GI chest 2025
- related: GI gastroenterology
- tags: #literature #GI
- GI bleed
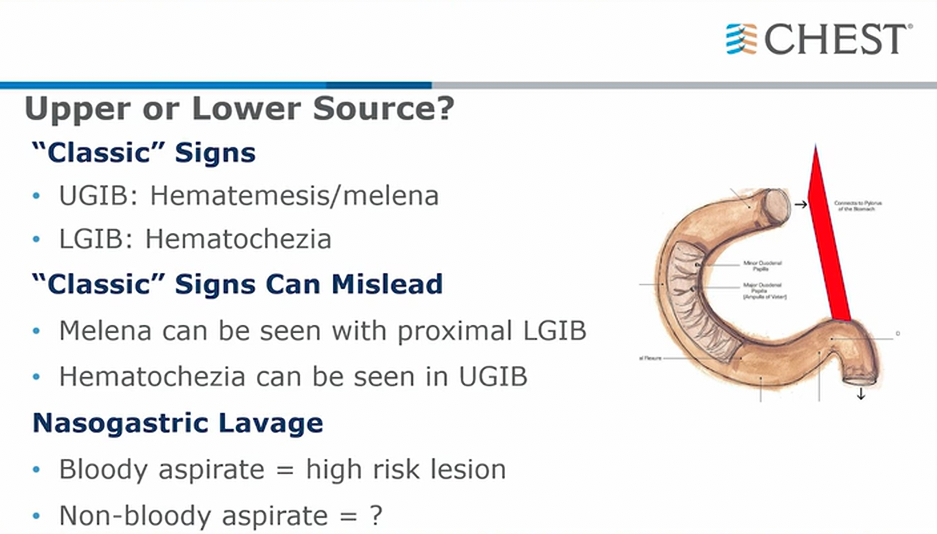
- classically, ligament of Treitz is used to differentiate between upper and lower GI bleed
- positive bloody aspirate can help decrease suspicion for lower GI bleed
- non bloody aspirate is not necessarily a rule out. Duodenal ulcers may not reflux blood into stomach
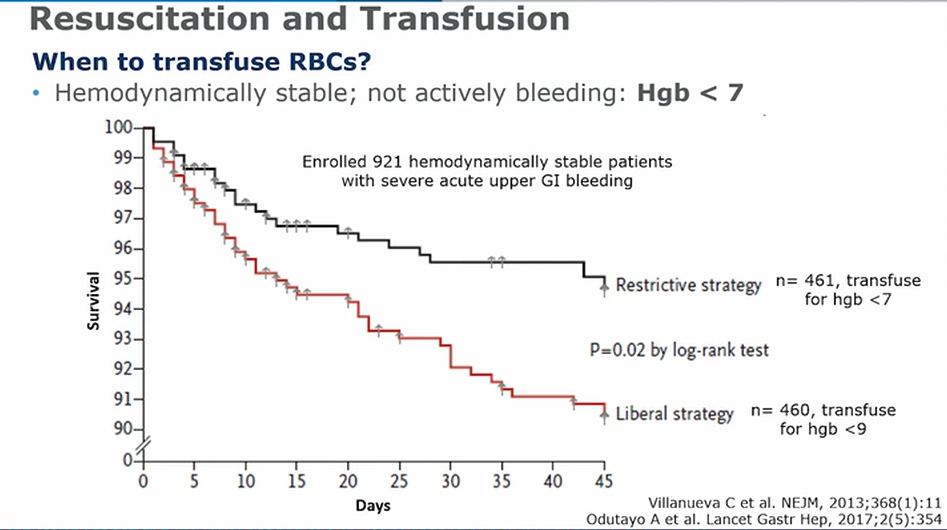
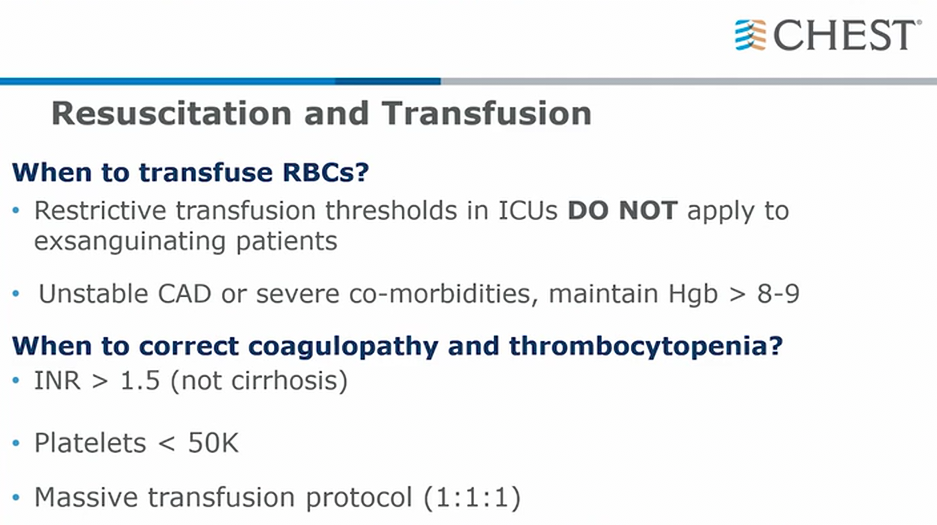
- if unstable: transfuse
- if stable use goal of 7, except for CAD patients (MINT study)
Risk
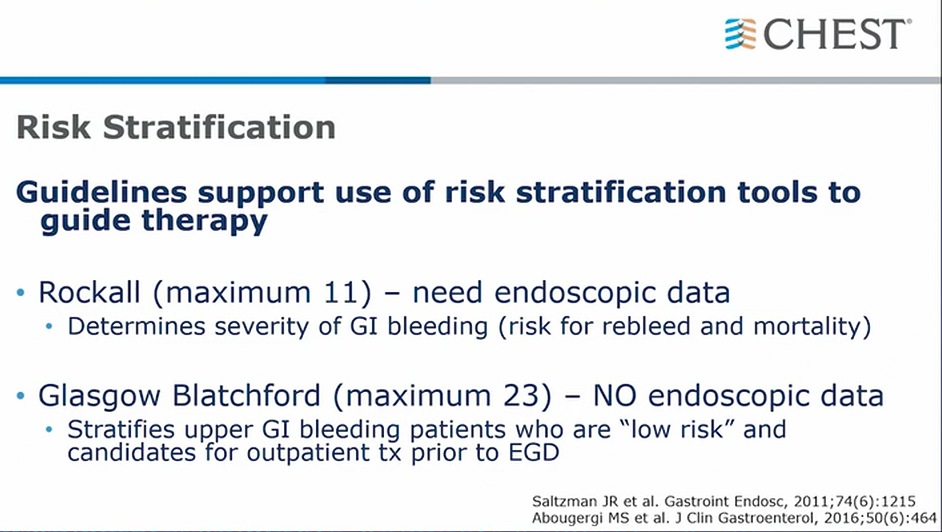
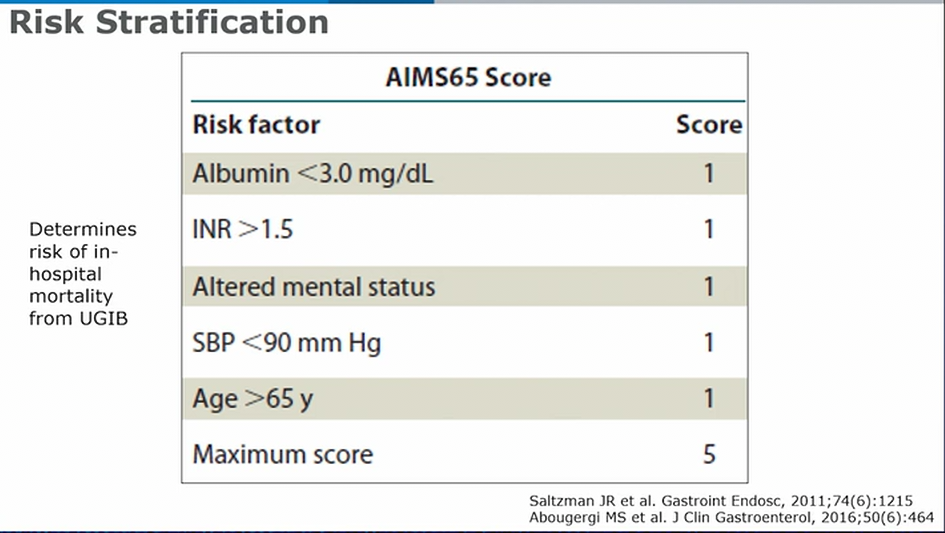
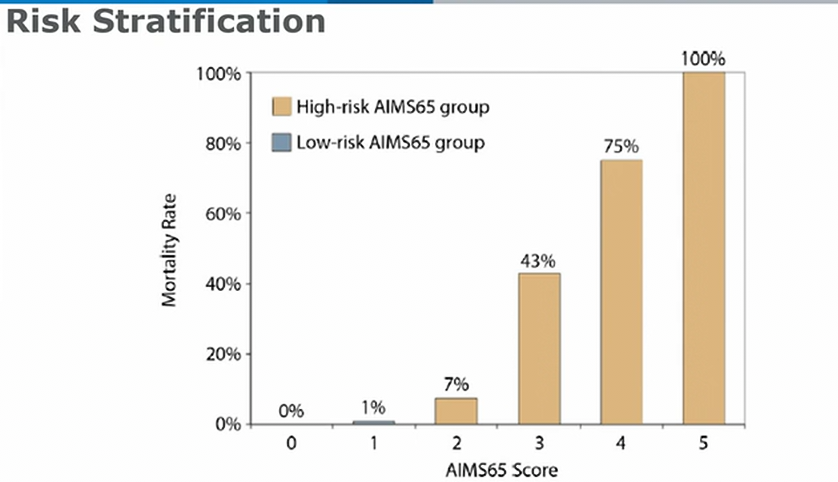
- AIM65 good for mortality prediction
UGIB
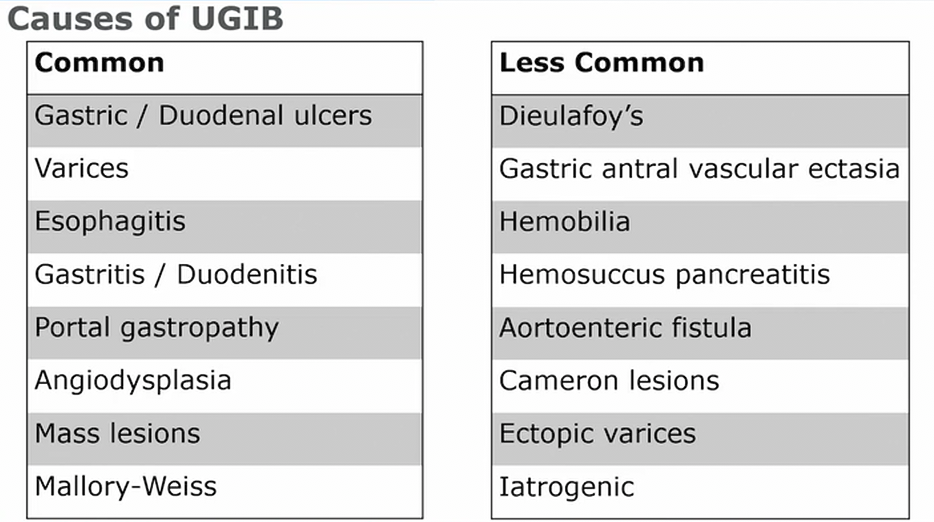
- 10-15% patients, lesion not found
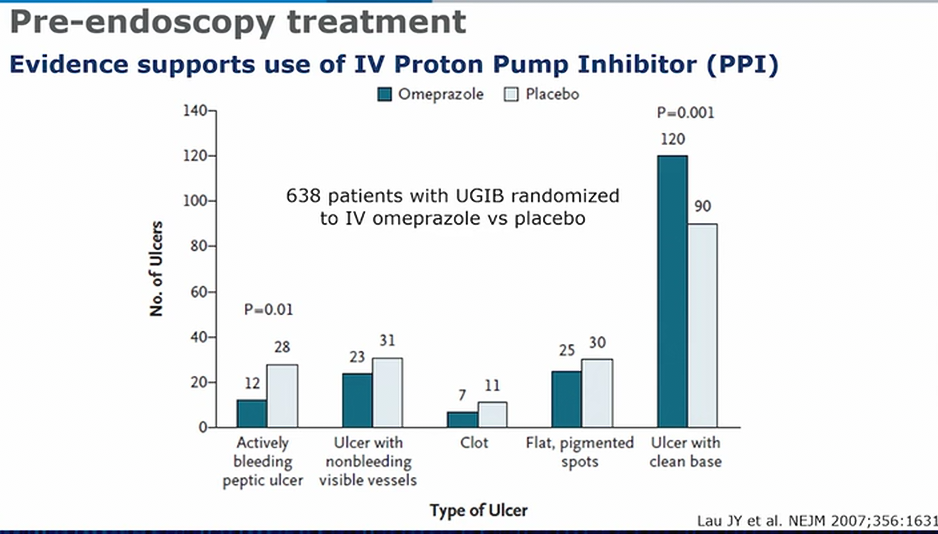
- omeprazole vs placebo. IV PPI very important
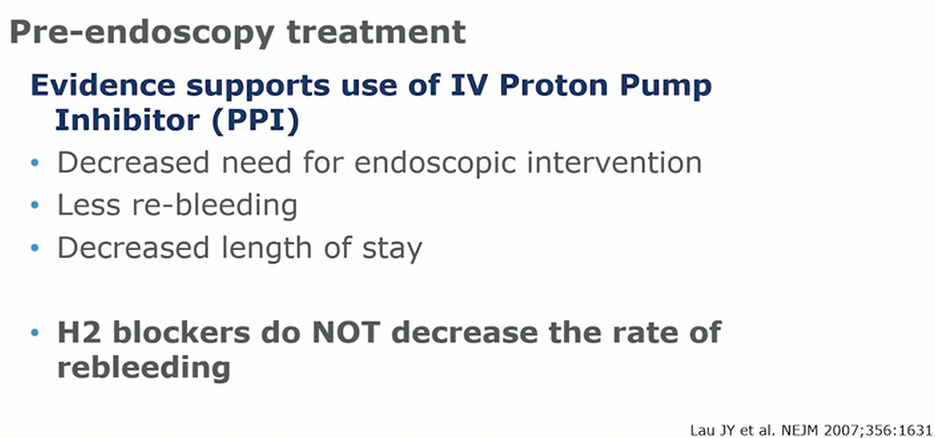
- neutral gastric pH is critical for stability of clot formation
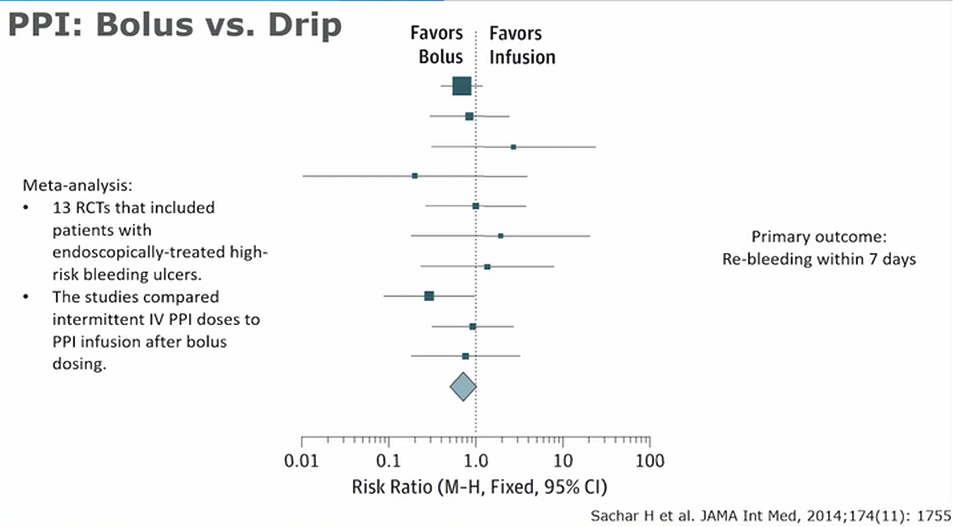
- intermittent PPI preferred over ggt
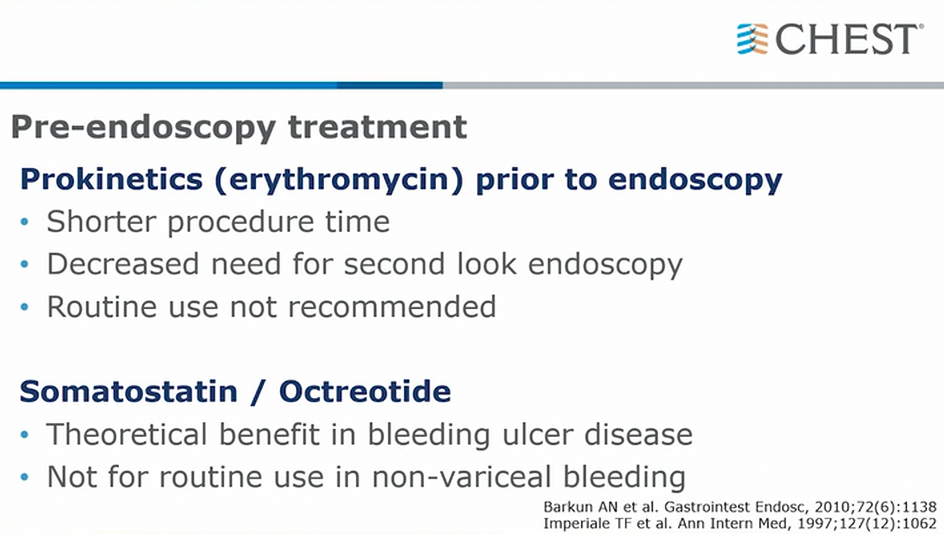
- erythromycin 30-90 min before procedure. Does not improve other outcomes
- octreotide: decrease gastric acid secretion and blood flow. Really only if EGD not available
- this is for non variceal bleeding
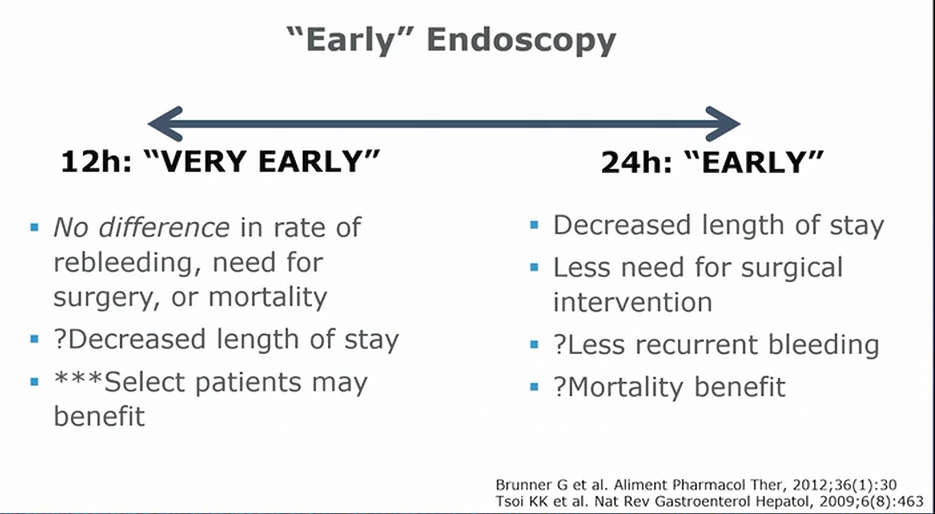
- very early not necessarily better than 24 hours
- unstable patients may benefit from very early intervention. However, first step is always stabilize and resus
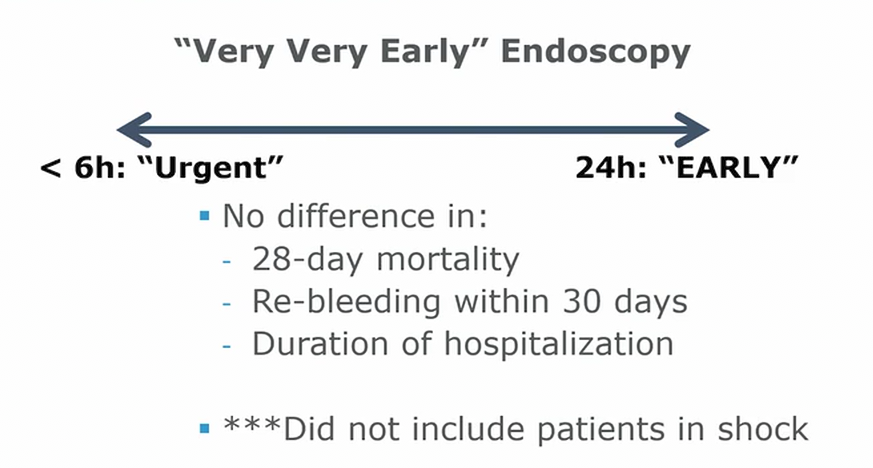
- if patient decompensating, scoping is next
- this is for stable patients
- this is for non variceal bleeding
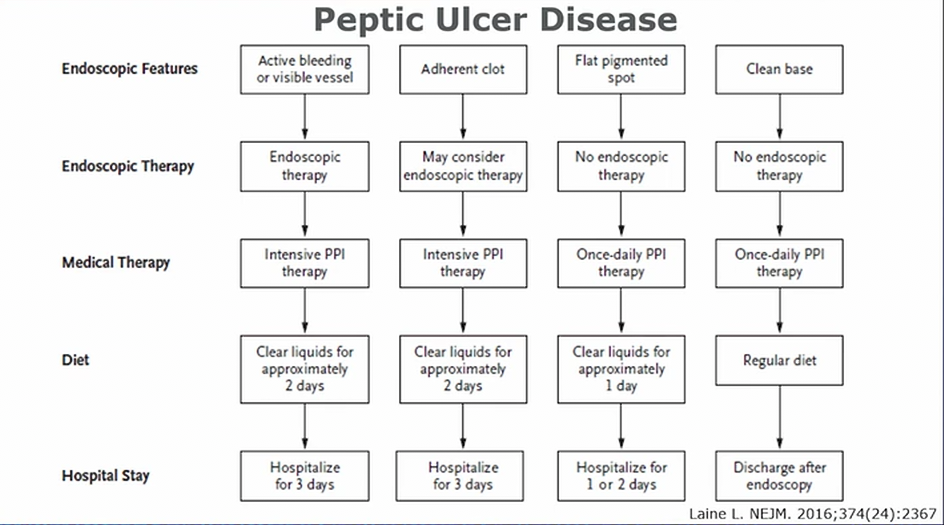
- adherent clot: 25-30% chance of rebleed
- visible vessel: 50% rebleed risk
- active bleed: 90% chance rebleed. Keep in ICU and monitor for extra day
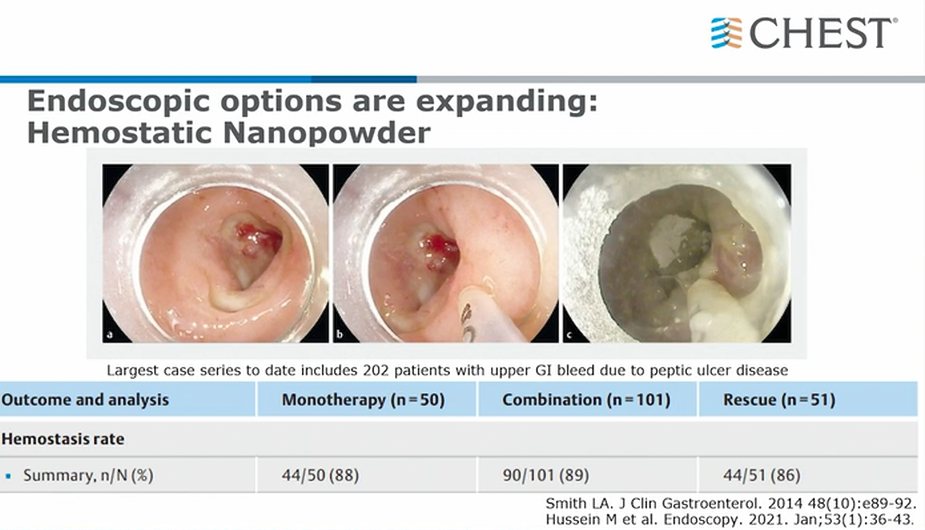
- new powder, sprayed on surface of bleed
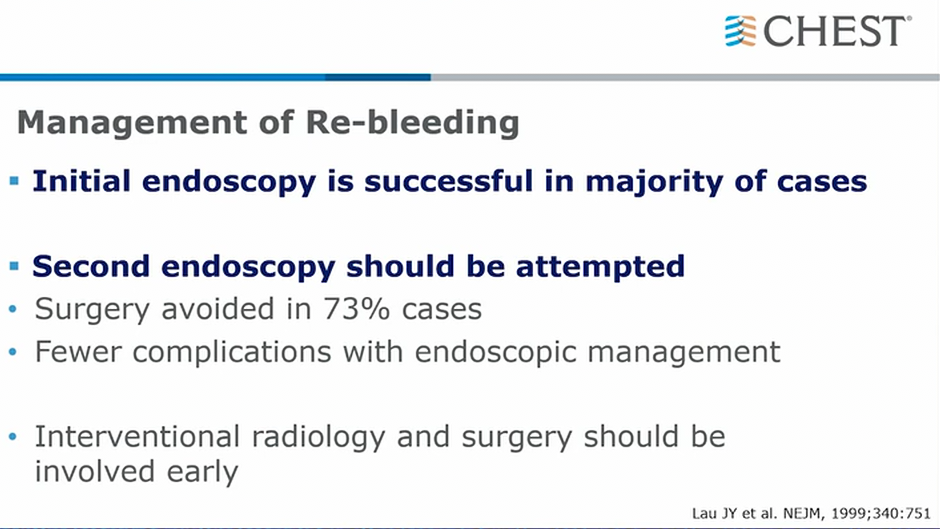
- 2nd endoscopy if rebleed
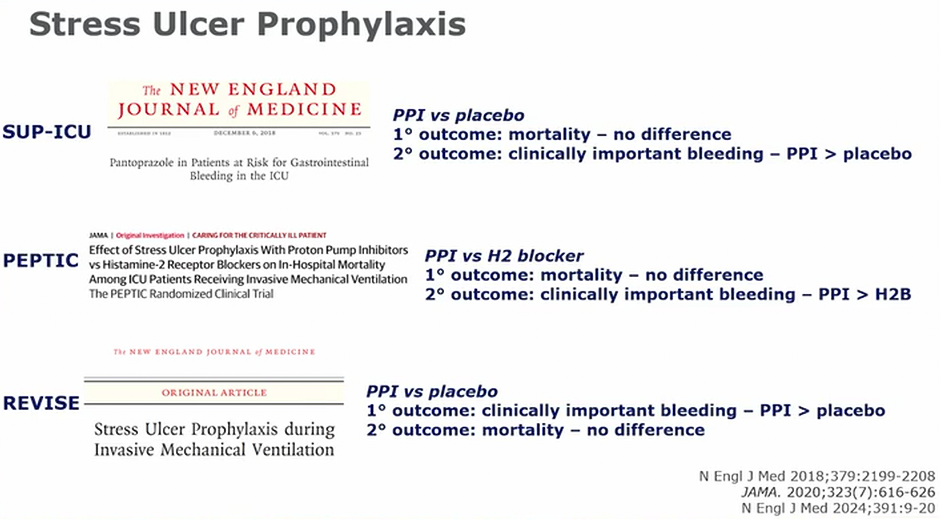
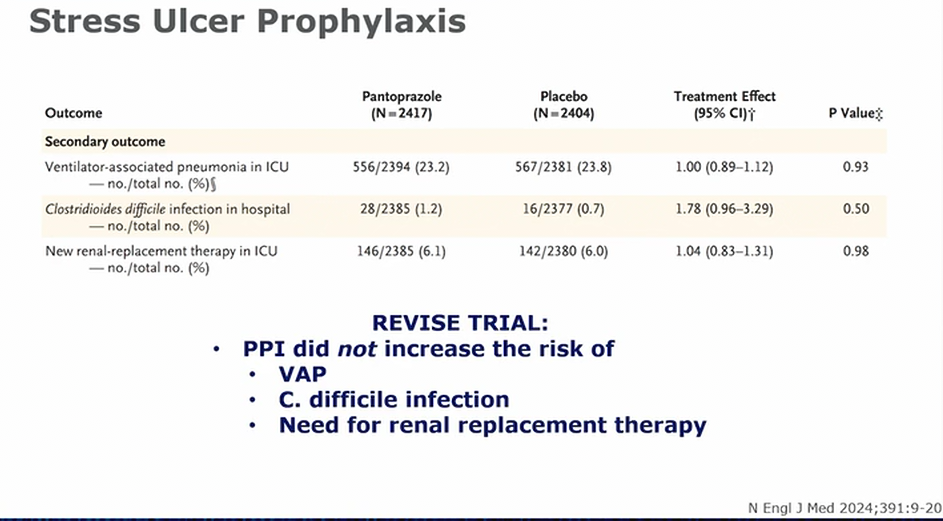
- PPI better than placebo and H2 in preventing clinically important bleeding (hemodynamic instability, EGD intervention needed)
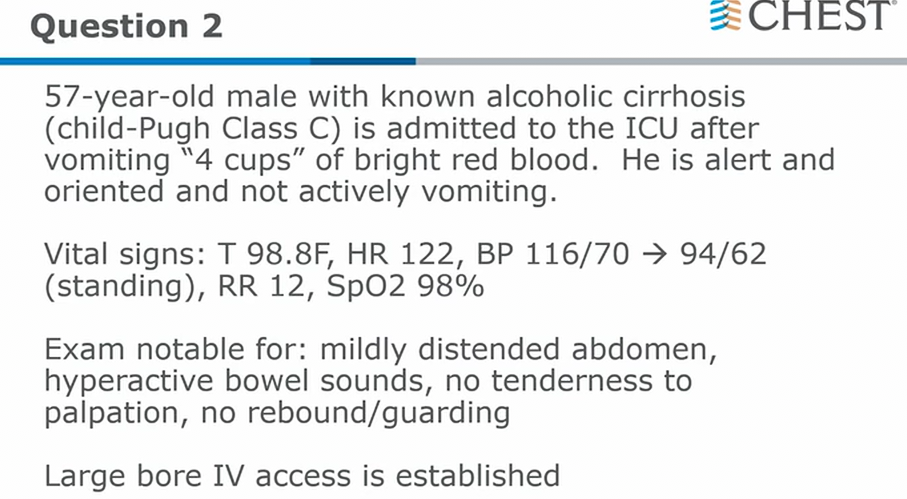
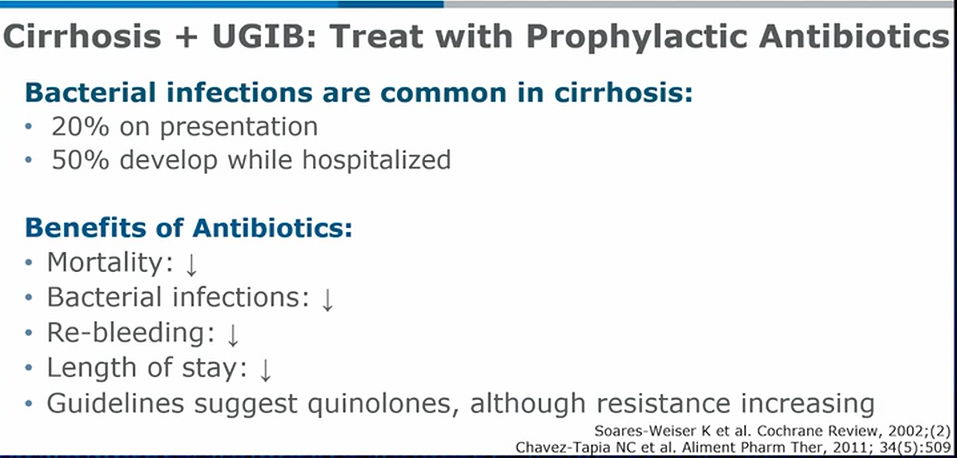
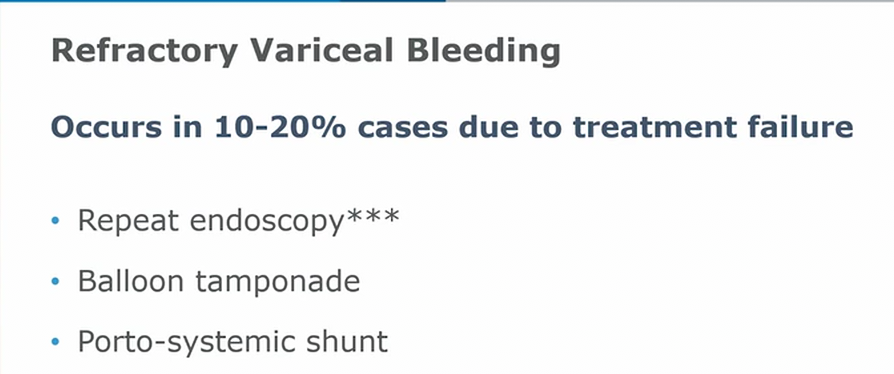
Variceal bleeding
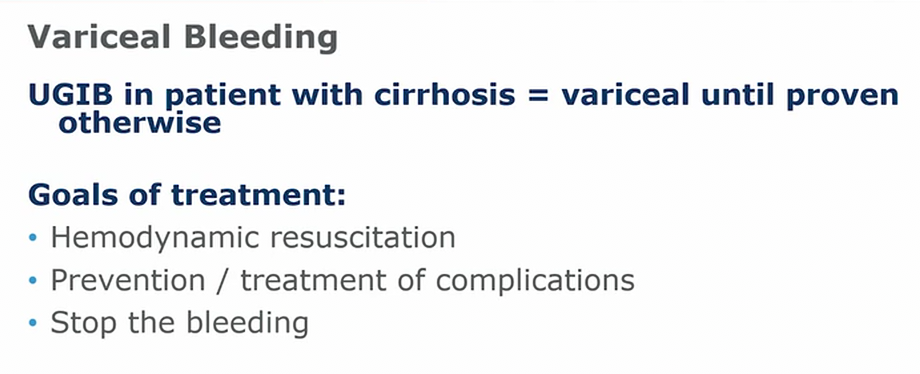
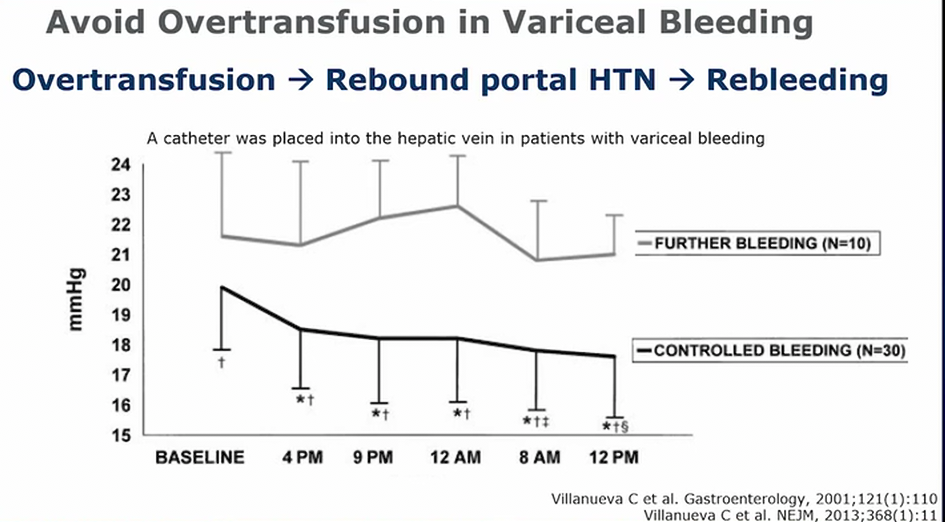
- don’t over transfuse
- people with continued bleeding are found to have higher pressure gradient, which can be from over transfusion
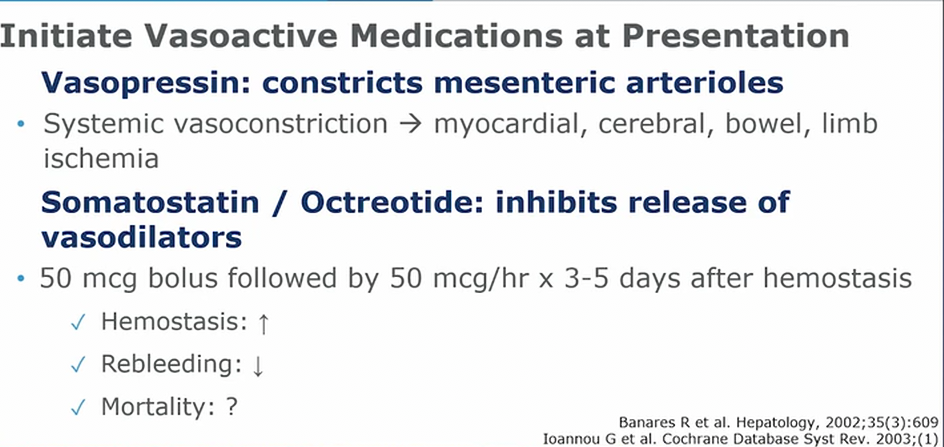
- vasopressin is helpful but at the dose required can cause systemic vasoconstriction and other side effects
- continue to use after hemostasis
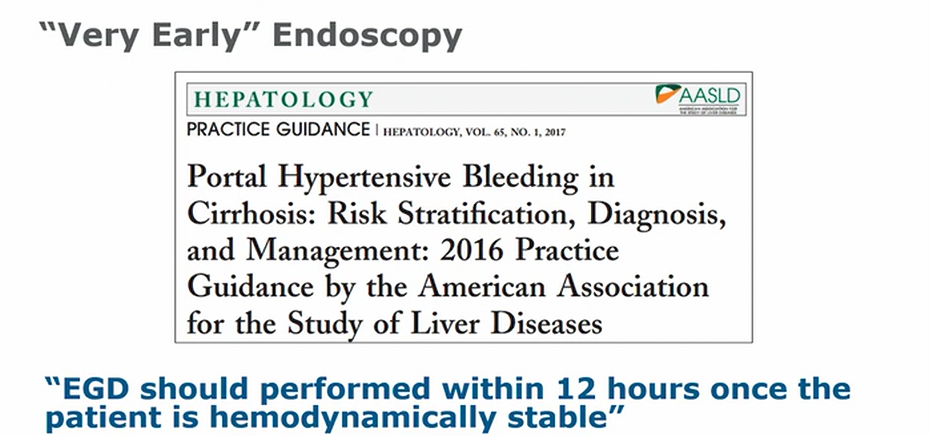
- variceal bleed, very early EGD

- banding is superior
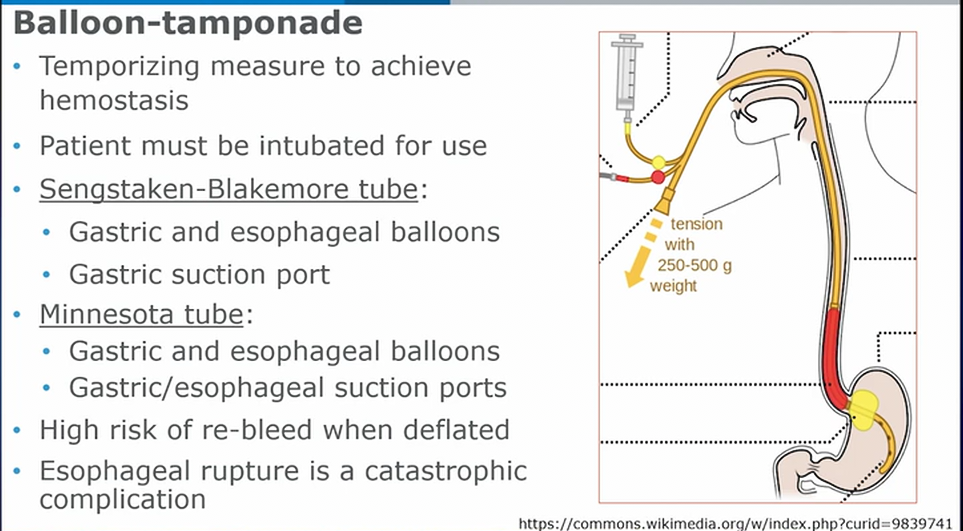
- patient needs to be intubated
- Minnesota tube has esophageal port could be better for proximal suctioning
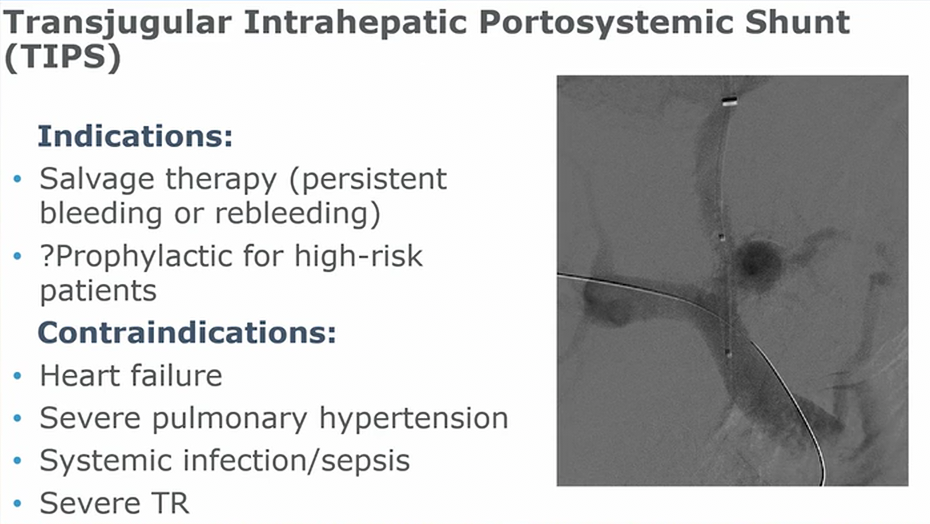
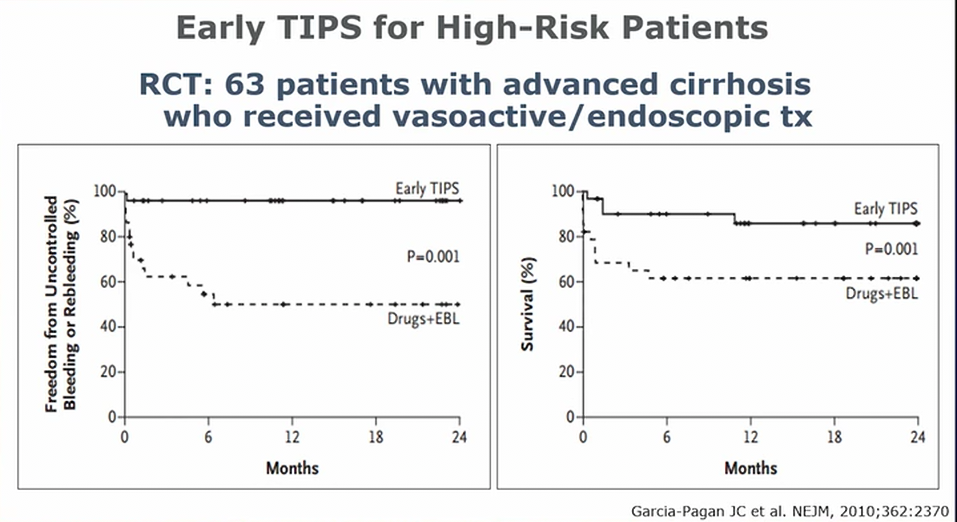
- salvage therapy
- great for very high pressure (> 20 mmHg)
- TIPS increases flow to right heart and can worsen other hemodynamics (TIPS can cause portopulmonary hypertension)
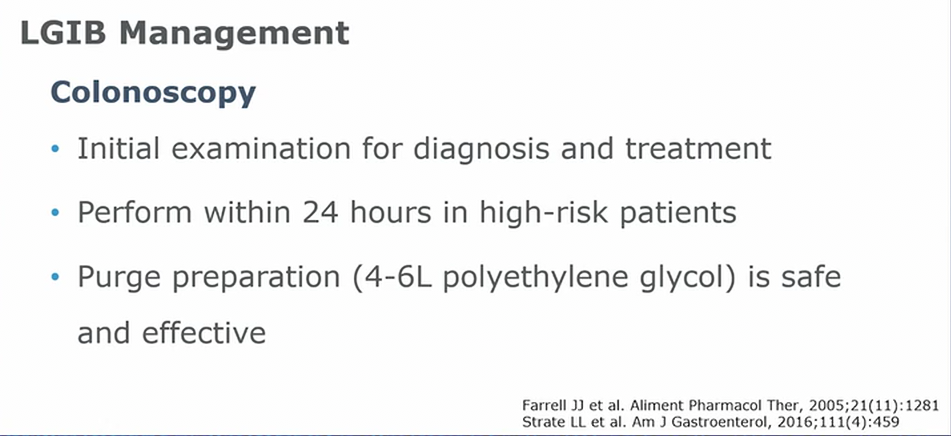
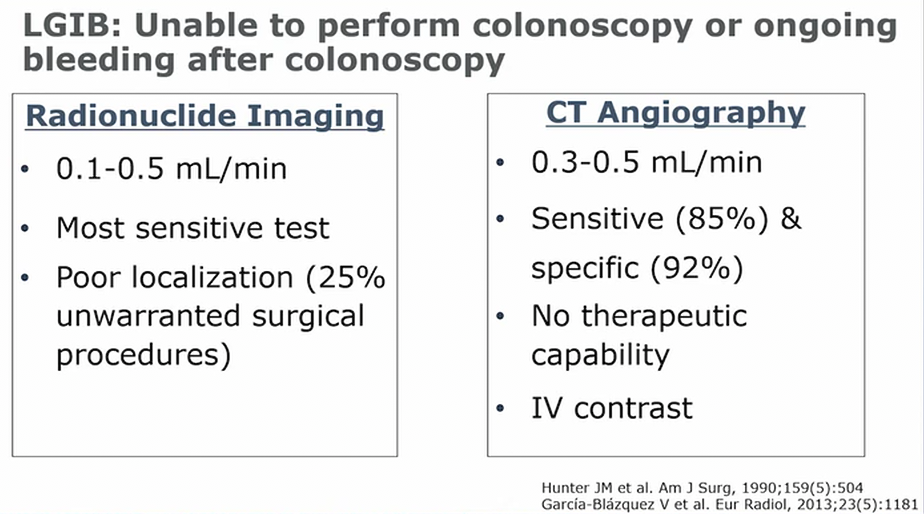
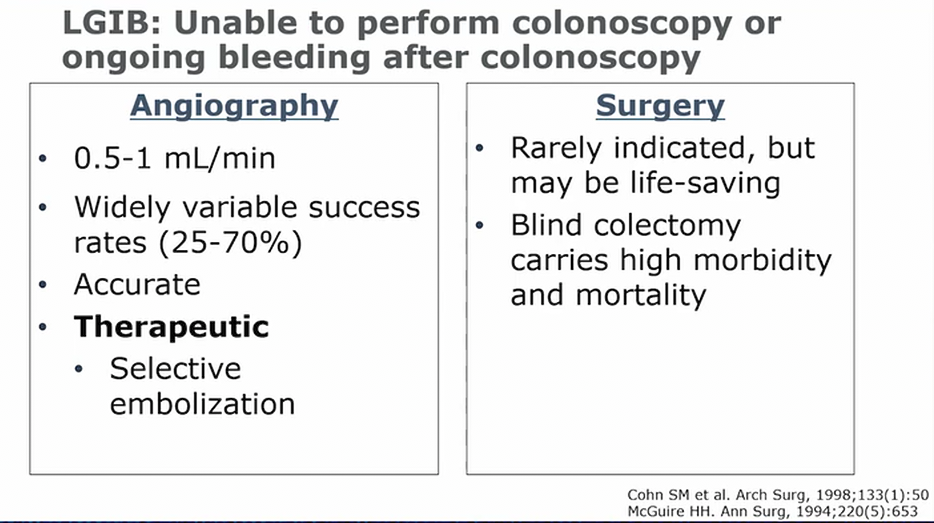
LGIB
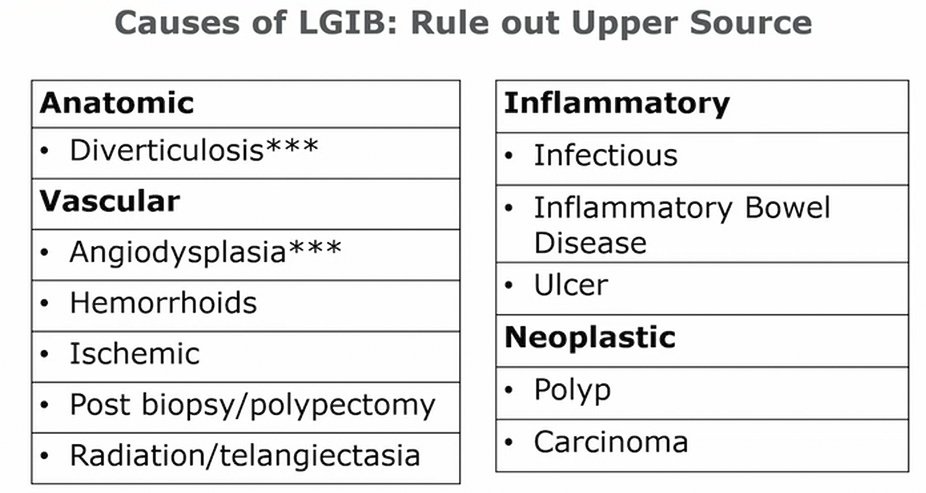
- first step is rule out UGIB
C Diff
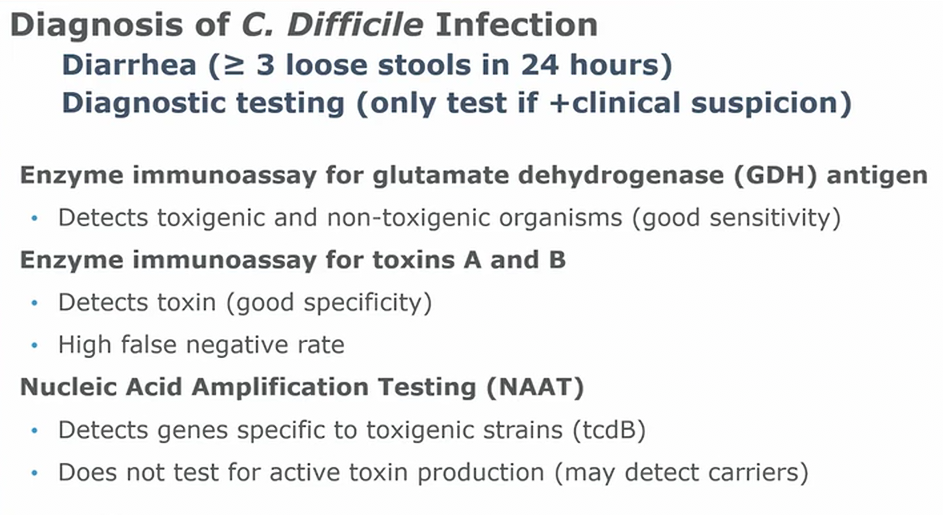
- must have diarrhea
- must have clinical suspicion
- screening + confirm test
- toxin B produces symptoms
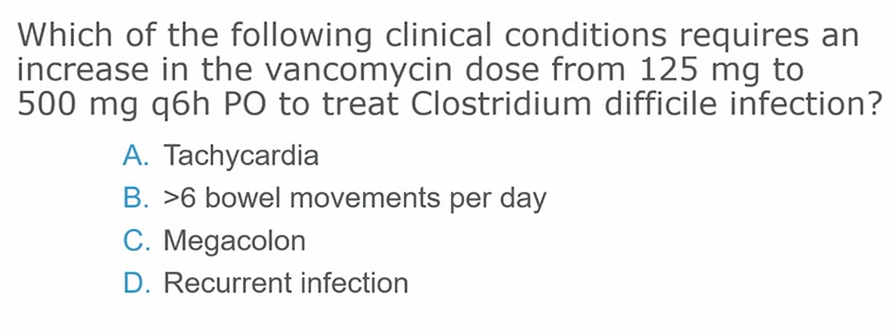
- megacolon
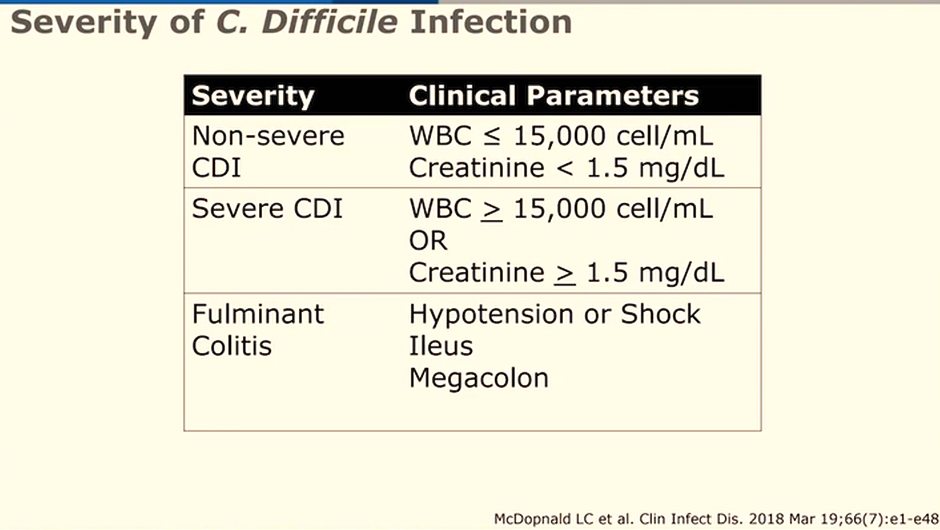
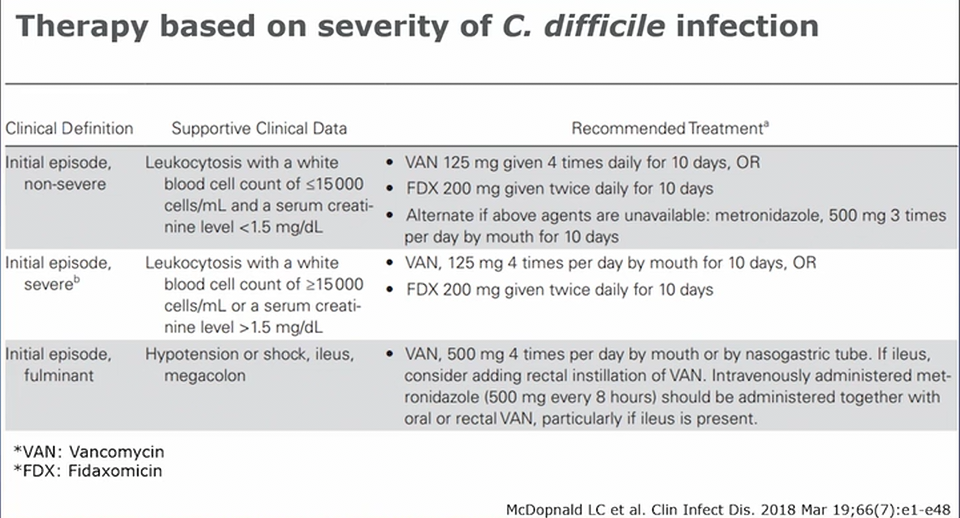
- fulminant
- increase vanc dosing
- consider adding rectal vanc if ileus
- IV flagyl
- do not give fidaxomicin
- get EGS on board for potential surgery
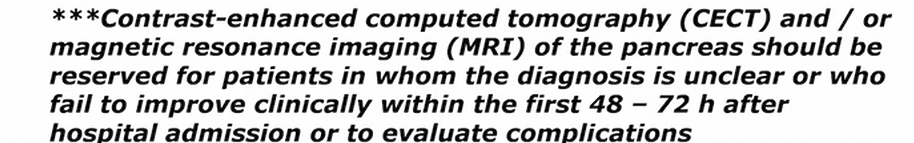
Pancreatitis
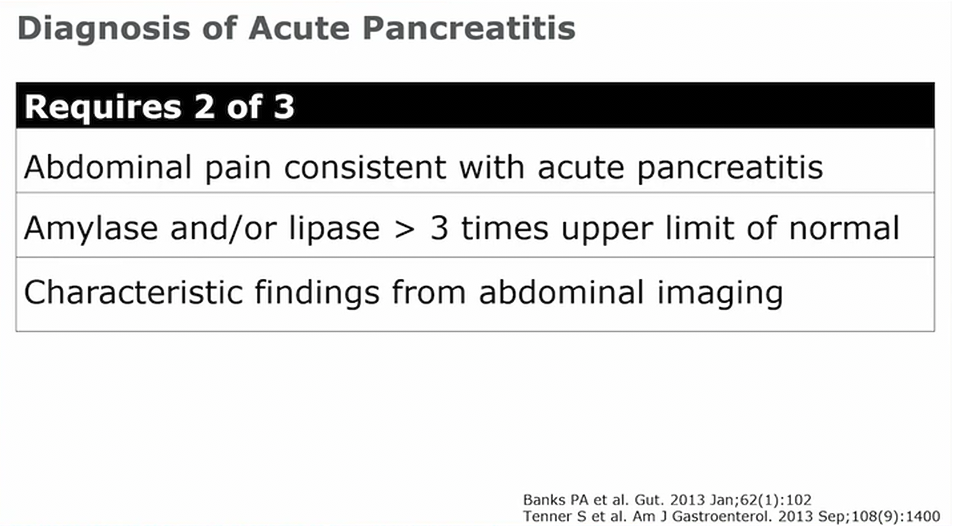
- amylase with short half life, stick around for 2-3 days. Lipase can stick around up to 2 weeks
- amylase: not elevated in 20% of cases. People with alcoholic pancreatitis might not have elevated amylase (just not able to make any) and also in 50% of hyper triglyceride pancreatitis (triglycerides interferes with amylase assay)
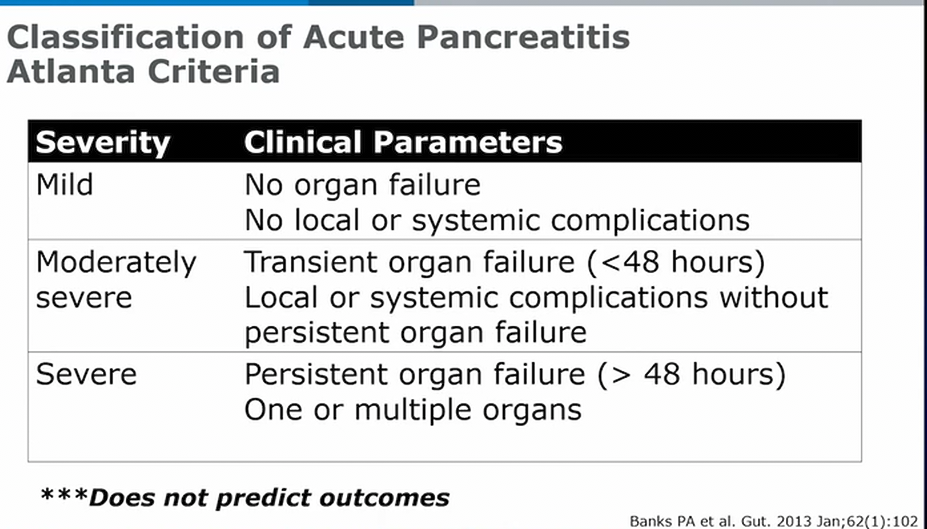
- moderately severe: peripancreatic fluid, necrosis, pseudocysts
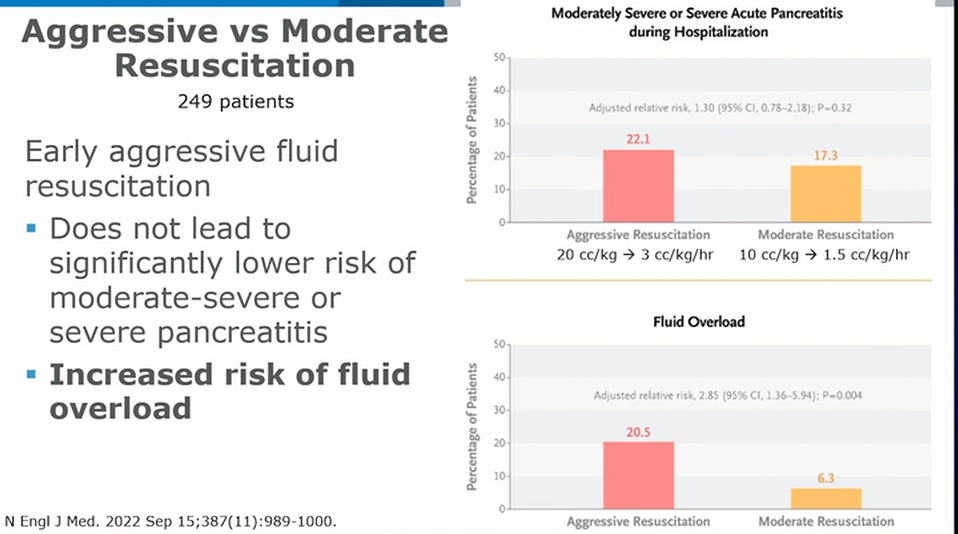
- 20cc/kg bolus + 3cc/kg/hr vs 10cc/kg bolus + 1.5 cc/kg/hr
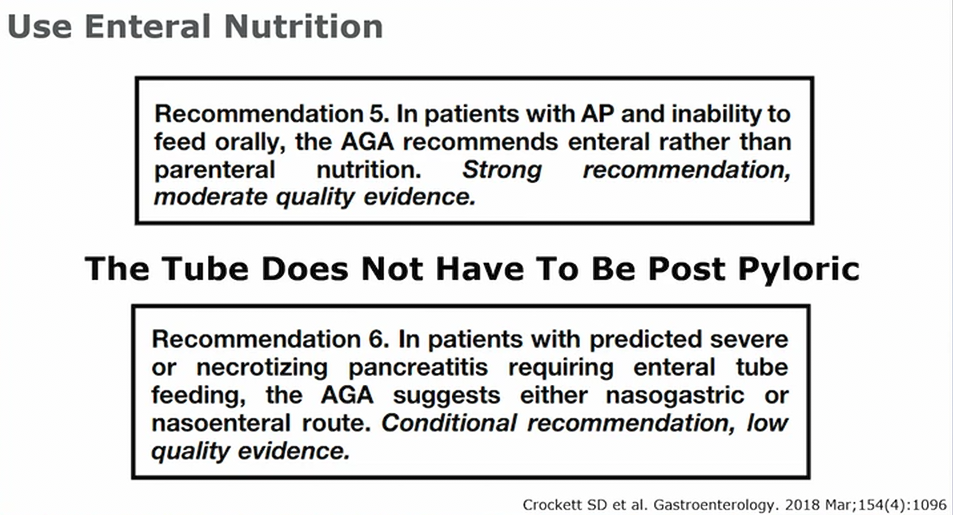
- tube does not need to be post pyloric
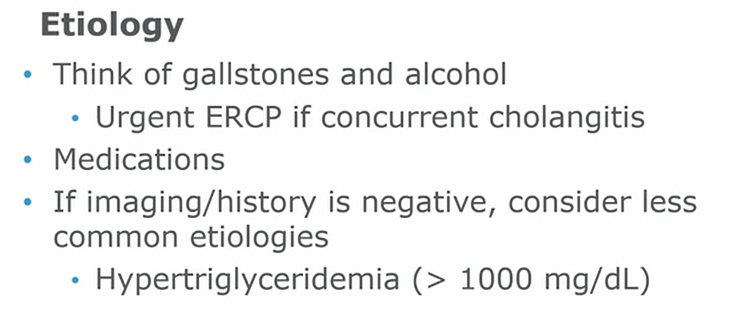
- TG with lactic acidosis, hypocalcemia: consider plasmapheresis
- treat with insulin gtt until TG < 500