different lung volume testings
- related: PFT and lung functions
- tags: #literature #pulmonology
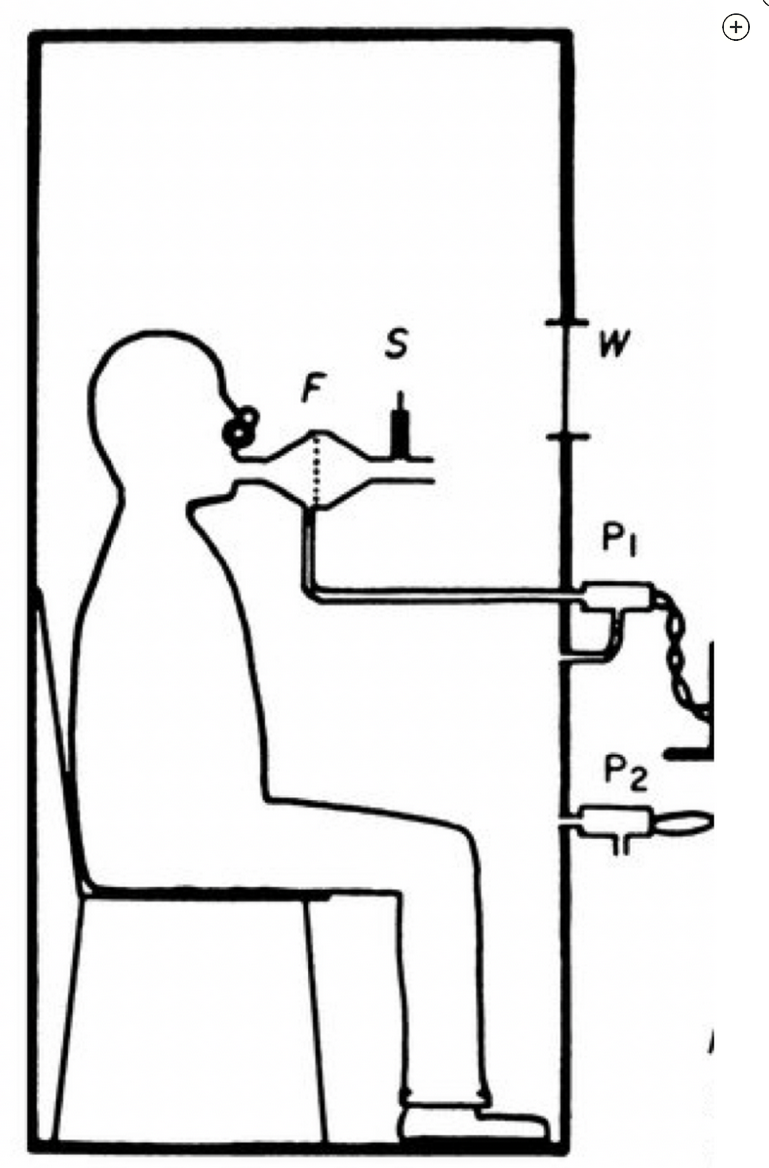
The most accurate method of measuring lung volumes is plethysmography, which uses Boyle’s law to calculate lung volumes (see Figure 4). Boyle’s law describes the relationship between pressure (P) and volume (V) of a confined gas using the formula . According to Boyle’s law, at a constant temperature, the product of pressure and volume within a closed system is constant. In a plethysmograph, the patient sits inside a sealed chamber, closing their lips tightly around a mouthpiece. At end expiration during tidal breathing (functional residual capacity [FRC]), the mouthpiece is closed. The patient is then asked to make a panting inspiratory effort. During this maneuver, the lungs expand, decreasing pressure within the lungs and increasing lung volume. Such a maneuver increases the pressure within the box since it is a closed system. Simultaneously, the volume of the plethysmograph box itself decreases to accommodate the new volume of the patient. The volume of the whole plethysmograph is known (), and barometric pressure () can be measured precisely with a barometer. can be measured at the mouth during the panting maneuver at FRC, which is calculated as follows: , where is barometric pressure. Total lung capacity (TLC) is easily calculated once FRC is known, since it is equal to inspiratory capacity (IC) plus FRC. IC is equal to tidal volume (Vt) plus inspiratory reserve volume (IRV), both of which can be measured directly with spirometry. Likewise, residual volume (RV) can be easily calculated once FRC is known, since it is equal to FRC minus expiratory reserve volume (ERV) (see Figure 5).
This patient’s PFT used the nitrogen washout technique, rather than plethysmography. The principle behind the nitrogen washout technique is that the initial amount of nitrogen in the lungs must equal the total amount of nitrogen ultimately exhaled. Nitrogen washout measurement uses a gas dilution technique, which is notoriously inaccurate in patients with obstructive physiology. The reason for this problem is that nitrogen washout underestimates FRC in poorly ventilated lung regions that still contain nitrogen at the end of the washout test. This same limitation is seen with the helium dilution technique. When measured by plethysmography, this patient’s TLC was 125% predicted. Thus, she does not have restrictive lung disease (choice B is incorrect).
DLCO is a measure of pulmonary capillary surface area, and the differential diagnosis for reduced DLCO is broad. Reduced DLCO is seen in emphysema, many types of interstitial lung disease, many types of pulmonary vascular disease processes (including pulmonary embolism), and anemia of any cause. In this case, the presence of emphysema on HRCT, the absence of restrictive lung physiology, and the absence of substantial risk factors for pulmonary embolism all make the reduced DLCO most likely the result of emphysema (choice C is incorrect).
As mentioned in the discussion about nitrogen washout above, this patient does not definitely have restrictive lung disease based on the nitrogen washout measurements. Respiratory bronchiolitis-interstitial lung disease (RBILD) shows a mixed obstructive-restrictive pattern on PFTs, with mild to moderate reduction in DLCO. The mixture of obstruction and restriction is due to airway inflammation from tobacco use (obstruction) and interstitial disease associated with RBILD (restriction). Furthermore, the HRCT scan is not consistent with RBILD. With RBILD, the HRCT scan would show bronchial wall thickening, centrilobular nodules, ground-glass opacities, and sometimes upper lobe centrilobular emphysema (choice D is incorrect).