excessive daytime sleepiness EDS
- related: Sleep and Sleep Disordered Breathing
- tags: #literature #pulmonology
While excessive daytime sleepiness (EDS) is one of the cardinal symptoms of OSA, and improvement with therapy is the norm, studies suggest that residual sleepiness in patients adequately treated with CPAP may be as high as 13%, as assessed by a persistent elevation in ESS score. Risk factors for persistent EDS include female sex, a greater degree of pre-treatment sleepiness, and evidence of comorbid depression.
The first step in the evaluation of persistent EDS in these patients is to ensure that treatment for OSA is being used for a sufficient number of hours and is providing adequate relief of disease. Frequently, this information can come directly from the CPAP adherence download, which will contain data on hours of use, degree of residual disease, and adequacy of mask fitting. Abnormalities identified in any of these data points should be addressed with the patient; behavioral therapy, or modifications of CPAP settings or interface may be appropriate in these cases.
If CPAP adherence and effectiveness are deemed to be adequate, consideration should be given to alternate pathologies that can contribute to complaints of fatigue; these could be either medical or psychiatric disorders, as well as side effects from pharmacotherapy being used to treat these disorders. If no alternative explanation can be identified, consideration could be given to reevaluation with polysomnography (to evaluate for alternative intrinsic sleep pathology that might be disrupting sleep) or multiple sleep latency testing (to evaluate for narcolepsy).
Several randomized controlled trials have shown that wake-promoting agents such as modafinil and armodafinil can further improve daytime sleepiness in patients with OSA who are highly adherent to CPAP therapy. This improvement in daytime sleepiness leads to improvement in quality of life, without inducing insomnia (choice D is correct). Modafinil promotes wakefulness by inhibiting dopamine reuptake, leading to an increase in dopamine in the CNS. If taken late in the afternoon, modafinil can induce insomnia. Headache and nausea can occur but tend to subside in a few days. In contrast to stimulants (eg, methylphenidate), wake-promoting agents like modafinil do not have a major effect on increasing the BP or heart rate. In premenopausal women, modafinil and armodafinil render oral contraceptives ineffective. Therefore, in such patients, other wake-promoting agents should be considered (eg, solriamfetol), or the patient should be advised to use a more effective method of contraception.
Modafinil is typically started at 100-200 mg daily and can be increased to a maximum of 400 mg daily; armodafinil is usually initiated at 150 mg daily and can be increased to 250 daily.
In the case presented, modafinil therapy would be the most appropriate option of the answer choices provided (choice A is correct). Review of CPAP adherence demonstrates an adequate number of hours of use, very little large leak (choice B is incorrect), and minimal residual disease. While reports of intermediate AHI levels from CPAP downloads may be difficult to interpret, current guidelines support using either very high or very low levels of residual disease as a solid basis for clinical decision making; in this case, the low residual AHI suggests no need for a retitration. While consideration could be given to looking for alternate pathologies by repeating polysomnography, there would be no indication to start CPAP at a subtherapeutic level (choice C is incorrect).
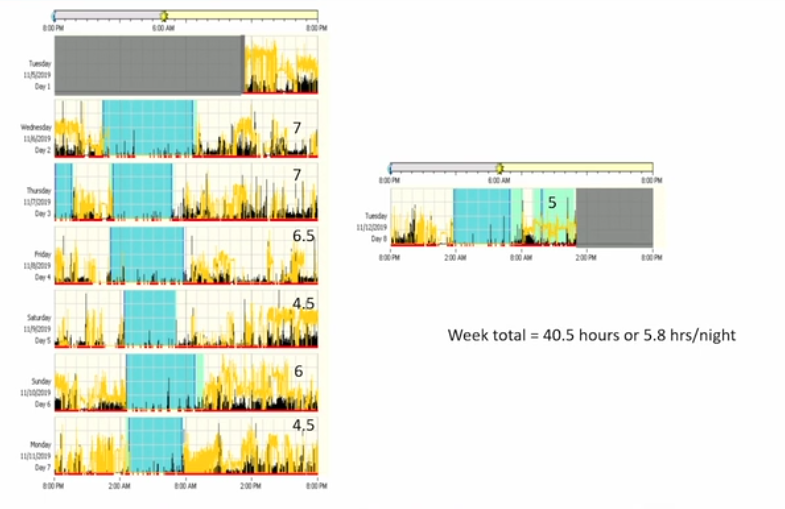
Wrist actigraphy can be useful in estimating total sleep time when there is a concern for insufficient sleep or certain circadian rhythm disorders. However, in the current case, there is no suggestion of short sleep duration or circadian rhythm disorders (choice D is incorrect).
- most common reason for EDS
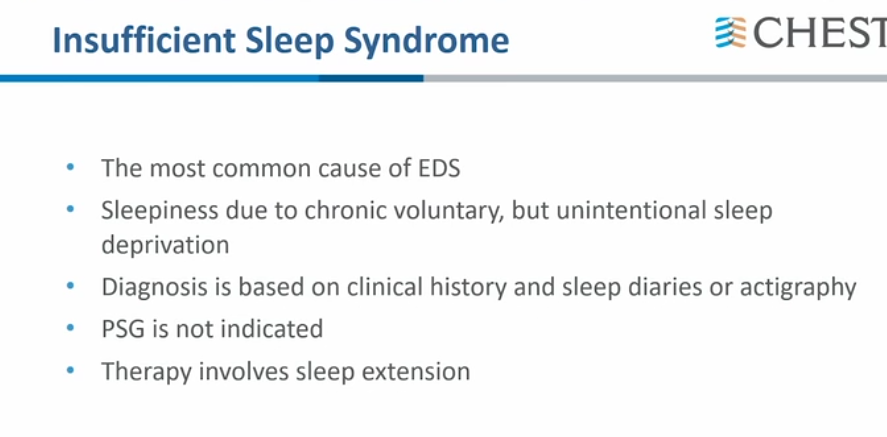
- actigraphy to see if getting enough sleep
- need to sleep more