Back Pain
Alarming symptoms
-
alarming symptoms:
- bowel, bladder incontinence
- saddle anesthesia
- any FND that’s new or rapidly progressing
-
path: muscle spasm
-
pt: young, male, heavy lifting
-
symptoms: back hurts, no alarming symptoms, “delt like,” asymmetric/unilateral
-
diagnosis: clinical
-
treatment: exercise, NSAIDS.,
- infarction: rapid onset
- compression: slow progressive onset
Workup
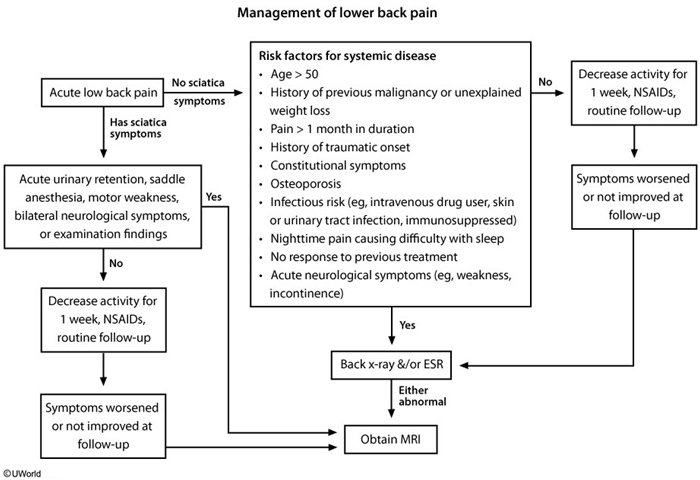
Someone comes in with lower back pain:
- if alarming symptoms, think cord compression:
- Give IV steroids ASAP
- Xray or jump to MRI if giving steroids
- Decompress the compression
- hematoma: drain
- abscess: incision drainage + abx
- cancer: radiation
- fracture: surgery
- if nonspecific, vague complaints, think musculoskeletal pain:
- NSAIDS, exercise
- Do not pick bedrest
- No imaging needed
- reassess in 4 weeks
- improvement: continue
- failed improvement or if positive symptoms: something else
- Xray
- if negative Xray, MRI
- some form of surgery
Cord Compression
- causes
- Spinal injury (eg, motor vehicle crash)
- Malignancy (eg, lung, breast, prostate cancers; myeloma)
- Infection (eg, epidural abscess with IV drug users or diabetes)
- Symptoms
- Gradually worsening, severe local back pain
- Pain worse in the recumbent position/at night
- Early signs: Symmetric lower extremity weakness, hypoactive/absent deep-tendon reflexes
- Late signs: Bilateral Babinski reflex, decreased rectal sphincter tone, paraparesis/paraplegia with increased deep-tendon reflexes, sensory loss
Most patients present with progressively worsening back pain. Pain is usually worse in the recumbent position (due to distension of the epidural venous plexus when lying down) in contrast to back pain from degenerative joint disease, which improves with recumbency. Bilateral lower-extremity weakness is present in about 60% of patients. Sensory loss below a spinal level and gait ataxia may occur. Paraplegia and bowel or bladder dysfunctions (eg, fecal or urinary retention/incontinence) are late findings. Examination shows focal point tenderness in the spine, exaggerated deep-tendon reflexes in the legs, and upgoing plantar reflexes.
In the acute phase of spinal cord injury, patients can develop spinal shock and have absence of reflexes and flaccid paraplegia.
Management
- Emergency MRI
- Intravenous glucocorticoids
- Radiation-oncology & neurosurgery consultation
- infarction: rapid onset
- compression: slow progressive onset
MSK Pain
- path: muscle spasm
- pt: young, male, heavy lifting
- symptoms: back hurts, no alarming symptoms, “delt like,” asymmetric/unilateral
- diagnosis: clinical
- treatment: exercise, NSAIDS.,
Disc Herniation
- path: nucleus pulposus pinching nerve
- pt: 30-50 yo male, heavy lifting
- symptoms: sciatica, lightning shock pain down leg, positive straight leg test
- diagnosis: Xray probably negative, MRI next
- treatment: depends on severity/lifestyle
- neurosurgery > conservative at 6 mo (probably atheletes)
- neurosurgery = conservative at 1 yo (probably older guy just wants to live)
Acute lumbosacral radiculopathy
This patient’s symptoms - back pain radiating down the leg which is worsened with coughing or bearing down - are consistent with an acute lumbosacral radiculopathy (ALSR). ALSR is most often due to a mechanical compression of the L5 and/or S1 dorsal root, usually by a herniated disk. ALSR typically presents with low back and leg pain (sciatica), often with associated numbness and/or weakness in the leg. Reproduction of radicular pain with flexion at the hip and dorsiflexion at the ankle (positive straight leg raise) is relatively specific for the diagnosis.
Most patients with ALSR will have spontaneous improvement, and can be managed with conservative measures for comfort. Studies of various medications in ALSR have largely been mixed, though non-steroidal anti-inflammatory drugs (NSAIDs) are often effective and are well tolerated. Anti-spasmodics/muscle relaxants may also be considered, but they are associated with significant sedation and inconsistent benefits. Opioids appear to be less effective and are associated with sedation and a significant risk of dependence. Pain-modifying drugs such as gabapentin are primarily used for chronic symptoms and also cause significant sedation (Choice B).
Patients with ALSR should usually be advised to maintain light-normal activity. A brief period of bed rest (<3 days) is also acceptable, but extended bed rest has been shown to provide no benefit and may prolong recovery. If the patient’s symptoms fail to improve, or there are new neurological deficits at follow-up, magnetic resonance imaging of the lumbo-sacral spine and surgical referral may be indicated.
Osteophyte
- path: bony spur growing into canal and pinches nerve
- pt: older male, no heavy lifting
- symptoms: asymmetric, unilateral, sciatica, + SLR
- diagnosis: Xray probably negative, MRI showing bone spur
- treatment: surgery. Not going to get better with conservative
Compression Fracture
- path: osteoporosis
- pt: >50, female, falls
- symptoms: vertebral step-off, pinpoint tenderness
- diagnosis: xray probably positive, MRI better
- treatment: surgery, dexa scan for osteoporosis.,
Spinal Stenosis
- path: narrowing of canal, pinching of nerve
- pt: old, male or female
- symptoms: pseudoclaudication in butt/thighs, positional (claudication when walking around upright)
- diagnosis: xray probably negative, MRI better
- treatment: surgery, laminectomy.,
Others
- women in menstrual cycle with lower back pain, treatment with NSAIDS
- back pain with abdominal pulsating mass: aortic aneurysm
Back Pain
The characteristics of the back pain described in this scenario are typical for nerve root irritation. The pain is frequently brief and shooting, and radiates along the corresponding nerve distribution. It can be provoked by forward bending, coughing, or straining, and it diminishes on lying down. A positive straight-leg raising test at a 60 degree angle or less is characteristic.
Spinal stenosis is responsible for neurogenic claudication. In contrast to radiculopathy, the pain in spinal stenosis increases with extension of the spine and decreases with flexion of the spine.
The diagnosis of spinal stenosis in a patient with symptoms is best confirmed by using MRI of the spine. The encroaching of osteophytes at the facet joints, hypertrophy of the ligamentum flavum, and protrusion of intervertebral disks results in a narrowing of the spinal canal. In some patients, gait disturbance is so prominent that they complain of having “spaghetti legs” or walking “like a drunken sailor.” The preservation of pedal pulses helps distinguish this disease from vascular claudication.