hypogonadotrophic hypogonadism
- related: Endocrinology
- tags: #endocrine
In Diabetes
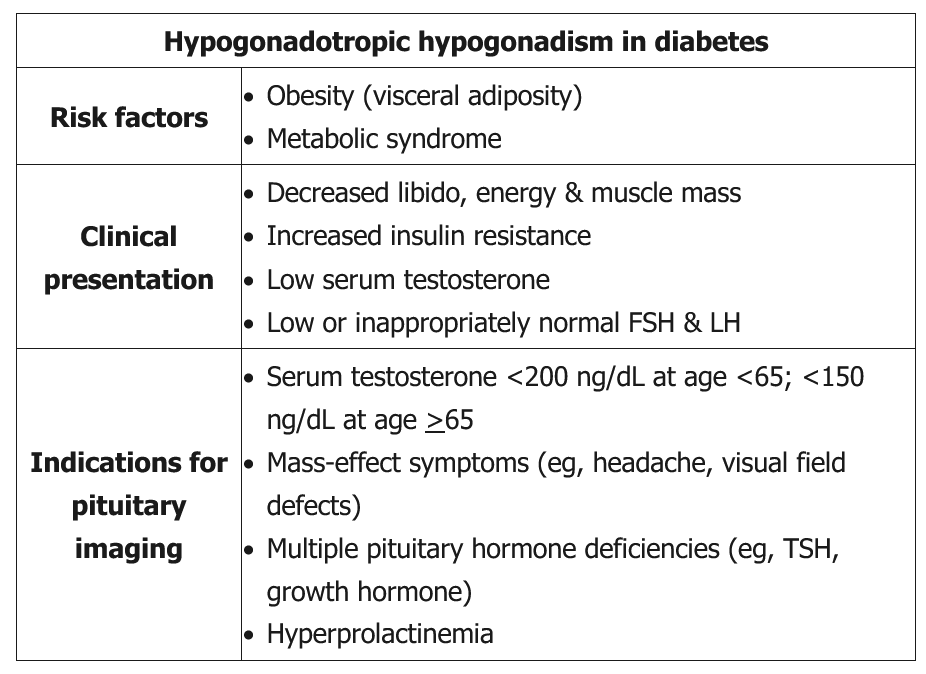
This patient has hypogonadal symptoms with a low serum testosterone level and low/inappropriately normal FSH and LH levels. This is consistent with hypogonadotropic (central) hypogonadism. Hypogonadism is common in men with type 2 diabetes, especially those age >65 or with concurrent obesity. For this reason, some experts have recommended regular screening with serum testosterone in patients with diabetes.
Older (ie, age >65) obese men with type 2 diabetes typically have low-normal to mildly low serum testosterone levels (200-300 ng/dL) due to decreased gonadotropin release from the anterior pituitary (likely obesity mediated), as well as physiologic changes in testosterone metabolism (eg, decreased sex hormone-binding globulin). These patients do not need pituitary imaging. However, younger men with more pronounced declines in serum testosterone (as in this patient) and/or abnormalities in additional pituitary hormones (eg, central hypothyroidism) are more likely to have sellar masses or other structural disruptions of the hypothalamic-pituitary axis (eg, infiltrative disease). These patients should have pituitary imaging, preferably with MRI.
Links to this note
- Reproductive Disorders
- Secondary hypogonadism reflects a hypothalamic (GnRH) and/or pituitary (LH/FSH) deficiency. There are rare congenital causes, such as Kallmann syndrome, which are associated with anosmia. Common causes of acquired hypogonadotrophic hypogonadism are hyperprolactinemia, medications, critical illness, untreated sleep disorders, obesity, liver and kidney disease, alcoholism, marijuana use, and disordered eating. Tumors, trauma, thalassemias, and infiltrative diseases that cause disruption of gonadotropin production (such as sarcoidosis and hemochromatosis) are uncommon causes.