cardiology with critical care
mechanical ventilation
- Increasing oxygenation
- increase FiO2
- Increase PEEP, I:E ratio (increase alveolar recruitment)
- Decrease O2 consumption (increase sedation, analgesia, paralysis, synchrony)
- Minute Ventilation = RR X tidal volume
modes of ventilation
- AC: assist control. Specified volume or pressure for all breaths regardless whether patient or machine initiates breath
- default mode for most ICU
- volume control
- pressure control
- VC-CMV, continuous mandatory ventilation
- PC-CMV
- full respiratory support
- clinician control inspiratory pressure or volume
- tachypneic patient: air trapping or respiratory alkalosis, problem in asthma/copd
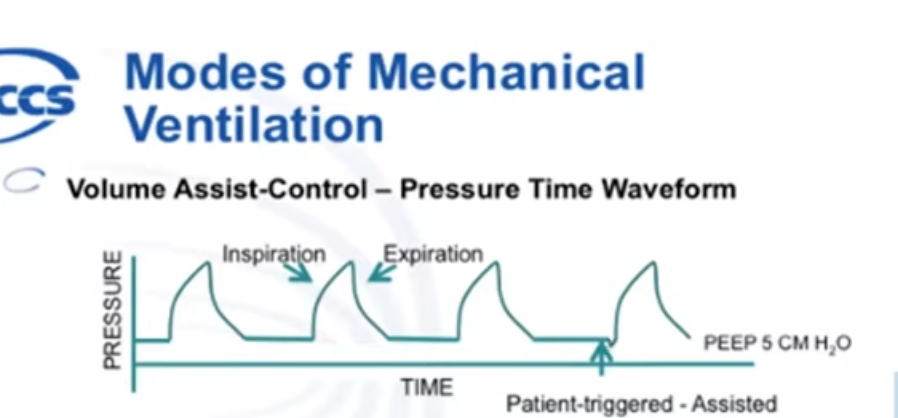
- 4th breath: deflection, triggered by patient
- SIMV: synchronized intermittent mandatory ventilation. Device gives pre-specified volume or pressure for set RR. Patient then takes spontaneous breaths in between
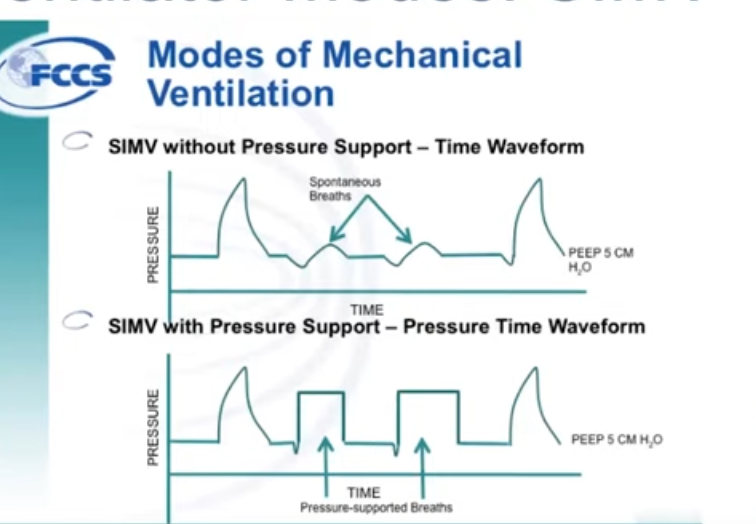
- pro: takes over full work of breathing, allows more spontaneous breathing, may help with weaning
- cons: patient fatigue if RR or pressure support too low
Initial Settings
- avoid ventilator induced lung injury
- volutrauma: lung overdistention
- barotrauma: high pressure
- atelectrauma: repeat opening/closing alveoli
- FiO2: 100% at first then reduce to 60% in 30 min to 1 hour if SpO2 > 88%
- RR: usually 14-18, or match pre-intubation RR
- Volutrauma: TV: 6-8 cc/kg for ideal body weight for height
- Barotrauma: PEEP: 5-10 cm H2O
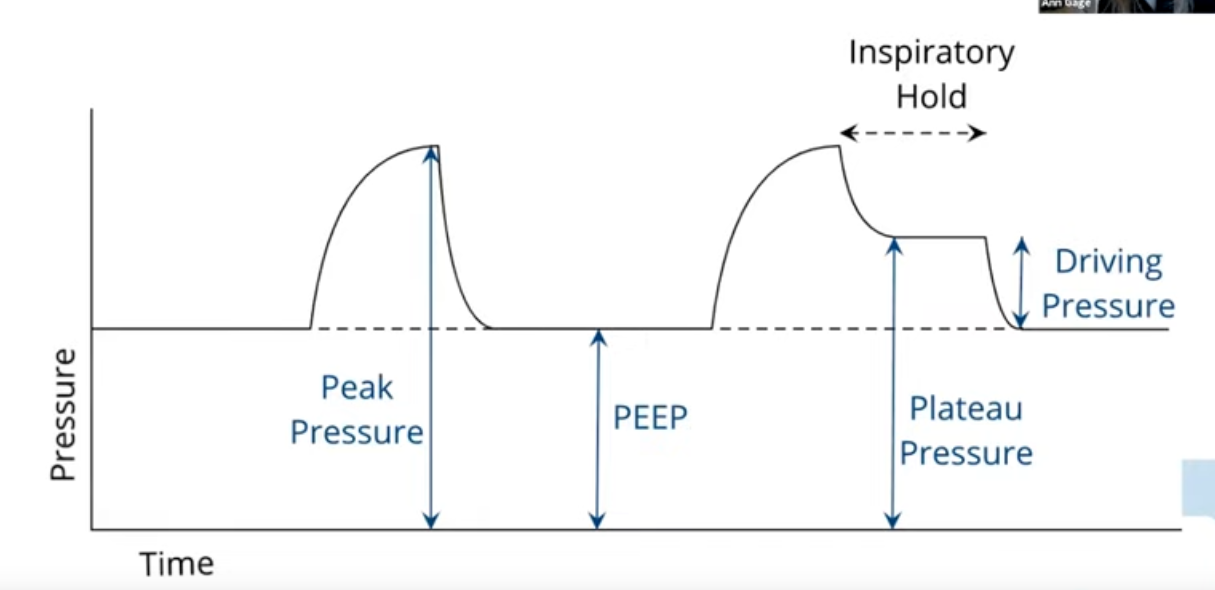
- Atelectotrauma: maintain plateau pressure < 30 cm H2O
- plateau pressure surrogate for transpulmonary pressure as pleural pressure negligible
ARDS
- acute lung injury from parenchymal or systemic process
- increased capillary permeability from damage to alveolar epithelium and capillary endothelium
- protein in alveoli = pro inflammatory cytokines => fibrosis => low compliance => hypoxemia
- Berlin definition
- acute onset injury
- CXR bilateral opacities
- non-hydrostatic pulm edema, not cardiogenic
- P:F ratio < 300
- mild: 200-300
- mod: 100-200
- severe: <100
- low plateau pressure
- permissive hypercapnia, pH > 7.25, do not have to get back to 7.4 with 40 CO2. Due to the magnitude of benefits from LTVV, it is sometimes recommended that bicarbonate drips be started temporarily to maintain an acceptable pH if needed, rather than making ventilator changes that would violate LTVV parameters.
- relative hypoxemia: spO2 88-94%, keep FiO2 < 60%
- start with volume control
- low tidal volume: 6cc/kg IBW
- PEEP: usually start with 8
- ABG 30-60 min after stabilization
- Then titrate:
- lower RR to target pH near 7.25
- FiO2: decrease to target 92-96% or PaO2 60 - 80
- Pplat: < 30 cm H2O
- if plateau > 30 and pH > 7.25: decrease TV
- if plateau > 30 and pH < 7.25: cautious decrease in PEEP
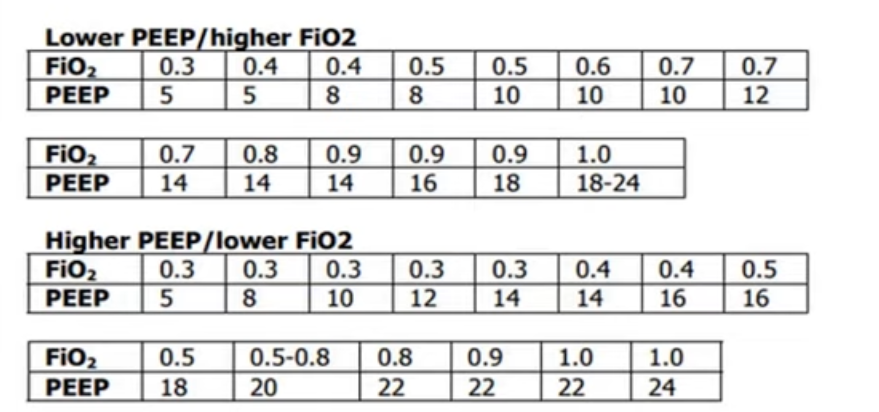
- PEEP
mechanical ventilation and hemodynamics
- spontaneous inspiration
- increase venous return => increase preload
- decreases pulmonary resistance => decrease RV afterload
- increase LV afterload
- positive pressure ventilation
- decrease venous return => decrease preload
- compress pulmonary vasculature => increase RV afterload
- LV afterload decreased
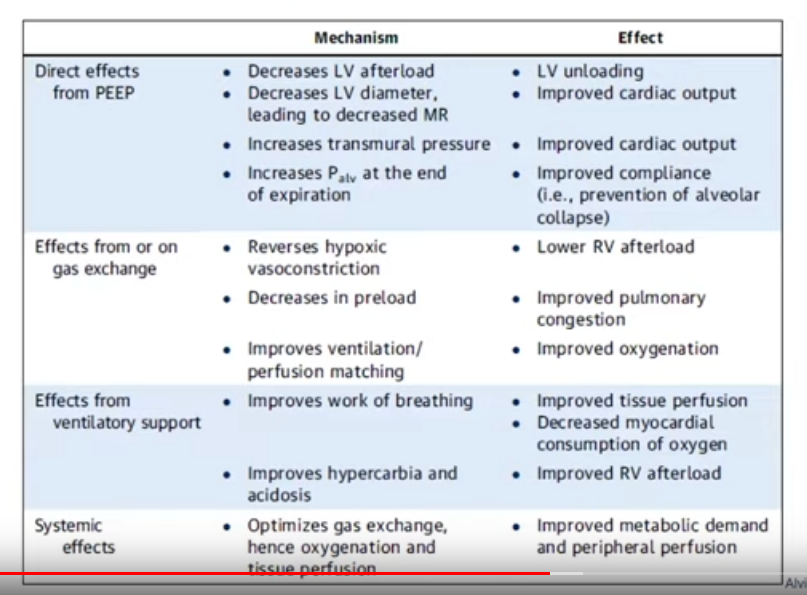
- PEEP can be bad for pt preload sensitive (RV dysfunction)
- PEEP decreases LV afterload: good for MR or dilated LV
- RV volume/pressure overload: pushes into LV, PEEP can cause less preload and less push into LV
vasopressors in ICU
- norepinephrine: a1 and small b1
- vasopressor: equivalent to epi and phenylephrine
- increases MAP without increase HR
- dopamine/epinephrine both increases HR
- less increase in cardiac O2 demand
- slight increase in CO with b1
- no b2, lactate not increased
- epinephrine
- a1, b1, b2
- low dose: 1-4 mcg/min. Increase CO, decrease SVR
- high dose: increase CO and SVR (SVR bad for heart)
- all dose: increase HR and O2 demand
- b2 increases lactate
- arrhythmia from b1 activity
- phenylephrine
- a1
- vasoconstriction, no inotropy, no chronotropy
- decrease SV but maintain CO with increase SVR
- good for LVOT obstruction
- better with arrythmia
- dopamine
- messy
- 1-2 mcg: D1, increase renal, mesenteric, cerebral/coronary vasodilation
- 5-10: variable. B1 and D1
-
10: alpha stimulation, increase SVR
- much higher atrial and ventricular arrhythmia
- higher death in cardiogenic shock patient
- vasopressin
- V1/V2, smooth muscle constriction
- septic shock: vasopressin goes up first but depleted in 24-48 hours
- no catecholamines => no effect in HR
- no increase in PVR => good for PHTN
-
0.06 may cause skin ischemia
- hypotension common with withdrawal, taper 0.01 every 30-60 min