Entamoeba Histolytica
Entamoeba infection
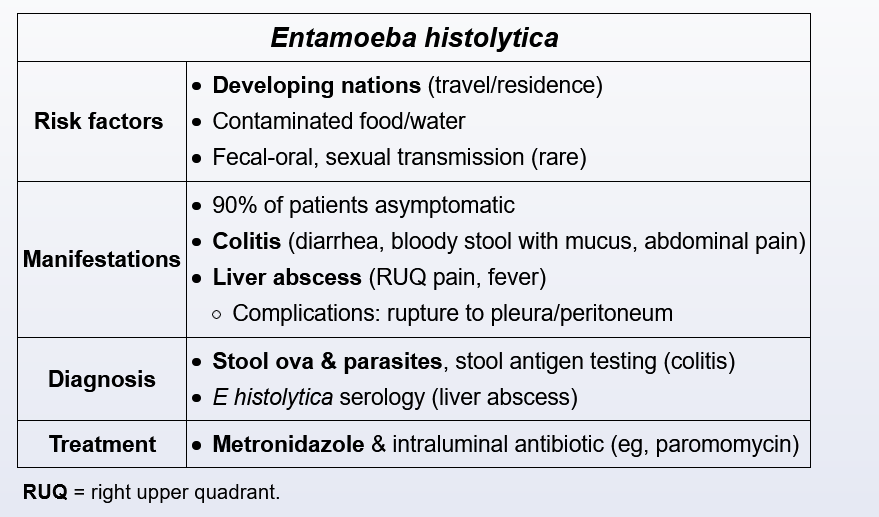
This patient who recently spent several weeks in South America has fever, right upper quadrant pain, and a hypoechoic liver lesion indicating likely extraintestinal Entamoeba histolytica.
E histolytica is a protozoa transmitted via the ingestion of contaminated food or water. Prevalence is high in regions with poor sanitation; carriage rates approach 50% in parts of India, Africa, Mexico, and Central/South America. Although the majority of infections are asymptomatic, approximately 10% develop amebic dysentery or, more rarely, extraintestinal disease of the liver, lung, heart, or brain.
Amebic liver abscess is the most common manifestation of extraintestinal disease. Risk is greatest in men in the fourth or fifth decade of life with underlying cirrhosis or alcoholic hepatitis (as this possibly allows for easier seeding of the liver with organisms). Manifestations typically begin 8-20 weeks after inoculation and include fever, right upper quadrant pain, and nonspecific symptoms (eg, malaise, nausea). A recent history of dysentery is present in <35% of patients.
Imaging usually reveals a round, well-defined hypoechoic mass in the right hepatic lobe. Diagnosis is made with blood serology and antigen detection; aspiration is not required but is often performed if a cyst is large (rupture risk) or if an alternate diagnosis requires exclusion. Aspirate typically resembles “anchovy paste” and is often aseptic with a negative Gram stain.
Hydatid cysts are due to the tapeworm Echinococcus granulosus. Cysts tend to grow slowly over years and remain asymptomatic until the size is >10 cm. Fever is rare without cyst rupture.
Pyogenic and amebic liver abscesses often result in similar clinical and radiographic pictures. Differentiation is typically made using E histolytica serologic or antigen testing for those with possible exposure. If testing is negative or uncertainty remains, fine needle aspiration can usually differentiate the etiology; pathogens that cause pyogenic liver abscess are usually identified by culture and Gram stain of aspirate fluid (unlike in this patient).