cardiac pacing EKG examples
- related: cardiac pacemaker
- tags: #permanent


Troubleshoot
Pacemaker is not sensing intrinsic activity, but fortunately, it’s also not capturing anything.

Seems to capture the first 3 beats, but then stops capturing (no P or QRS).
Not sensing what little intrinsic activity there is, but also not capturing anything.
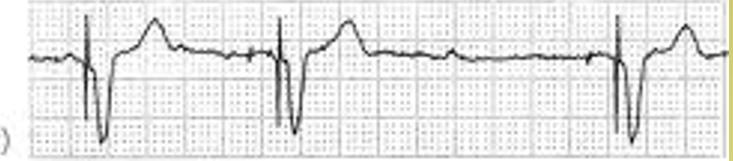
It captures each paced beat, but does not fire, suggesting it sensed something that was not there – did it sense the one wave as a P or QRS and inappropriately inhibit?
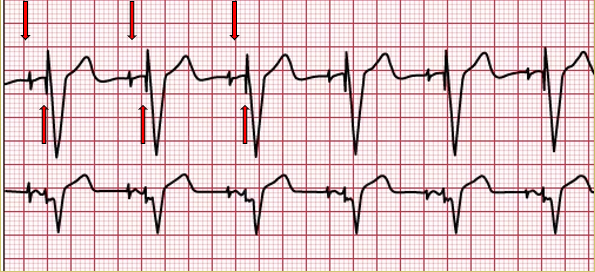
The first pacer spike does not seem to capture, nor does the second. Then there are 2 pacer spikes way too close together, and the second spike seems to create (capture) a QRS complex. The cycle is repeated 5 beats later. I think this was a permanent internal VVI pacer that sensed the temporary transcutaneous pacer, even though the external pacer did not capture.
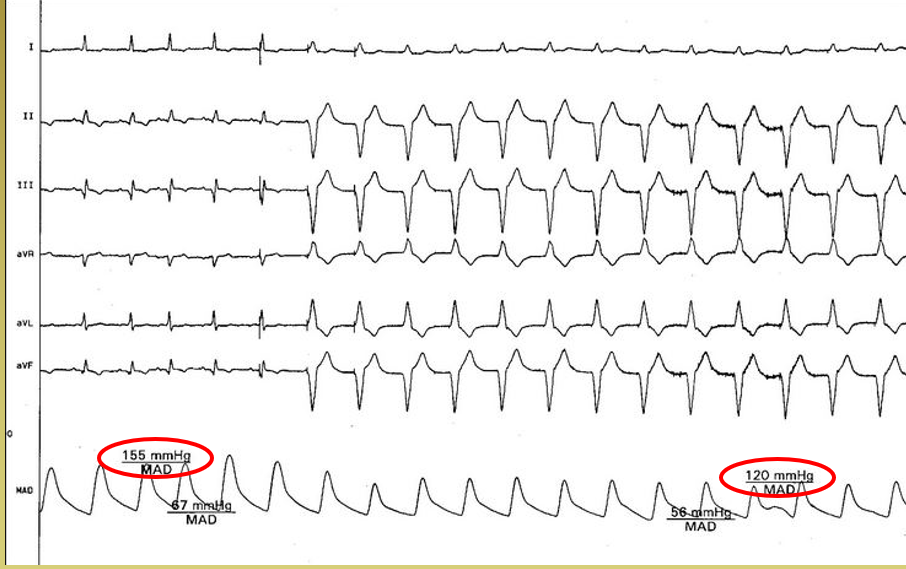
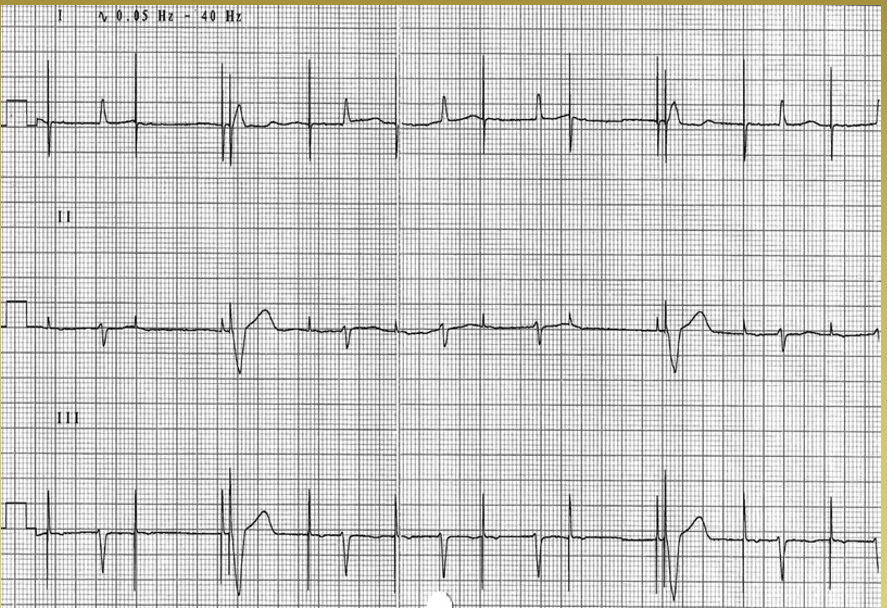
The fifth beat appears to be paced, as does the next one. Though hard to see spikes, it looks like all the rest are V-paced, as they have the wider QRS, suggesting they are not conducted via normal pathways. The big issue here is the drop in BP as the “atrial kick” is lost.
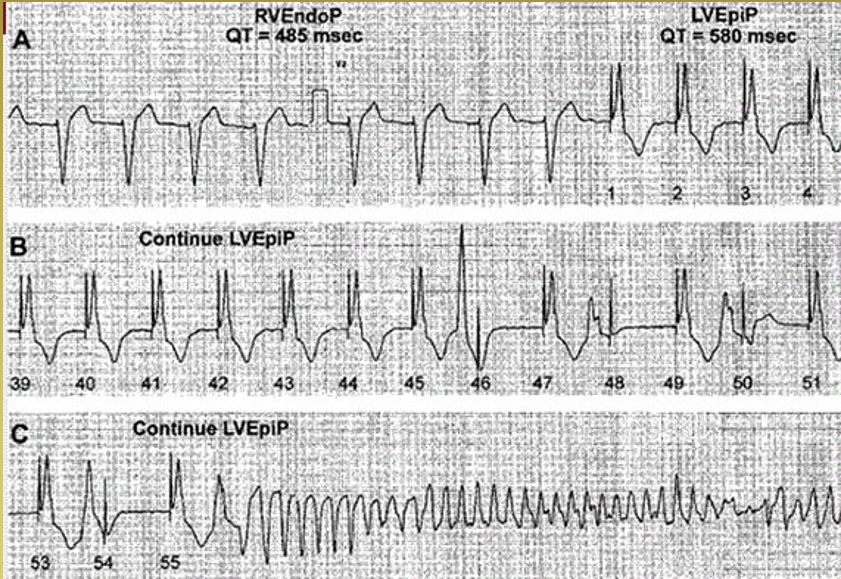
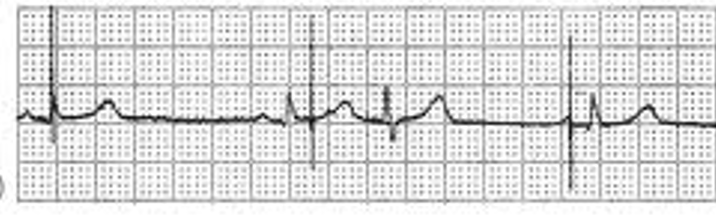
This is a rare, but fatal issue with telemetry. Beat 1 shows pacing beginning. Beat 46 shows a PVC followed by a pacing spike right in the T wave. It happens again in beats 48, 50 and 54. Although the spike is not visible, it happens again on beat 56, causing ventricular tachycardia/fibrillation.
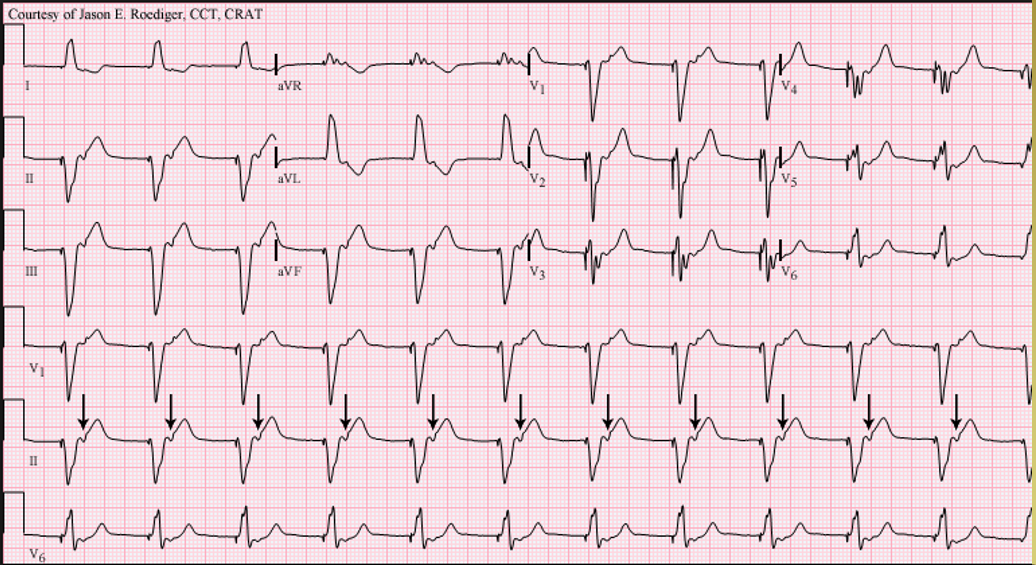
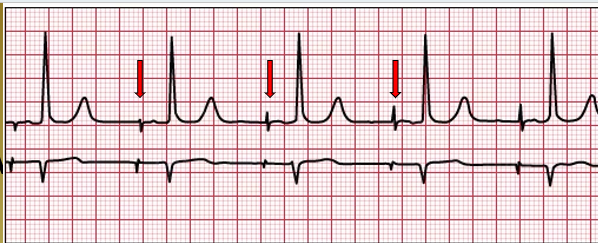
The arrows are pointing out what are probably retrograde P waves, suggesting retrograde conduction. Could you just A-pace, have antegrade conduction and A-V synchrony?
Managed Ventricular Pacing (MVP)
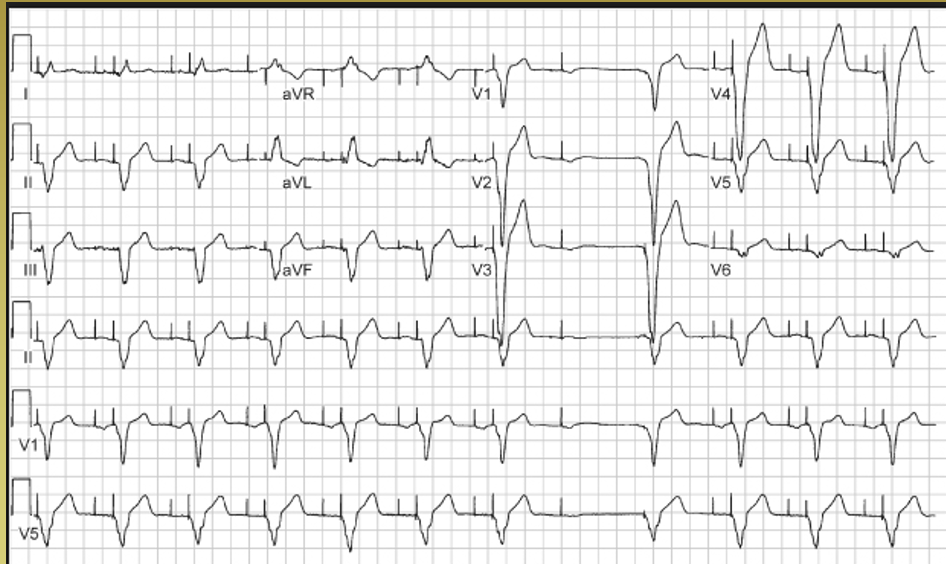
Don’t underestimate the programming of permanent pacemakers. Some (like this one) will test every 24 hours to see if dual chamber pacing is still required, or if atrial pacing, or no pacing, will suffice. This device tried an Atrial pace, but there was no ventricular beat, so it reset and resumed A-V pacing. Confusing until the programming was reviewed – this might be misinterpreted as an A-pace with inappropriate sensing of a non-existent QRS.
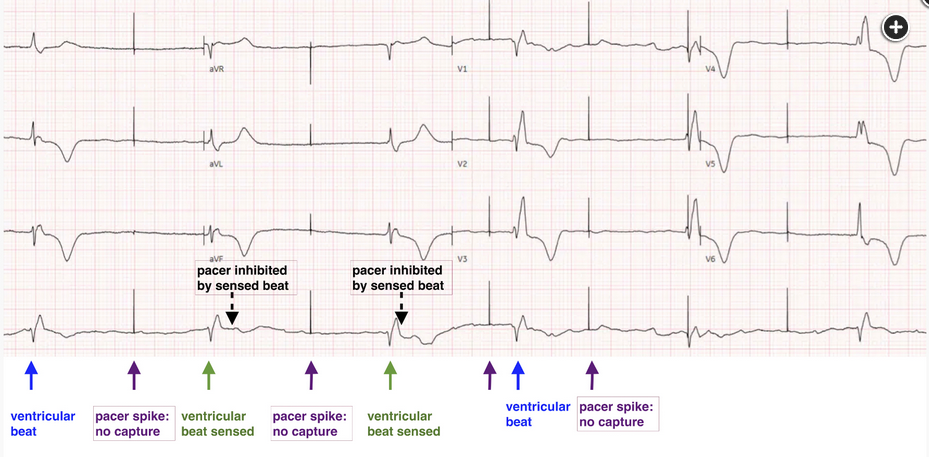
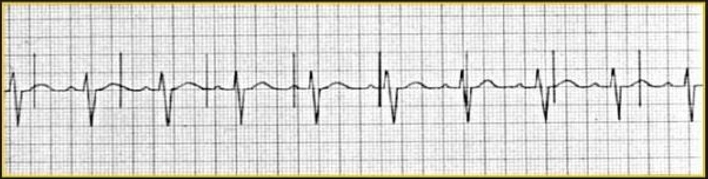
The rhythm strip reveals pacing spikes with appropriate sensing but loss of capture and ventricular escape. As shown in Figure 2, the first beat is a ventricular escape beat; then a pacer spike with no capture; then a second ventricular beat that is sensed, so there is no pacer spike; then a pacer spike with no capture; then a third ventricular beat that is sensed; then a pacer spike with no capture; then a fourth ventricular beat; then a pacer spike with no capture. The interval between these two pacer beats with no capture is 1 s, showing that the pacer rate is 60. The ventricular escape beats are very wide. This, along with maintenance of appropriate sensing, suggests the likelihood that loss of capture is not due to a problem with the pacer leads but rather to metabolic abnormalities (choice C is correct). Loss of capture in this patient was caused by severe acidosis with hypoxemia, which resolved after intubation and mechanical ventilation.
It is important to consider metabolic derangement when evaluating the failure of a pacemaker to capture. Since the primary disturbance is metabolic, methods of pacing such as transcutaneous pacing or insertion of a transvenous wire are likely to be ineffective. Chronotropic catecholamine agents such as isoproterenol or dobutamine are no more likely to work, may exacerbate hypotension, and can precipitate myocardial ischemia. Thus, the most important step in management is to address the underlying cause of the metabolic derangement.
Pacemaker lead fracture or dislodgement would be expected to affect both pacemaker sensing (with failure to sense diagnosed by pacer spikes where they do not belong) and capture, but in this case appropriate sensing is preserved (choices B and D are incorrect). In pacemaker generator failure, there would be no spikes at all (choice A is incorrect).