cyanide poisonings
- Keywords: Step 3, Medicine, General Medicine
Cyanide
Cause
- Cause: house fire, smoke inhalation injury, nitroprusside use in hypertensive emergency
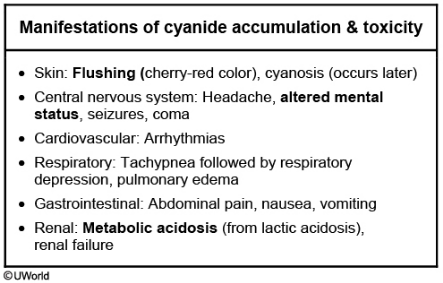
- Sx:
- early: neurologic and cardiorespiratory stimulation, and patients develop headache, vertigo, dizziness, hyperventilation, tachycardia, nausea, and vomiting.
- late: coma, seizures, bradycardia, hypotension, and cardiorespiratory arrest. HCN can also cause anoxic brain injury leading to permanent neurologic deficits.
- reddish skin discoloration (cherry red skin), tachypnea, headache, and tachycardia, often accompanied by nausea/vomiting, confusion, and weakness. Symptoms develop rapidly and can quickly progress to seizures and cardiovascular collapse.
- diagnosis: Laboratory studies indicate severe lactic acidosis in conjunction with a narrowing of the venous-arterial PO2 gradient, resulting from the inability of tissue to extract arterial oxygen.
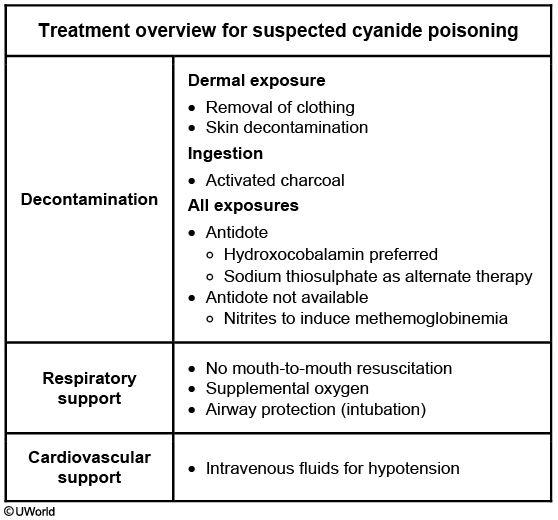
- treatment:
- direct binders: Hydroxycobalamin (b12), sodium thiosulfate
- induce methemoglobin: nitrites increase Fe3+ that binds to cyanide
This patient’s symptoms suggest acute cyanide toxicity in the setting of renal failure and nitroprusside use. Nitroprusside is a potent vasodilator that works on both arterial and venous circulation and is used for hypertensive emergency management. It has rapid onset and offset of action. The most important side effect is cyanide accumulation and toxicity.
Patients with chronic renal failure or those receiving a high-dose or prolonged infusion of sodium nitroprusside are at increased risk for cyanide toxicity. As a result, low infusion rates (<2 µg/kg/min), short-term usage, and close monitoring are recommended. Treatment involves cessation of nitroprusside and administration of sodium thiosulfate.
Cyanide is a potent inhibitor of cytochrome oxidase a3 in the mitochondrial electron transport chain. It binds to ferric iron (Fe3+), inhibiting its reduction to ferrous iron (Fe2+) and blocking production of ATP from oxidative phosphorylation. Cells then switch to anaerobic metabolism, leading to lactic acid formation and causing metabolic acidosis. Serum bicarbonate levels fall in an attempt to buffer excess acid. Metabolic acidosis also triggers central and peripheral chemoreceptors, increasing alveolar ventilation and then presenting as tachypnea. This leads to a fall in arterial PCO2 (PaCO2).
A 38-year-old African American man comes to the emergency department after experiencing severe back pain for the past 2 days. He has a history of hypertension for the last 5 years. His current medications include hydrochlorothiazide, amlodipine, and valsartan. The patient has a 15-pack-year history and drinks 4-5 bottles of beer daily. His temperature is 36.7 C (98 F), blood pressure is 230/112 mm Hg, and pulse is 84/min. Funduscopic examination shows arteriolar wall thickening and occasional cotton-wool spots. The rest of the examination is within normal limits. Initial laboratory studies show serum blood urea nitrogen of 28 mg/dL, potassium of 5.1 mEq/L, and serum creatinine of 2.3 mg/dL. Transesophageal echocardiogram is consistent with dissection in the descending aorta. The patient is admitted to the coronary care unit and started on intravenous labetalol and nitroprusside infusion. The next morning, the nurse finds him confused and agitated. He then has a generalized tonic-clonic seizure. His temperature is 36.7 C (98 F), blood pressure is 176/99 mm Hg, and pulse is 102/min. Physical examination remains otherwise unchanged.
Which of the following is the most likely diagnosis?