breastfeeding
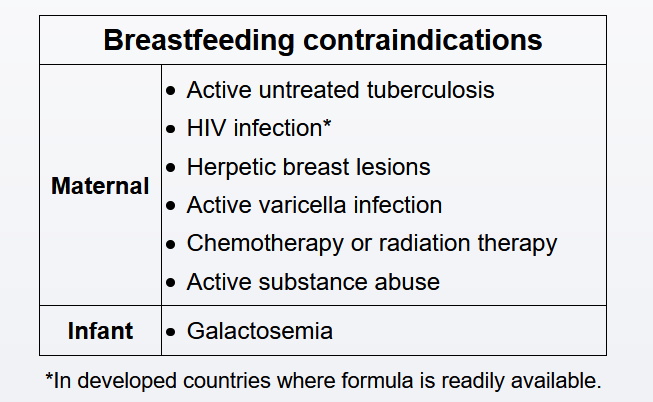
Breast milk is the optimal form of infant nutrition due to its immunologic properties; however, breastfed infants are at risk of postnatal HIV acquisition. In the United States and other industrialized countries with access to clean water for formula, women with HIV are advised to formula-feed their infants.
In resource-poor countries, formula feeding is associated with an increased risk of water-borne infectious disease (eg, diarrhea). In these countries, breastfeeding decreases infant morbidity and mortality rates by providing protective maternal antibodies and minimizing exposure to water-borne pathogens. In addition, most antiretroviral drugs are excreted in breast milk in significant enough quantities to provide passive infant protection and decrease the risk of postnatal HIV transmission.
Breastfeeding should be encouraged in women with epilepsy as the benefits of breastfeeding outweigh the risk of exposure of the infant to antiepileptic drugs (AEDs). Studies show that neurodevelopmental outcomes in these breastfed infants are either better than or no different from those who are not breastfed (Choices C and D). Sedating AEDs (eg, benzodiazepines, phenobarbital) can sometimes cause the child to become irritable or sleepy; in these cases, breastfeeding should be discontinued, but it can be attempted again after a week.