CO2 capnography
- related: ICU intensive care unit
- tags: #literature #pulmonology
Capnography is the measurement of the partial pressure of CO2 in the exhaled breath over time. The maximum CO2 concentration at the end of each tidal breath (end-tidal, ET CO2) can provide information about ventilation and perfusion in patients in cardiac arrest undergoing cardiopulmonary resuscitation (CPR).
The increase in cardiac output with the return of spontaneous circulation (ROSC) causes rapid transport of CO2 accumulated in tissues during cardiac arrest to the lungs. This is detected as a sudden rise in EtCO2 on capnography and is the earliest indicator of ROSC, occurring even before a pulse can be palpated. This technology virtually eliminates the need to stop CPR to check for a palpable pulse, reducing interruptions in cardiac compressions.
In addition, recent studies have indicated that EtCO2 can help determine prognosis during cardiac arrest. Patients with an EtCO2 of ≤10 mm Hg after 20 minutes of CPR are highly unlikely to achieve ROSC.
Use of capnography has revolutionized monitoring during CPR. ETCO2 gives a measure of adequacy of resuscitation. For example, a decrease in ETCO2 may indicate that chest compressions have become less effective, perhaps reflecting operator fatigue. As noted, excessive ventilation can contribute to reduced perfusion and, thus, falling ETCO2. Capnography can assist in identifying the patient who has a very low likelihood of survival from cardiopulmonary arrest. Prospective studies indicate that ETCO2 of 10 mm Hg or less after 20 min of CPR is associated with very low likelihood of survival neurologically intact. ETCO2 is 16 to 18 mm Hg at 14/min (choice D is incorrect). Importantly, an abrupt increase in ETCO2 to >35 to 40 mm Hg is often the first indication that return of spontaneous circulation (ROSC) has been achieved. ETCO2 is 16 to 18 mm Hg; thus, capnographic criteria for ROSC have not been achieved (choice C is incorrect).
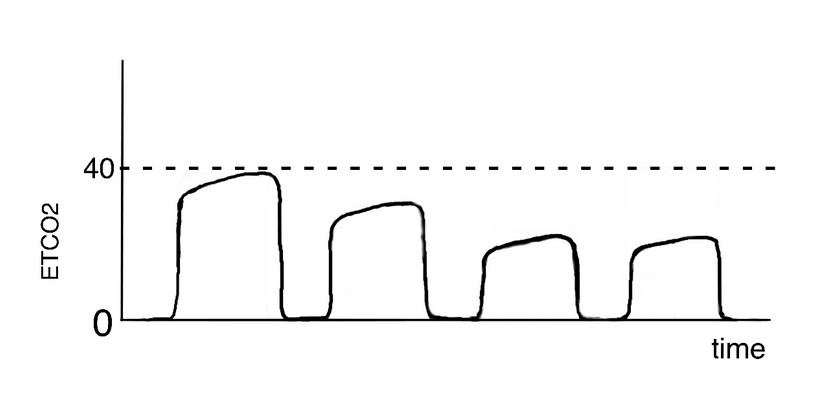
Air leaks around the endotracheal tube can lead to the dilution of end-expiratory CO2 gas and would be demonstrated on a capnogram as a rounded and decreased peak of the alveolar plateau phase (choice B is correct) (Figure 2). Common causes of air leaks around the endotracheal tube include cuff underinflation, displacement of the tube high up in the trachea, and high mean airway pressure. Structural defects to the cuff itself are also possible and may be caused by trauma (eg, teeth) or by manufacturing defects, although they are considered less likely. In the patient presented here, possible risk factors for the air leak included inadequate sedation and the need for frequent suctioning, which may have resulted in the cephalad movement of the endotracheal tube, and suspected high airway pressures due to ARDS. An underinflated cuff may have also been a factor, as the ideal endotracheal tube intracuff pressure has not been defined, nor have the optimal frequency and technique of pressure checks. The consequences of an air leak around the endotracheal tube can vary from the need for simple reinflation to an unplanned extubation or ventilator-associated pneumonia.
Bedside capnography monitoring provides information about alveolar ventilation, circulation, and cell metabolism and can be used to detect certain complications related to the endotracheal tube. The waveform of a capnograph plots the concentration of airway CO2 measured over the course of a respiratory cycle, and in the absence of disease and complications, has a square wave pattern as depicted in the first waveform of Figure 2. In the initial phase of expiration (Figure 2, line A), no CO2 is measured as the first gas sampled is from the conducting airways where no gas exchange takes place. The upstroke that follows (Figure 2, line B) represents progressively increasing amounts of CO2 coming from the alveoli, and as expired gas becomes primarily alveolar gas, it reaches a plateau that is flat with a slight upward tilt (Figure 2, line C). The end-tidal CO2 is measured at end expiration, which corresponds to the end of the plateau, just before the CO2 level falls. Under normal conditions, the difference between the PaCO2 and the end-tidal CO2 is 2 to 5 mm Hg, with the arterial CO2 greater than the exhaled CO2 because of the anatomical dead space. When the patient inhales, CO2 levels drop back to zero (Figure 2, line D). Alterations in the appearance of the curve may be due to physiological or pathological changes or may reflect the tubing or sensor.
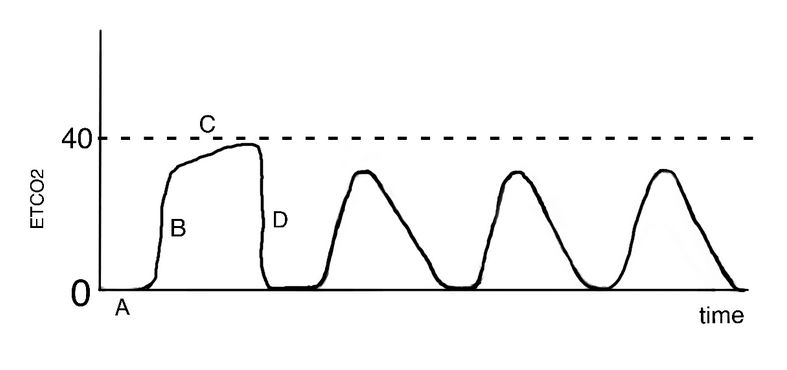
The capnogram of an esophageal intubation shows a rapidly steady decrease in CO2 concentration to a flatline trace (choice A is incorrect) (Figure 3) and is useful to help differentiate esophageal from tracheal intubation in the setting of a cardiac arrest. Small amounts of CO2 may sometimes be present initially when mask ventilation is used before intubation, whereby alveolar gas is essentially pushed into the esophagus and stomach.
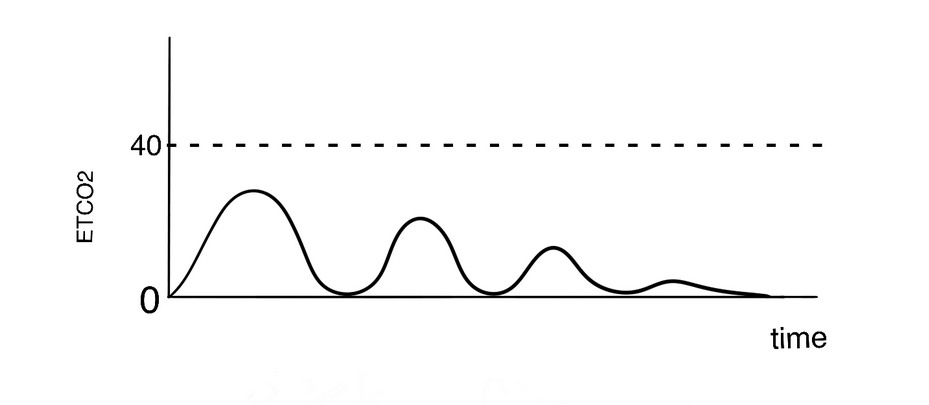
A kink in the endotracheal tube, or any obstruction in the airway, whether due to a foreign body or bronchoconstriction, will result in a less steep upstroke without an alveolar plateau, commonly described as a shark fin, and reflects the inhomogeneity of gas distribution and alveolar ventilation (choice C is incorrect). In a patient with asthma, the degree of bronchospasm is directly related to the reduced verticality of the upstroke (Figure 4).
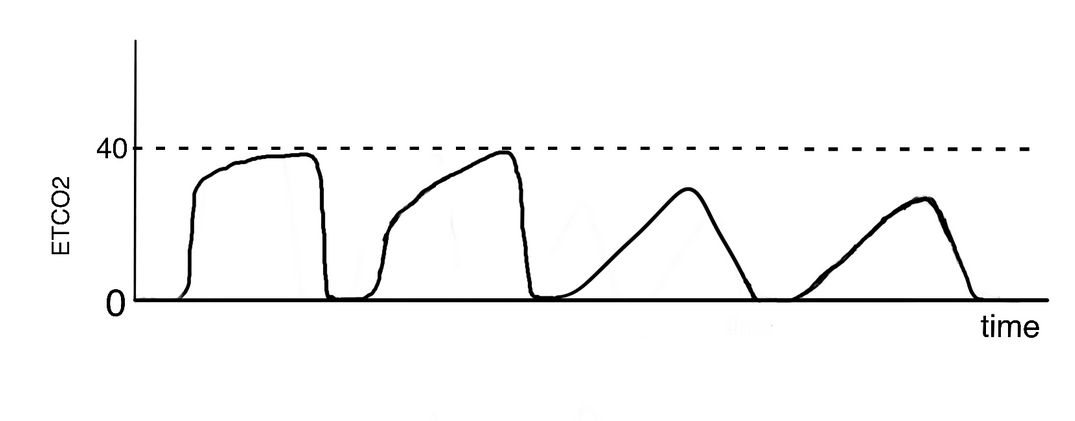
A drop in end-tidal CO2 but with a sustained square wave capnography trace may represent a sudden drop in pulmonary blood flow as can occur when there is a significant reduction in cardiac output or when a large pulmonary embolism causes marked reduction in pulmonary perfusion (choice D is incorrect) (Figure 5).
- esophageal intubation:
- ET tube kink:
- hemodynamic deterioration: