approach to abnormal liver enzymes, transaminitis
- related: GI gastroenterology
- tags: #GI
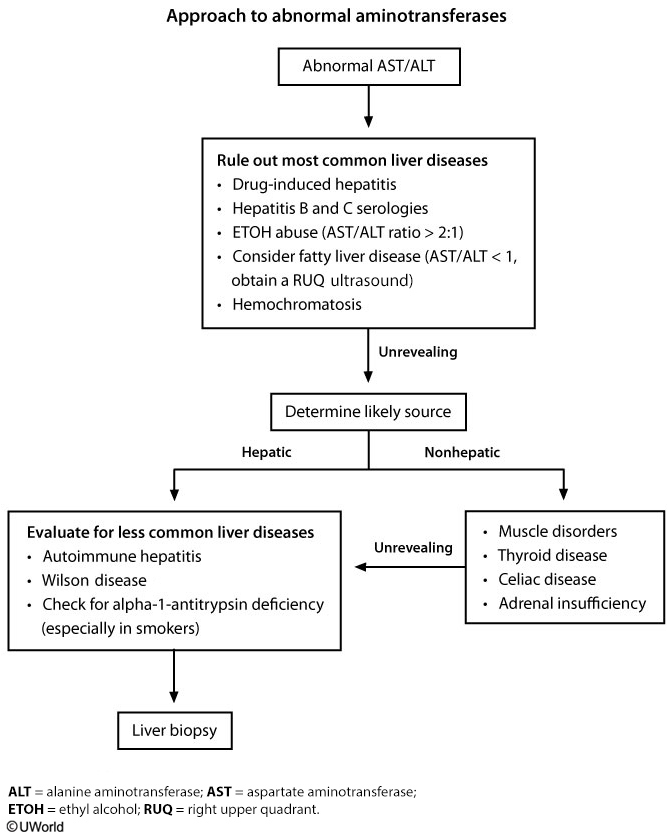
This patient with mild aminotransferase elevations in the setting of autoimmune disease (vitiligo, hypothyroidism) and iron deficiency anemia likely has celiac disease. Celiac disease is a chronic malabsorptive disorder of the small intestine caused by immune-mediated hypersensitivity to gluten and is frequently associated with other autoimmune diseases (eg, type 1 diabetes mellitus, hypothyroidism). The initial evaluation should include serologic testing for IgA anti-tissue transglutaminase and IgA endomysial antibody; small bowel enteroscopy with biopsy can confirm the diagnosis.
Celiac disease classically presents with gastrointestinal (eg, diarrhea, abdominal pain) and malabsorptive (eg, weight loss; deficiencies of iron, folate, or vitamin B12) symptoms. However, extraintestinal symptoms may include osteoporosis, arthritis, neurologic symptoms, infertility, and elevated aminotransferases, which can occur with minimal or no intestinal symptoms. Therefore, celiac disease should be considered in any patient with an autoimmune history who develops unexplained iron deficiency anemia or any of the recognized extraintestinal manifestations.
Hereditary hemochromatosis causes elevations in aminotransferases but is unlikely in a premenopausal woman due to the regular iron loss that occurs with menses. The presence of microcytic anemia despite iron supplementation virtually rules out this diagnosis.
Chronic alcoholic liver injury is characterized by elevations in aspartate aminotransferase (AST) greater than alanine aminotransferase (ALT), typically with a ratio of >2:1 (this patient has ALT>AST). In addition, chronic alcohol intake usually causes a macrocytic rather than microcytic anemia.
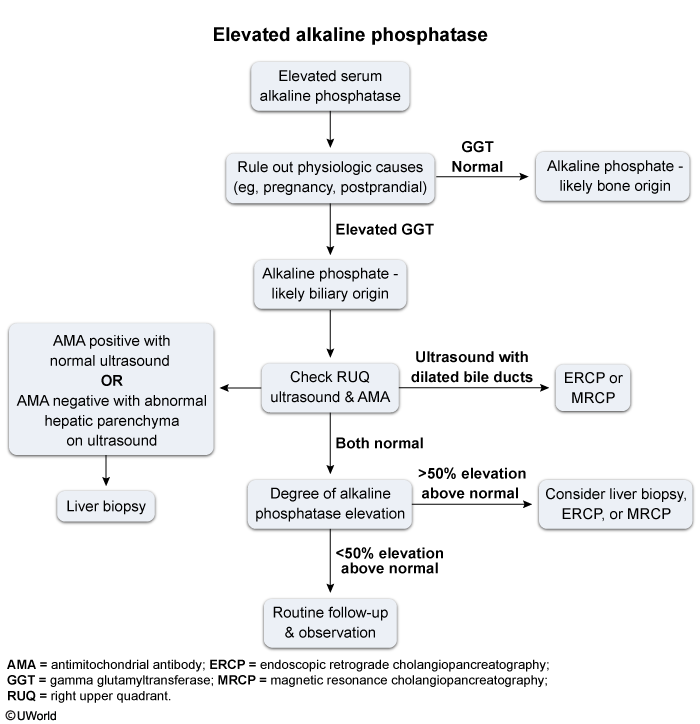
Primary biliary cholangitis usually presents with fatigue, pruritus, and elevated alkaline phosphatase (but relatively normal transaminase levels). This patient’s normal alkaline phosphatase and absence of pruritus make this less likely.
Alk Phos