diagnose idiopathic hypersomnia with MSLT and actigraphy
- related: Sleep and Sleep Disordered Breathing
- tags: #literature #pulmonology
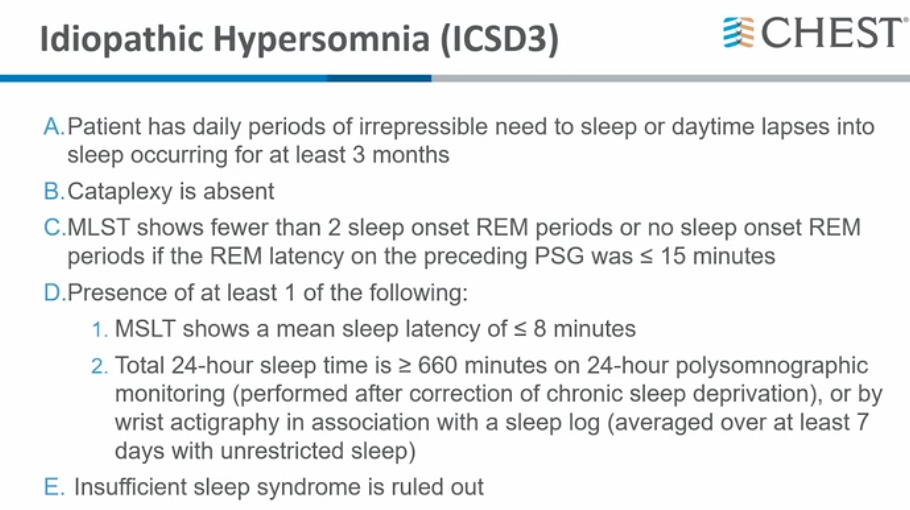
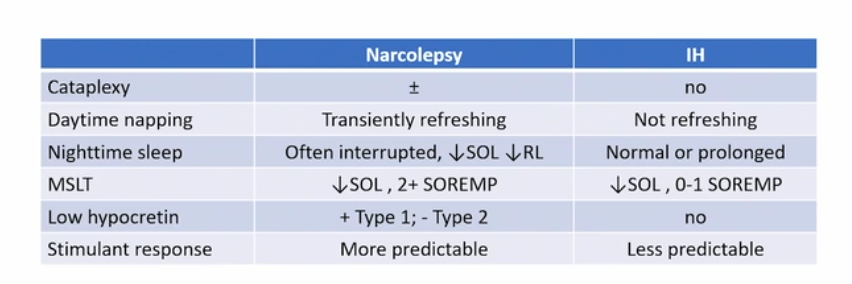
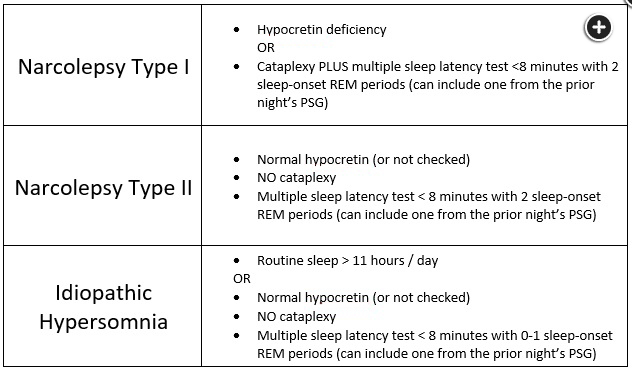
Idiopathic hypersomnia is a sleep disorder in which the patient has excessive daytime sleepiness often accompanied by long nocturnal sleep durations, long daytime naps, and sleep inertia. Many patients will also have autonomic manifestations. In contrast to narcolepsy, patients will note that sleep is never refreshing and they typically do not have cataplexy, sleep paralysis, or other REM-related phenomenon. While the MSLT is the gold standard to differentiate idiopathic hypersomnia from narcolepsy, a secondary criteria to diagnose idiopathic hypersomnia is documentation of prolonged sleep, ie, >11 hours of sleep in a 24-hour period. Some sleep laboratories have protocols in which they monitor patients for a full 24 hours, but this is not covered by insurance and is labor intensive. Many sleep labs deploy actigraphy for 1-2 weeks prior to the MSLT and, if 11/24 hours of sleep is documented, that can also qualify.
While an elevated Epworth is useful to assess the degree of sleepiness, it is nonspecific and not diagnostic. Sleep efficiency on a polysomnogram is the percentage of time the patient slept divided by the time of the recording. While idiopathic hypersomnia patients may often have a high sleep efficiency, it is also not diagnostic. Finally, a maintenance of wakefulness test is typically used to assess for ability to stay awake in a patient who may have a safety sensitive job but it is not used to make a diagnosis in hypersomnia disorders.
The differential diagnosis for patients presenting with excessive daytime somnolence is broad and includes inadequate sleep time, disrupted sleep quality, fatigue due to medications or other medical or psychiatric disorders, and central disorders of hypersomnolence. Disrupted sleep quality can be further subdivided into external and internal contributors. External contributors are typically environmental noise and/or light, while internal contributors include sleep-related breathing disorders, as well as other physiologic causes of frequent arousals from sleep. Making a definitive diagnosis of a central disorder of hypersomnolence typically requires excluding other contributors to diurnal fatigue.
The evaluation of the patient complaining of hypersomnolence will vary among patients, depending upon the initial assessment. If the history clearly suggests inadequate sleep time due to behavior or insomnia, it is likely that additional work-up can be foregone until that problem is addressed. If environmental contributors seem to be driving the complaint, then focusing on those issues would be appropriate. Asking about the use of prescription medications or illicit substances that can contribute to hypersomnolence, and reviewing comorbidities to ensure that there are no other diseases likely to be causing the symptoms, are both appropriate. Patients with complaints suggesting obstructive sleep apnea can often be evaluated with home sleep apnea testing as the first-line evaluation.
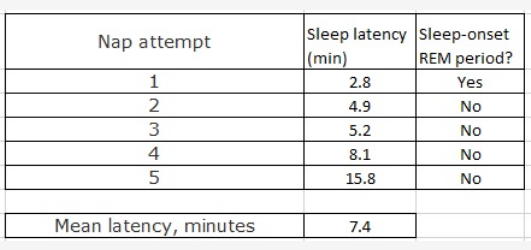
However, when the history and physical are less revealing, a more thorough work-up is generally required. In general, this should include some measurement of sleep duration at home (either sleep logs or actigraphy) followed by in-laboratory PSG and MSLT. Several studies have suggested that sleep logs tend to correlate quite well with actigraphy. It is imperative that all of these data be collected in a temporally adjacent fashion in order to allow complete interpretation of the test results. This patient had PSG and MSLT performed but did not have any preceding measurement of routine sleep time at home. In addition, several findings on the tests that were performed suggest a likely diagnosis of inadequate sleep time at home, despite the patient’s report to the contrary; both the elevated degree of Stage N3 sleep and the progressive prolongation in sleep latency over the span of the five MSLT naps suggest prior sleep deprivation. Therefore, it would be appropriate to repeat the data collection with preceding actigraphy or sleep logs before making a formal diagnosis (choice D is correct). Had the patient’s home sleep assessment confirmed a diagnosis of inadequate sleep time, the need for additional testing would have been obviated.
Occurrences of patients inappropriately labeled as having a central disorder of hypersomnolence (and subsequently treated with stimulant therapy) are increasingly common due to incorrect testing protocols or misunderstanding of the diagnostic requirements. Narcolepsy type 1, narcolepsy type 2, and idiopathic hypersomnia all have formal diagnostic criteria.