cryoptogenic organizing pneumonia chest imaging
- related: ILD Interstitial Lung Disease or Diffuse Parenchymal Lung Disease
- tags: #permanent
- source: MKSAP cryoptogenic organizing pneumonia
Chest X-ray for cryptogenic organizing pneumonia have bilateral patchy consolidative opacities that are sometimes recurrent or migratory.
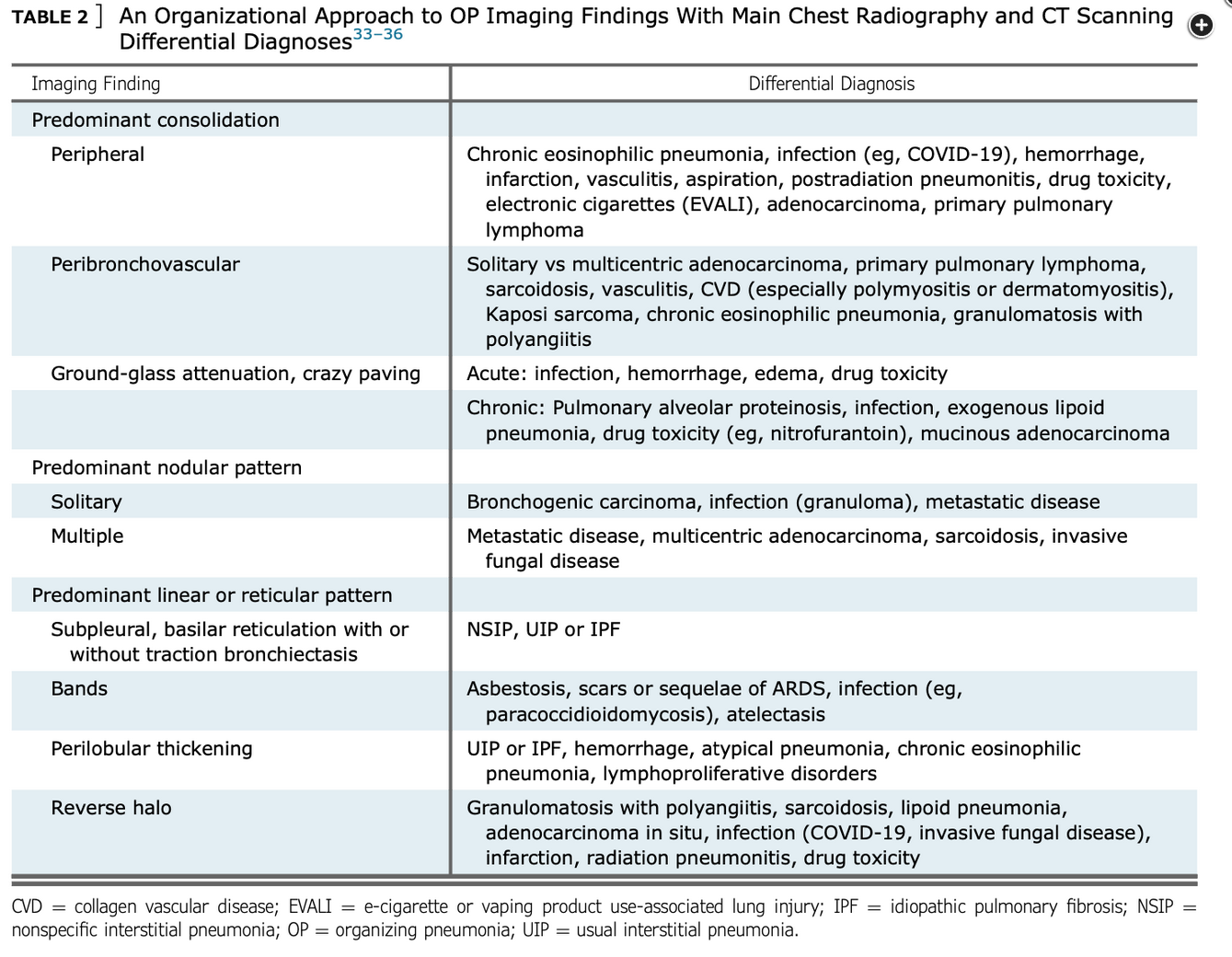
CT lung scan shows ground glass opacities more in periphery of lung and lower lung zones. Other patterns include bronchial wall thickening, air space consolidations, multiple nodules, reticular opacities in subpleural location.
Computed tomographic scanning — High resolution computed tomography (HRCT) lung scans are typically obtained to evaluate abnormalities seen on conventional chest radiographs. Rarely, a patient may have dyspnea and hypoxemia or a reduced diffusing capacity (DLCO) without a definite abnormality on chest radiograph, and an HRCT is obtained to evaluate the gas transfer abnormality. HRCT results are also used to guide site selection for patients undergoing bronchoalveolar lavage or lung biopsy.
HRCTs from patients with COP often reveal more extensive disease than expected from review of the plain chest radiograph. Radiographic patterns include patchy air-space consolidation, ground-glass opacities, small nodular opacities, and bronchial wall thickening with dilation (image 4). Patchy opacities occur more frequently in the periphery of the lung and are often in the lower lung zone.
Less common radiographic appearances include multiple nodules or masses that may cavitate, micronodules, irregular reticular opacities in a subpleural location, and crescentic or ring-shaped opacities. Rarely, a single nodule is the only manifestation of organizing pneumonia; this is termed focal organizing pneumonia (image 5). A retrospective study of 12 patients with biopsy-proven COP with a solitary lung mass showed that all lesions were subpleural, and in six the masses had a heterogeneous density; among these, four masses were cavitary. Lymphadenopathy was seen in seven patients. In a case series, mediastinal lymphadenopathy (diameter ≥10 mm in short axis) was reported in 6 of 16 patients with COP. Pleural effusion is uncommon.
Confident radiographic differentiation of COP from chronic eosinophilic pneumonia is frequently NOT possible, as both diseases have a predilection for the peripheral lung fields (image 6 and image 7). (See ‘Differential diagnosis’ below and “Overview of pulmonary eosinophilia”, section on ‘Chronic eosinophilic pneumonia’.)
Organizing pneumonia is a histopathologic response of the lung to a variety of infections, inhalational exposures, medications, and systemic illnesses. These include postbacterial pneumonia and SARS-CoV-2 infection, amiodarone pneumotoxicity, and the autoimmune idiopathic inflammatory myopathies. After thorough investigation, organizing pneumonia may be idiopathic (Figure 4) or cryptogenic. Patients with cryptogenic organizing pneumonia (COP) often present with a flu-like illness that includes cough, shortness of breath, night sweats, and weight loss. Although COP is generally quite responsive to corticosteroids, relapses may occur if the decrease in corticosteroid dose happens too quickly. A minority of patients with COP may require the addition of an immunosuppressive agent, but before starting this agent, a thorough investigation for an ongoing inhalational exposure, medication, or systemic autoimmune disease should be performed. The chest CT findings suggest that organizing pneumonia includes peripheral and basilar consolidation, patchy ground-glass opacities, and single or multiple lung nodules. Less commonly, the characteristic pathologic finding of organizing pneumonia—polypoid plugs of loose connective tissue extending into the alveoli—may be present in response to malignancy, including lung cancer and lymphoma (Figure 5).
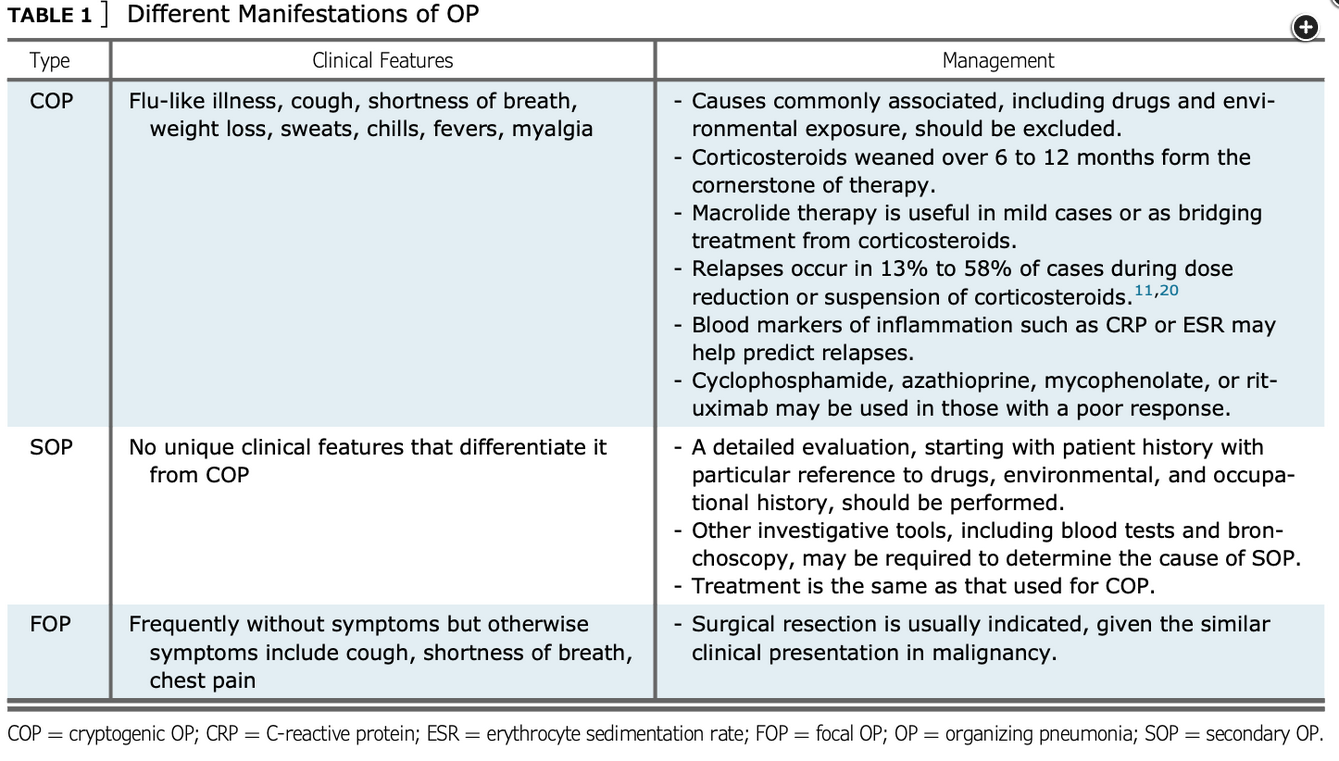
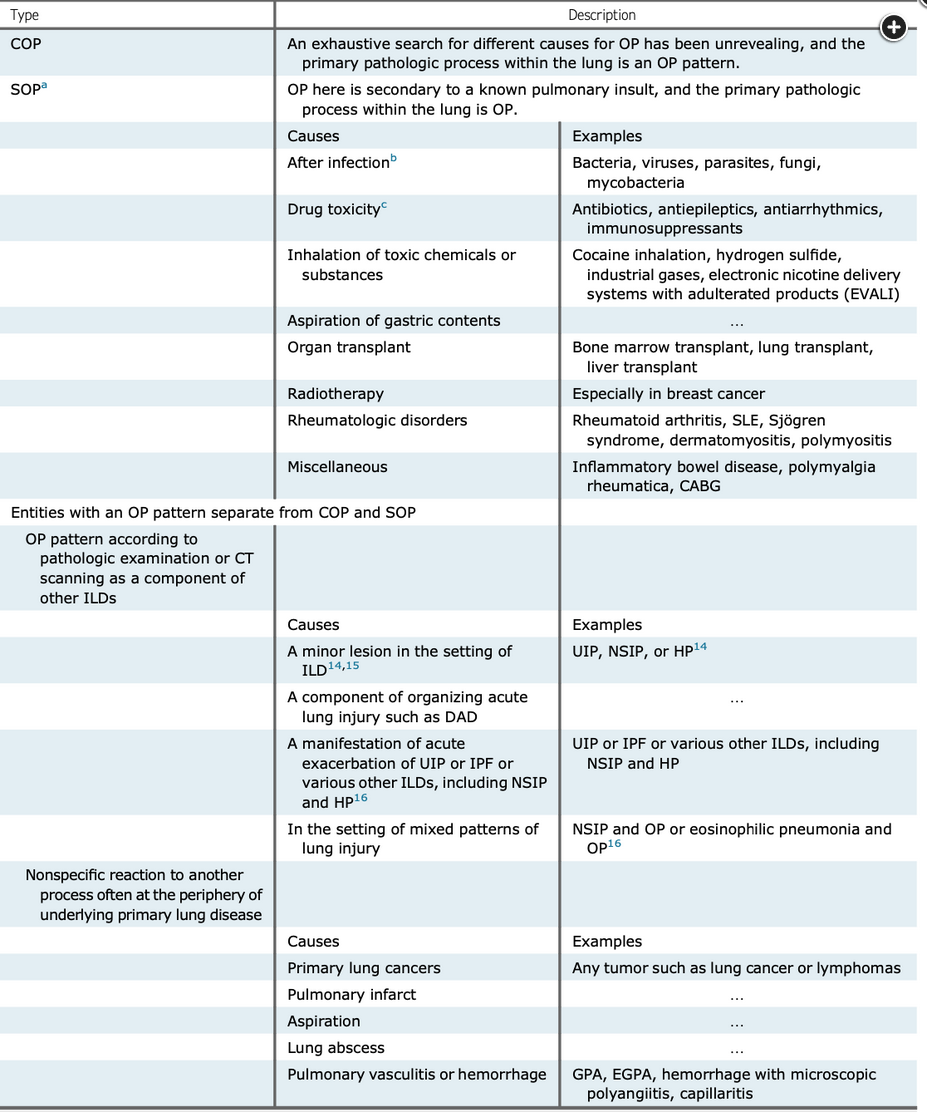
Classification of organizing pneumonia. Abbreviations: CABG, coronary artery bypass graft; ILD, interstitial lung disease; HP, hypersensitivity pneumonitis; DAD, diffuse alveolar hemorrhage; GPA, granulomatosis with polyangiitis; EGPA, eosinophilic GPA.
Figure courtesy of Cherian SV, Patel D, Machnicki S, et al. Algorithmic approach to the diagnosis of organizing pneumonia: a correlation of clinical, radiologic, and pathologic features. Chest. 2022;162(1):156-178.