Asynchrony Consequences and Management
- related: ICU intensive care unit, DeepCrit Cycle Dessynchrony
- tags: #literature
- source: pubmed
- vent dyssynchrony occurs either with high respiratory drive or low respiratory drive
- high respiratory drive results from too low of ventilator assistance
- low respiratory drive results from too much ventilator assistance
High respiratory drive
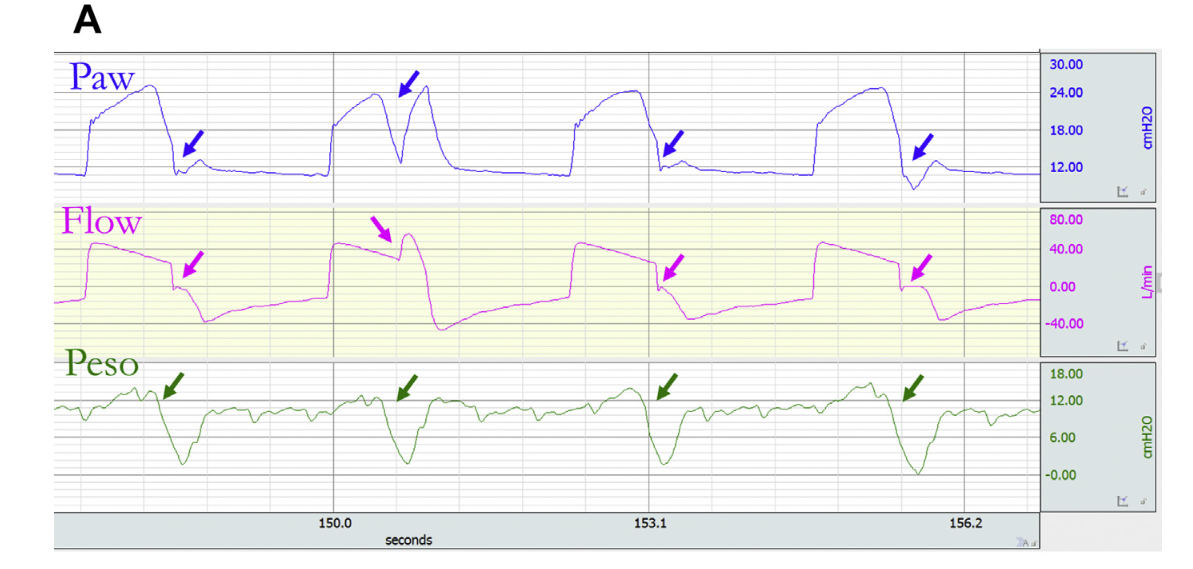
Flow starvation
- occurs when patient does not get enough air
- can be recognized with concave indentation on pressure curve as patient pulls air in
- management
- increase flow rate
- change to pressure support or pressure control so patient can adjust their own flow
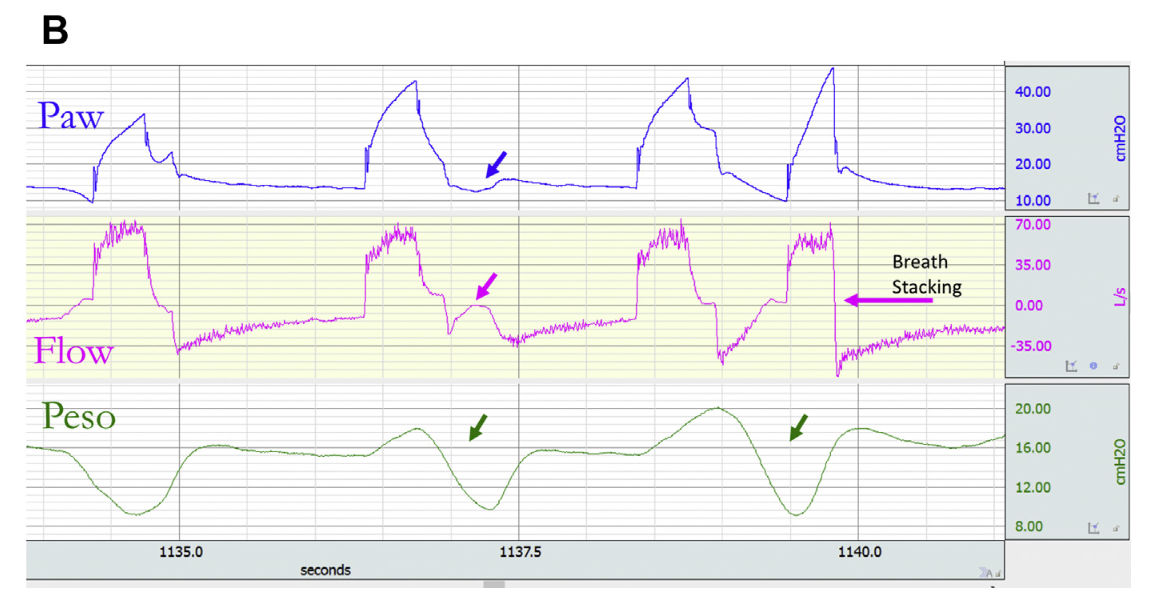
Short cycling
- occurs when patient continues to inspire during expiration
- when strong enough can cause double triggering (second breath) or breath stacking
- also has association with shorter inspiratory time
- occurs often in ARDS with low TV ventilation, worse lung injury, increased respiratory drive
- management
- can try increase sedation, increase tidal volume, increase inspiratory time, change to PS mode
Low respiratory drive
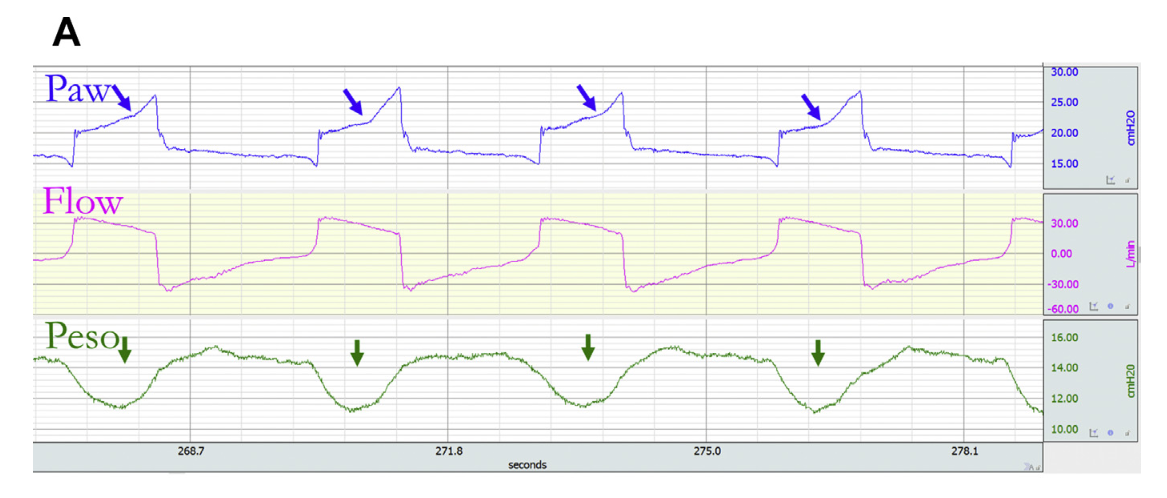
Reverse triggering and double cycling
- occurs more in deep sedation and decreased respiratory drive
- ventilator triggers a muscular effort
- can be seen with expiratory flow or decrease in inspiratory pressure in later cycle
- can also have second breath with resulting breath stacking
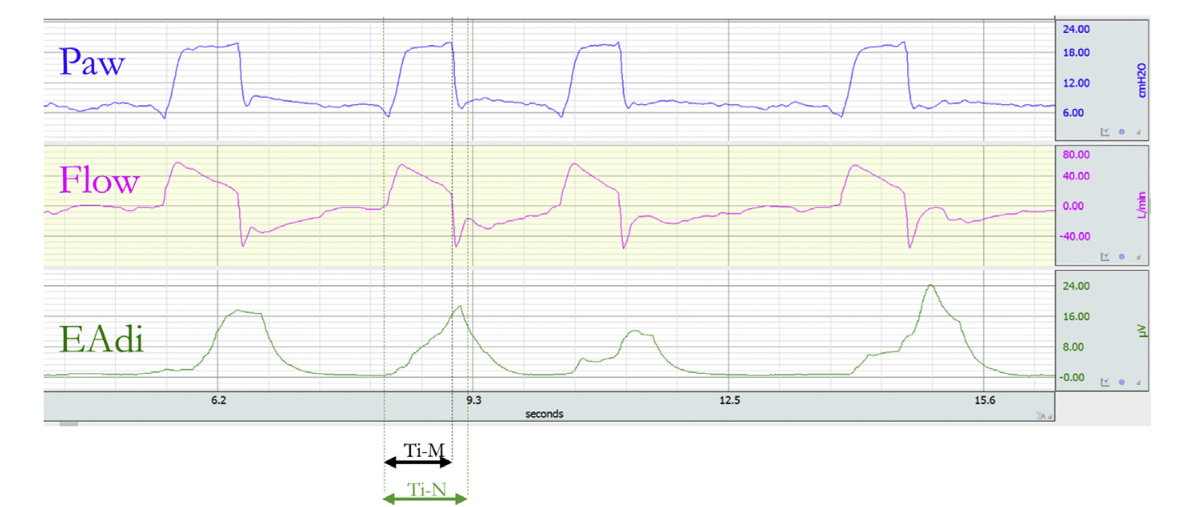
Delayed cycling
- occurs when mechanical inspiration continues after patient inspiration has stopped
- COPD and asthma patients are at more risk, leading to shorter expiratory time
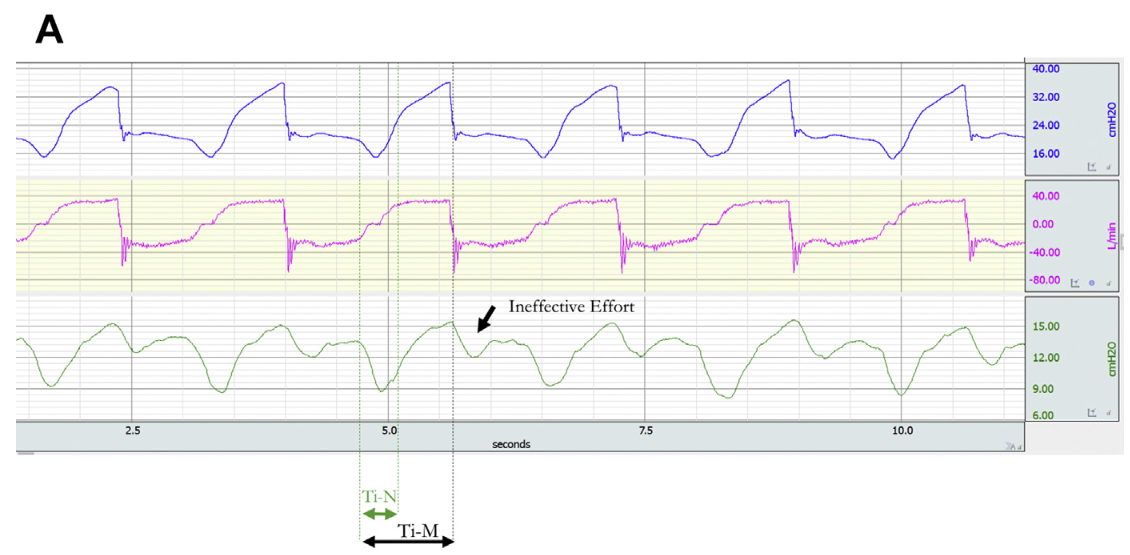
Ineffective efforts
- occurs when patient effort does not lead to breath on the vent
- happens more with airflow obstruction with autoPeeping => patient effort insufficient to overcome autoPeep
- also can happen with over sedation and decreased effort
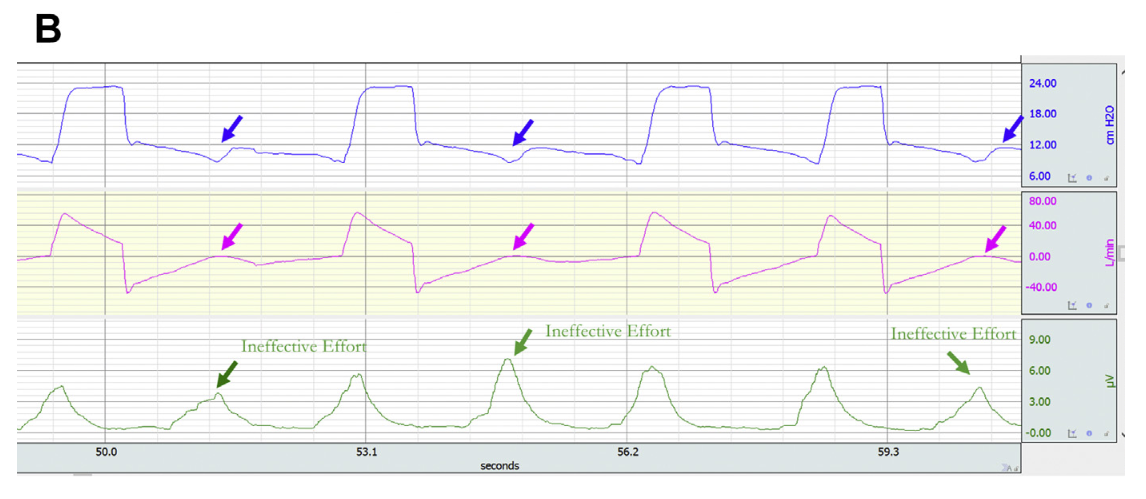
- management
- increase ventilator sensitivity
- switch from pressure to flow trigger
- give more PEEP for autoPeeping