acute and chronic silicosis
- related: Occupational Lung Disease
- tags: #pulmonology #literature #pulmonology
- work related lung disease: 1.silicosis
- associated infectious disease: 2.TB
Acute vs Chronic
- timing
- acute: several months to years
- chronic: 10-30 eyars
- CXR/CT
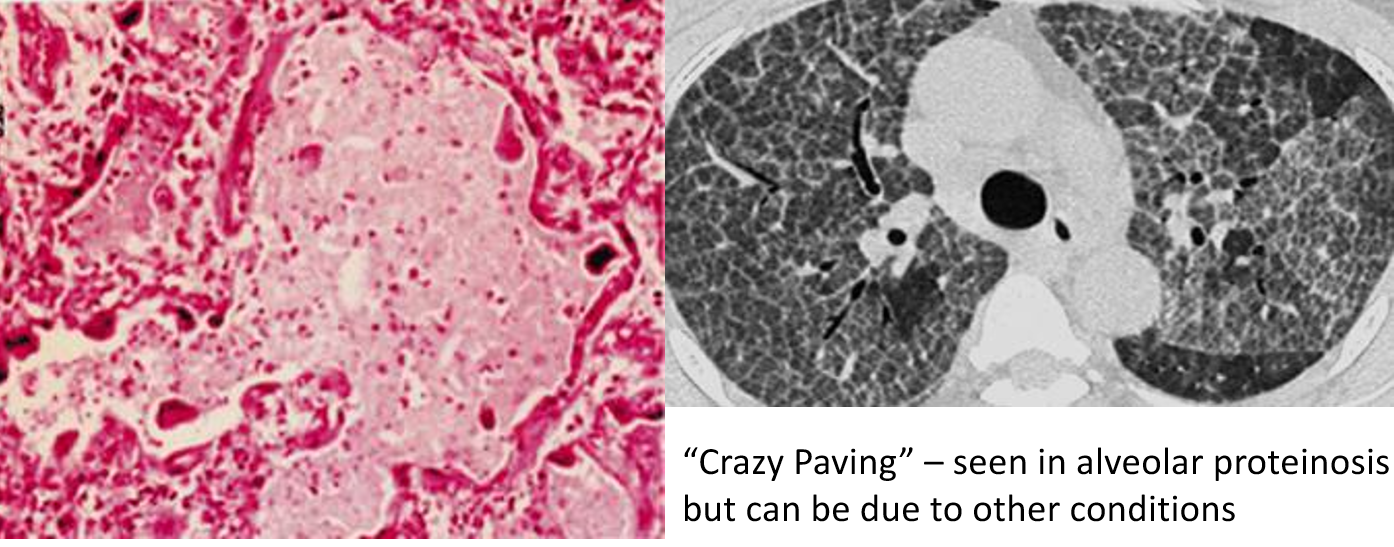
- acute: crazy paving
- chronic: egg shell calcification
- histology
- acute: alveolar proteinosis, interstitial infiltrates
- chronic: acellular1

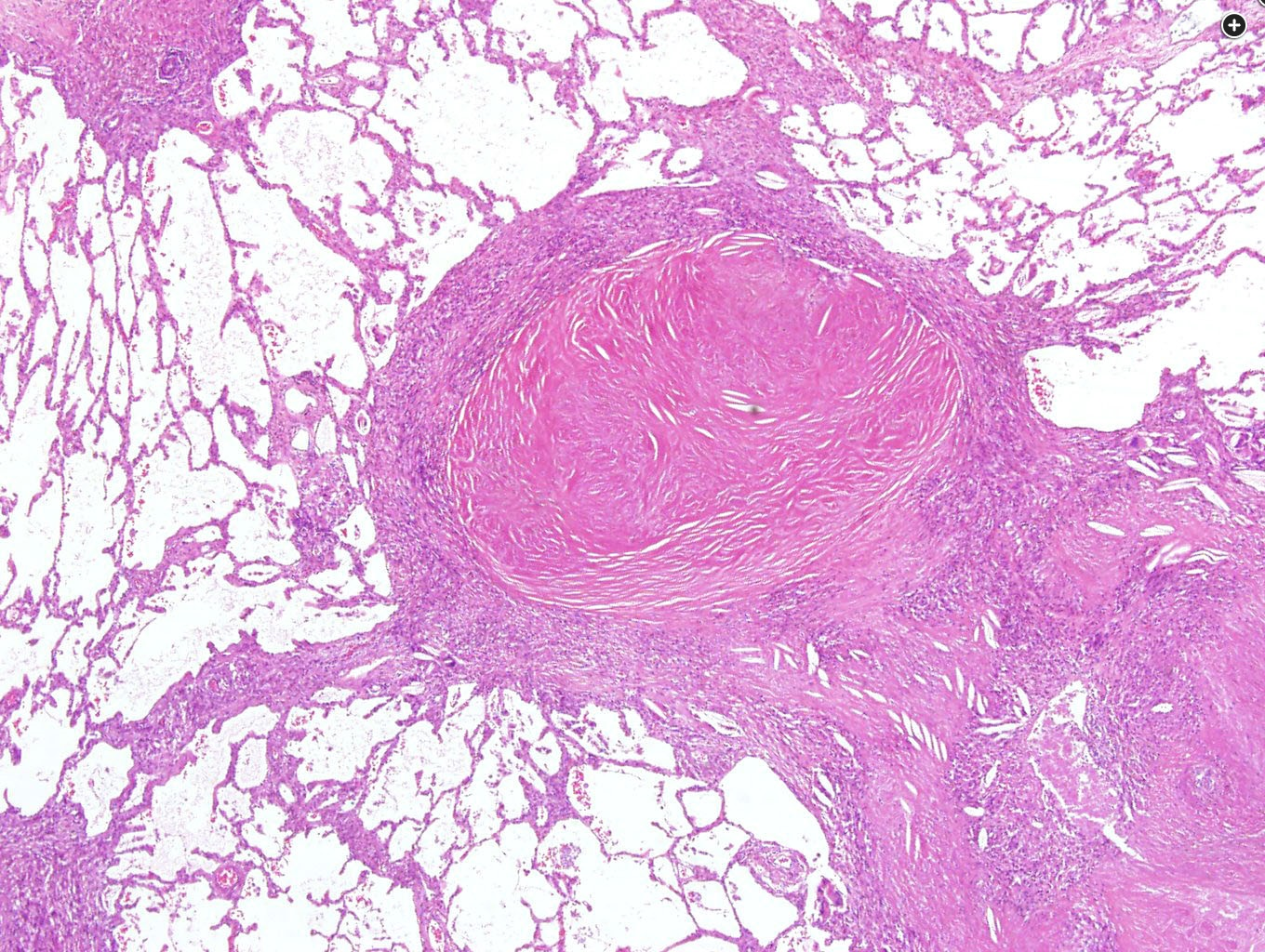
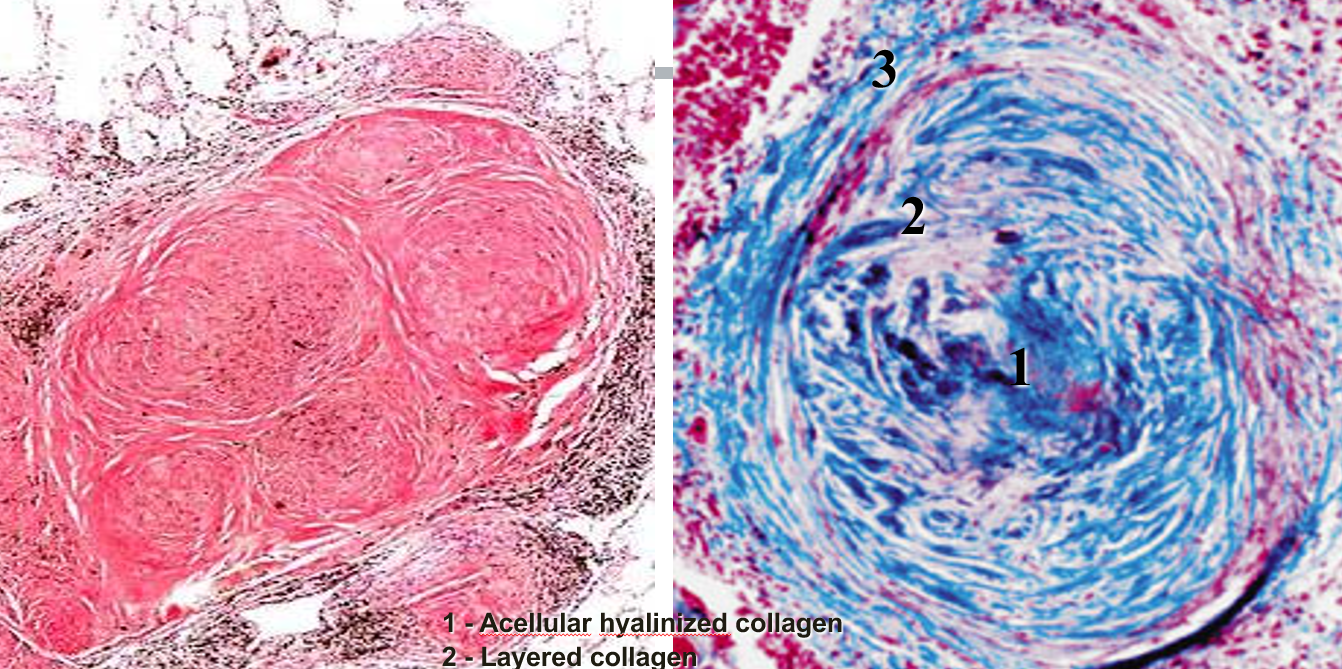
These nodular densities, a manifestation of chronic exposure, are composed of concentrically arranged coarse collagen bundles of low cellularity as shown.
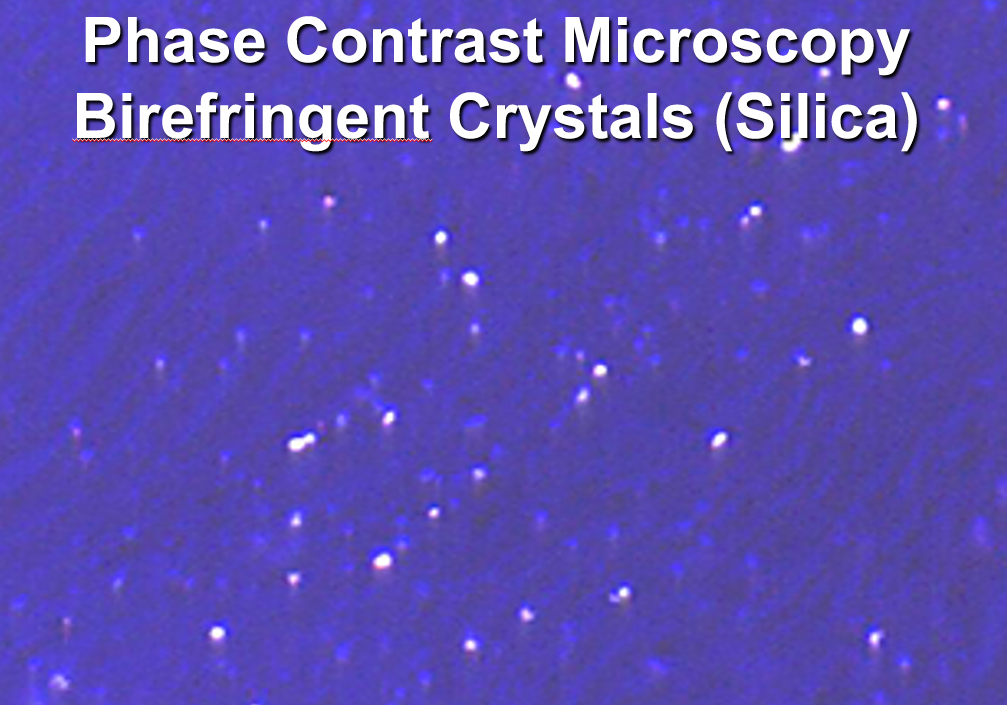
Earlier in the process of silicotic exposures, the central fibrotic core may be cuffed by a rim of lymphocytes and dust-laden macrophages. Cellular nodules (dust macules) made up of histiocytes, resembling granulomas, may also be seen and typically reflect mixed exposures (see below). There may be focal calcification and central necrosis seen variably within the nodules. If there is necrosis, it is assumed to be secondary to silicotuberculosis (not seen in this example). Mixed dust pneumoconioses such as those seen with inhalation of domestic (especially in developing global regions) or occupational coal dusts are typically manifested by the presence of dust macules, composed of histiocytes and variable amounts of other pigments, including anthracotic (black) pigment. Acute silicosis is manifested by alveolar proteinosis-like lesions. Although not shown here, use of polarized light microscopy allows for identification of silica within the nodules as weakly birefringent polyhedral particles, approximately 1 to 2 µm in maximal dimension, typically interspersed with pigment and brightly birefringent needlelike silicate crystals.
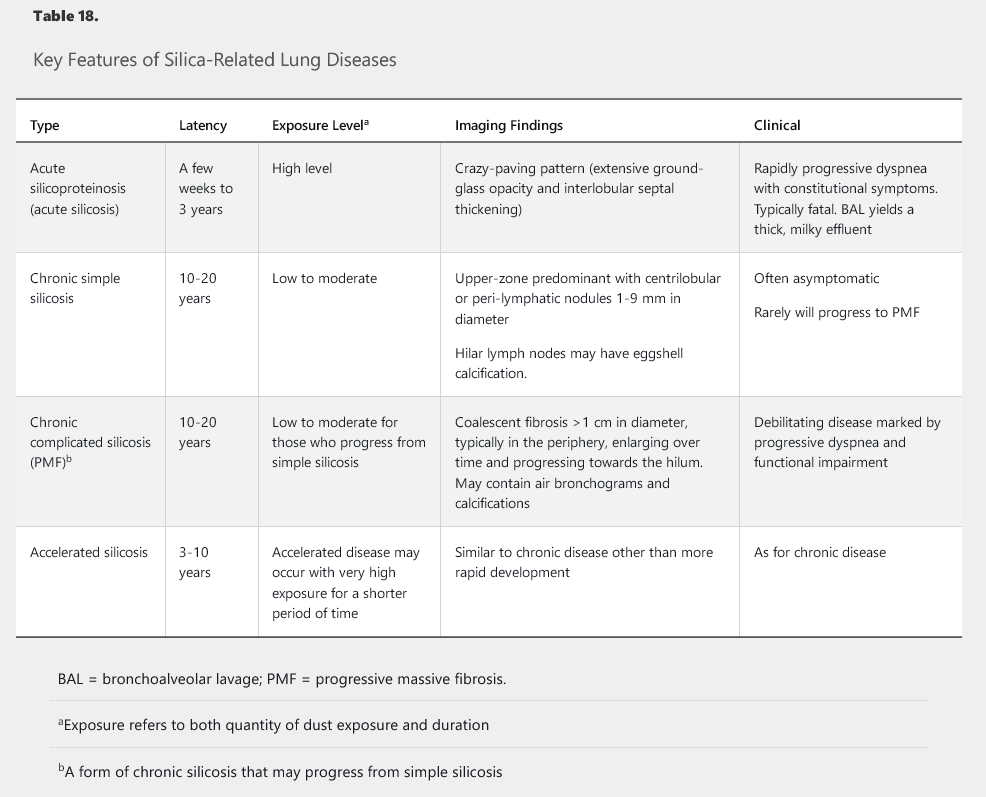
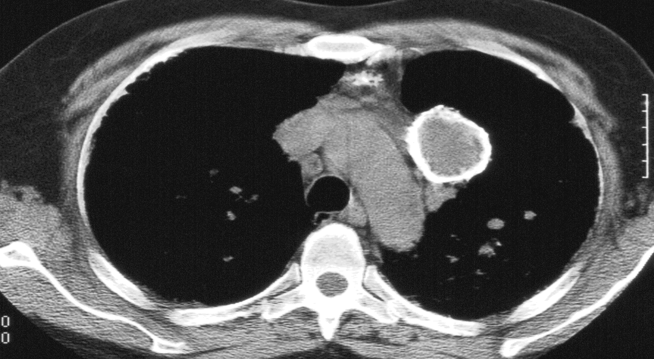
For an individual participating in an occupation involving drilling, sandblasting, or quarrying rock, such as those forging tunnels, exposure to crystalline silica is very common. Silicosis is a fibrotic pneumoconiosis resulting from inhalation of crystalline silicon dioxide particles, in most cases taking decades to develop and manifest with clinical symptoms. CT imaging typically reveals innumerable upper lobe–predominant, small, rounded, pulmonary nodules with a perilymphatic distribution; hilar and mediastinal adenopathy; and eggshell calcification of lymph nodes. In this case, the imaging was inconsistent with this pattern (choice A is incorrect).
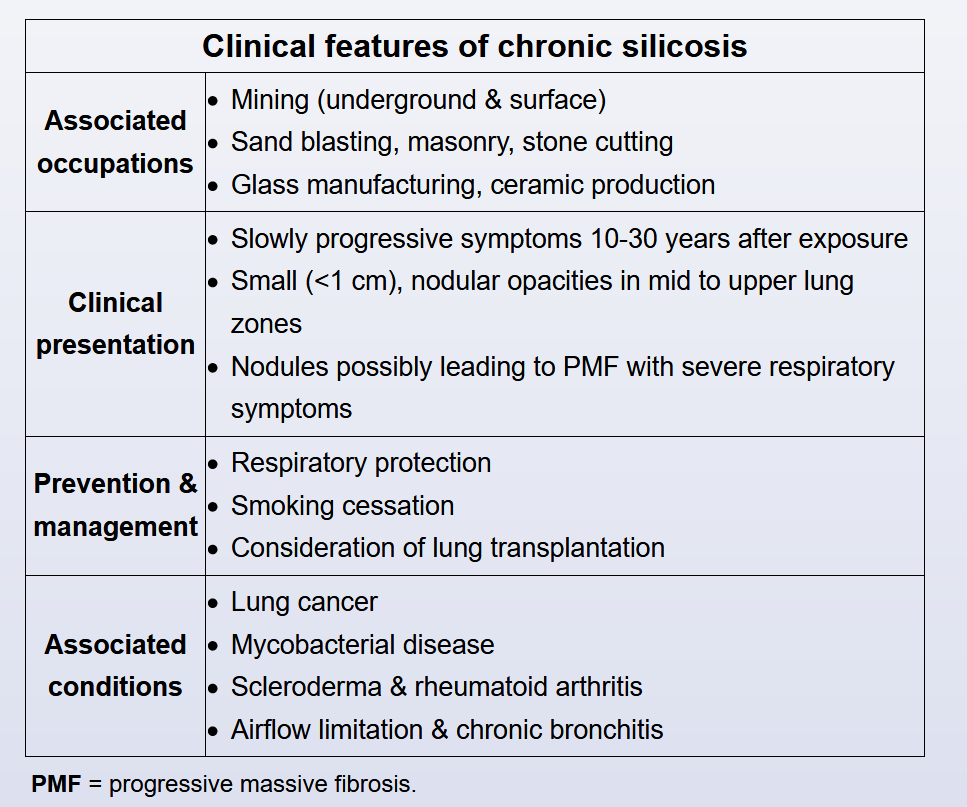
Occupations involving mining, quarrying, cutting, or polishing of stone such as tombstones, as well as work involving exposure to abrasives such as sandblasting or ceramics such as oven brickmakers, are at highest risk for exposure to crystalline silica and eventual development of silicosis.
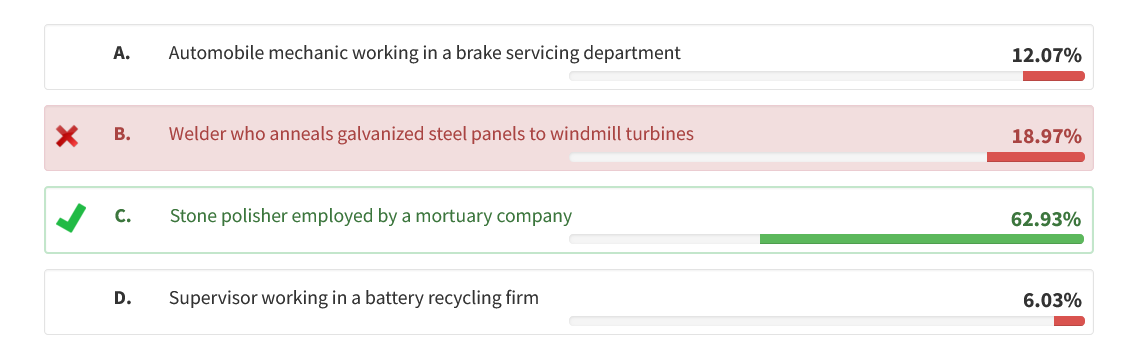
A welder assigned to adhere galvanized steel plating to prevent corrosion would be at higher risk for developing metal fume fever owing to exposure to zinc oxide, but not typically silicosis (choice B is incorrect). A supervisor in a battery recycling facility would be more likely to be exposed chronically to lead or other heavy metals but not to silica (choice D is incorrect).
Overview
- pt: mining, hydraulic fracturing, sandblasting, and foundry work
- prevention: Respiratory protection (eg, particulate respirator) is the best strategy for preventing the disease
- pathology: macrophage reaction to silica by activating fibroblasts and cause collagen production
- sx:
- 10-30 years later after exposure
- asymptomatic
- dyspnea on exertion, productive cough
- dx:
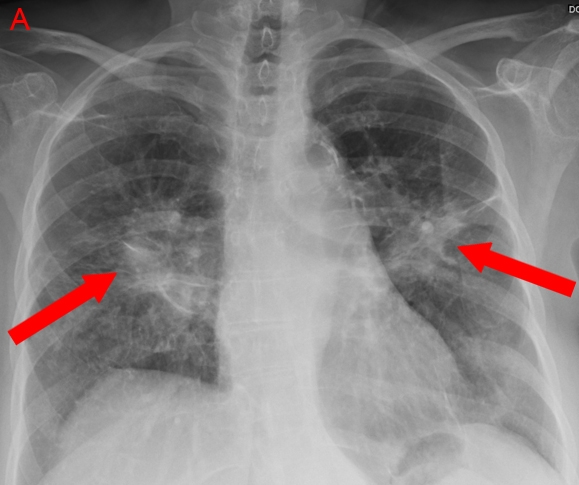
- cxr: many small, round opacities that are distributed predominantly in the upper lobes
- In advanced disease, the nodules can enlarge and coalesce, resulting in retraction of the hila, upper lobe fibrosis, and hyperinflation in the lower lobes
- may sometimes show calcification of rim of hilar nodule (eggshell calcificaiton)
- cavitation can also present
- complications
- associated with TB due to impaired macrophage response
- bronchogenic carcinoma
MKSAP
Silicosis is a fibrotic lung disease caused by the inhalation of silica dust. Silica exposure typically occurs in industries that grind, cut, or drill silica-containing materials such as concrete, tile, and masonry. Pottery making, foundry work, and sand blasting can also result in exposure. Sandblasting of denim jeans (stone washing) recently resulted in an outbreak of disease in Turkey. Hydraulic fracturing for natural gas and oil may expose workers to hazards, as this process involves fine sand and a wide variety of chemicals.
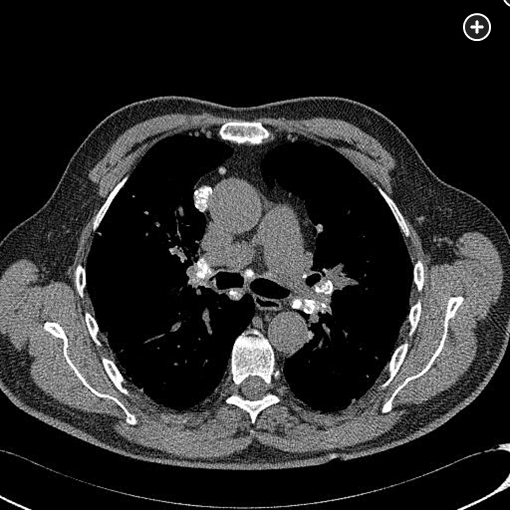
There are four main types of silicosis (Table 18), and they are associated with altered cell immunity and macrophage function. Patients with silicosis are at increased risk for the development of mycobacterial infection and connective tissue disease. Chronic silicosis is associated with the development of infection, including tuberculosis, and clinicians should have a high index of suspicion for this complication. Once fibrosis develops in silicosis, there is little evidence that any therapies alter disease course. If individuals have continued exposure, removal from the environment will prevent further lung injury. Silica exposure is associated with increased risk of lung cancer, particularly for smokers. As a result, smoking cessation remains an essential intervention.