diabetes inpatient management
- related: Endocrinology
- tag: #note
- Discontinue oral hypoglycemics, especially metformin & sulfonylureas
- Basal Bolus insulin regimen is the preferred guideline driven inpatient regimen
- Inpatient BG goal: 140-180 mg/dL pre-prandially, without severe or recurrent hypoglycemia. ebm NICE-SUGAR trial
- If a patient is having hypoglycemia, they have no BG targets, other than resolving the hypoglycemia.
- Total daily dose (TDD) = basal + prandial + correction
1. Assess Basal Insulin Dose
- Goal of basal insulin is to hold BG stable in fasting state
- Goal is not to correct hyperglycemia or cover food
- Thus, bedtime BG and AM BG should be the same
- most people need less bolus and more prandial
- Total basal dose (TBD) = 0.4 x TDD
- T1DM: TBD = 0.273 x TDD
- Calculate change between bedtime BG and fasting AM BG
- if AM BG has increased by >15-20% compared to bedtime, increase basal insulin dose
- if AM BG has decreased by >15-20%, decrease basal insulin dose
- if AM BG is within 15-20% of bedtime BG, basal insulin dose is correct (even if both readings are above goal because that means the dinner dose of lispro is too low)
- Dose Lantus usually 8PM for easier management in am. Alternatively, dose BID
- Change Lantus dose based on BG:
- BG in 100s: change by 10%
- 200s: 20%
- 300s: 30%
2. Assess Prandial Insulin Dose
- Patient is eating => give standing prandial insulin, do not use SSI only
- work backwards in time to alter pre-prandial BG readings
- To change bedtime BG, raise or lower pre-dinner prandial lispro dose
- To change pre-dinner BG, adjust pre-lunch prandial lispro dose
- To change pre-lunch BG, adjust pre-breakfast prandial lispro dose
- Change dose 10-20%
3. Assess Corrective Insulin Dose
- is corrective insulin correcting hyperglycemia? If not, the increase correction scale
The 4 things that go into a patient’s BG at any given time:
- Medication on board
- Food ingested (or TF or TPN)
- Activity (or lack thereof)
- Stress (physical stress of illness and in some cases, psychological stress)
Important questions to ask the patient &/or nursing when trying to figure out daily BG patterns:
- Did you eat a bedtime snack or eat overnight?
- Did you NOT eat bedtime snack or eat overnight?
- Did you walk 50 laps around the unit yesterday?
- Was the food gross? Was the food delicious?
- Was the pt made NPO?
- Missed insulin doses? Mistimed insulin doses?
- Mistimed POC BG? Missed POC BG?
- Bedtime or middle of the night correction insulin given?
- Tube Feeds turned off or on?
Cases
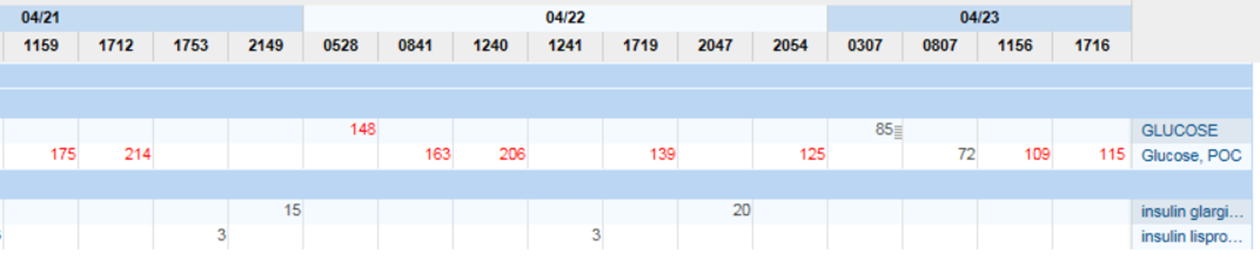
- no night time BG available
- should decrease basal bolus
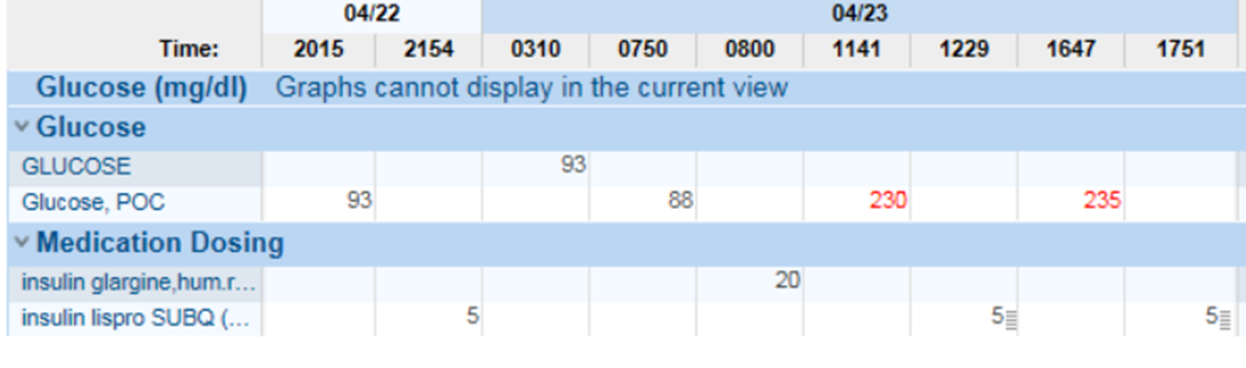
- hyperglycemia at lunch time because AM prandial dosing was held
- nurse did not give AM insulin because BG 88 in the morning
- decrease basal to bring BG 140-180
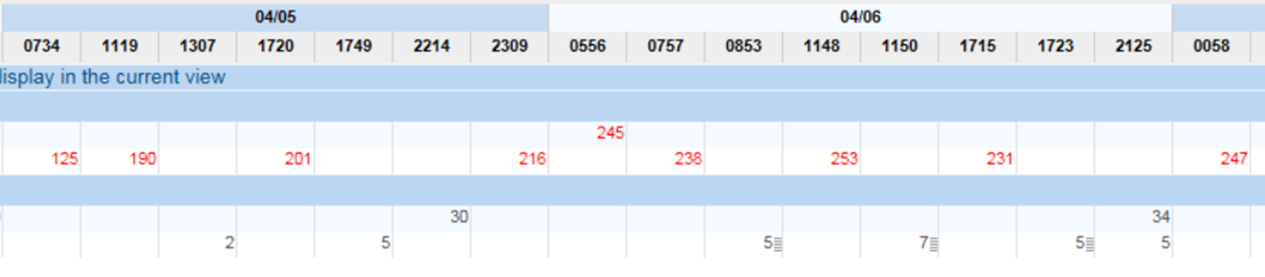
- basal bolus adequate
- prandial dose need to go up
Resources
- The 2021 ADA Standards of Care section on Inpatient Glycemic Mgmt: https://care.diabetesjournals.org/content/44/Supplement_1/S211
- The Endocrine Society guidelines for inpatient glycemic mgmt. (Umpierrez is the guru of inpatient glycemic mgmt.): https://academic.oup.com/jcem/article/97/1/16/2833111