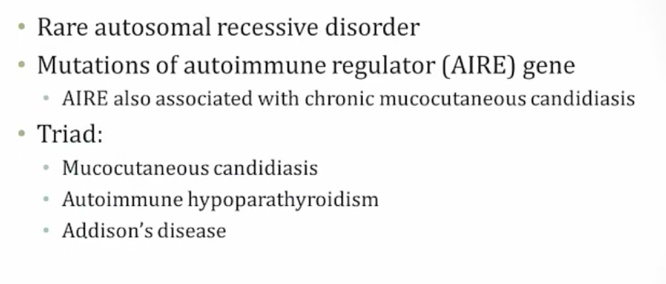
APS-1
Digeorge
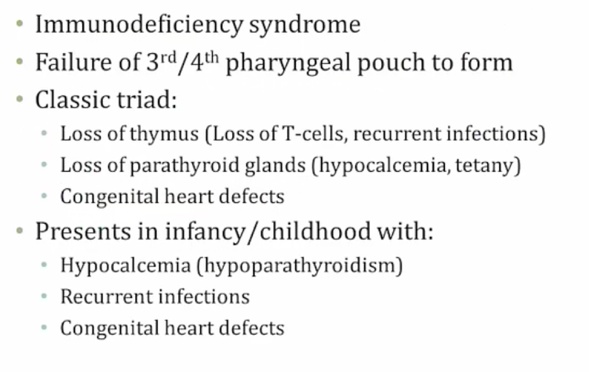
- thymic aplasia
Pseudohypoparathyroidism
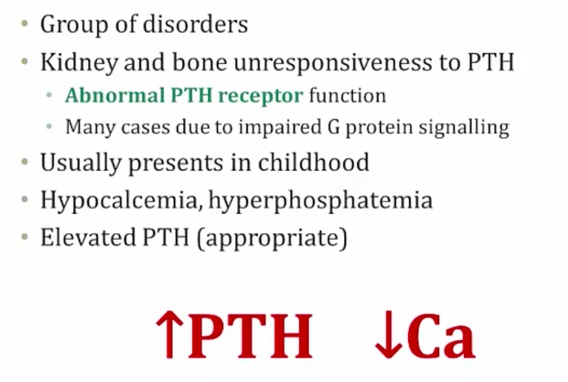
- Gs receptors
- Named pseudo because has signs and symptoms of hypoparathyroidism but not because of low hypoparathyroidism.
Albright’s Hereditary Osteodystrophy, AHO
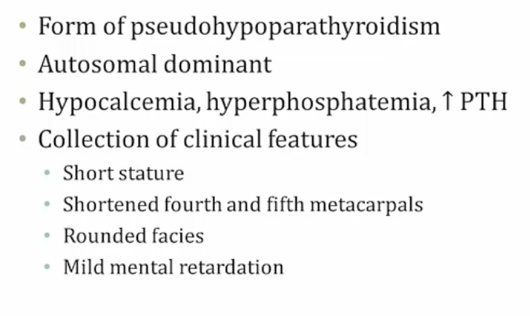
- Increased PTH, decreased Ca: Ca lost somewhere
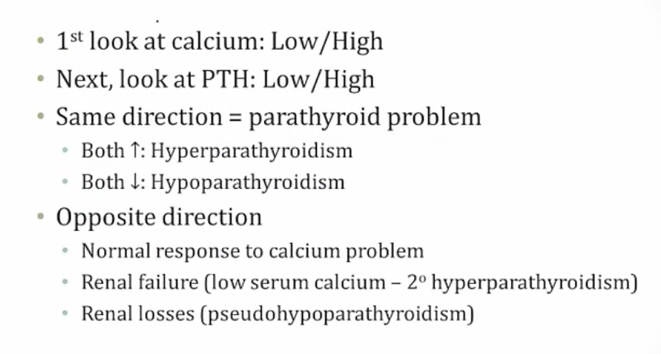
Ddx
- Hypercalcemia
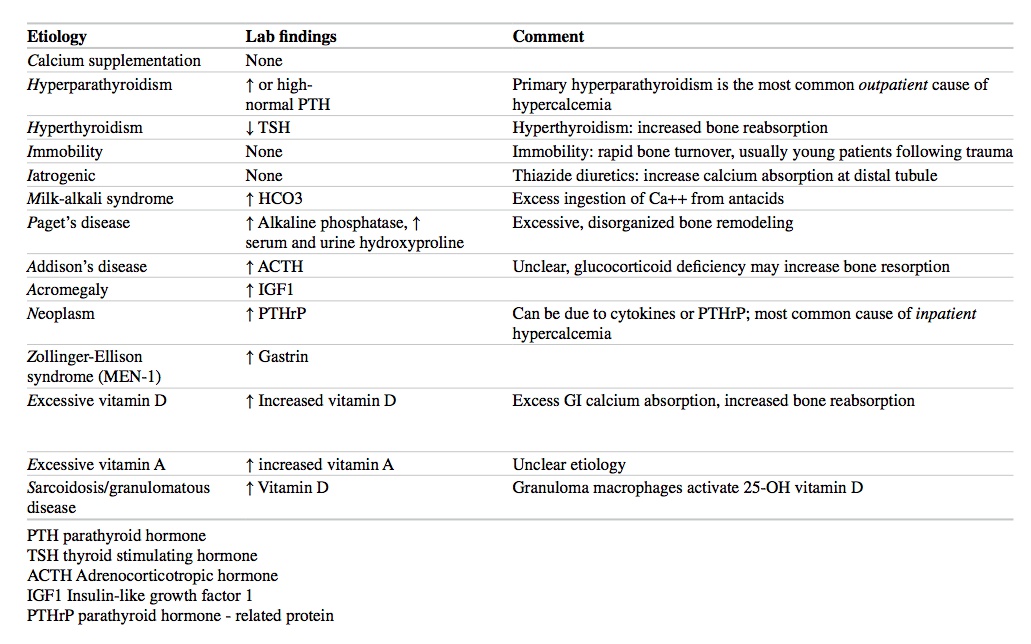
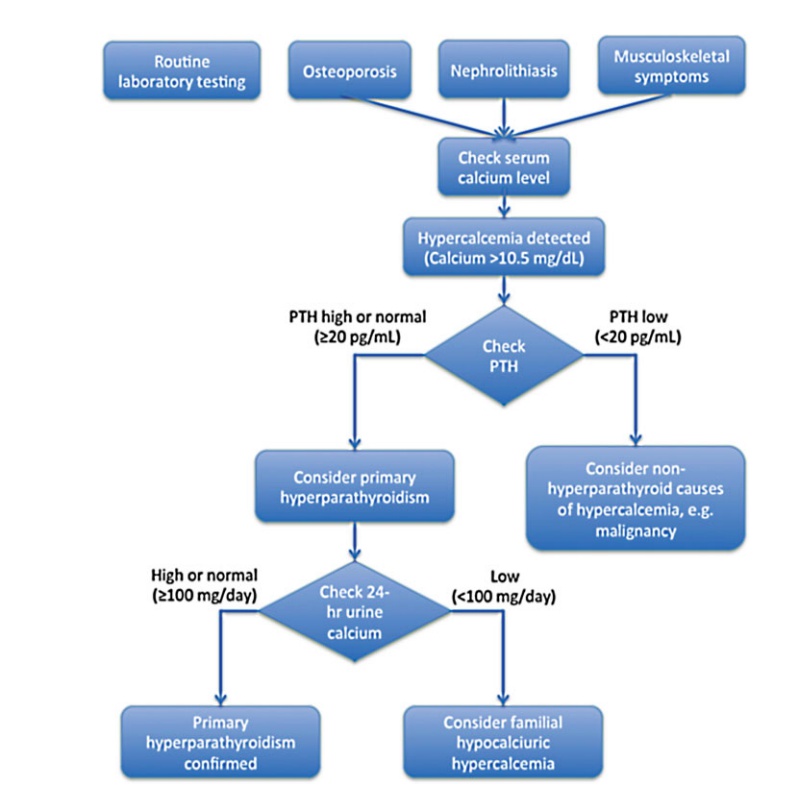
- Hyperparathyroidism workup: