hypoparathyroidism
- Keywords: Step 3, Medicine, Endocrinology, Parathyroid
Hypoparathyroidism
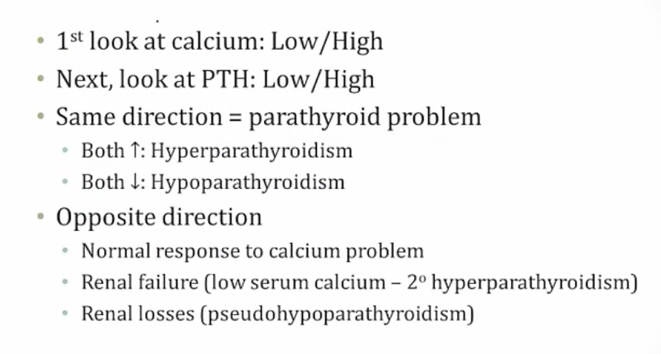
- primary: low PTH, surgery, radiation, autoimmune, congenital (Digeorge, APS-1)
- pseudohypoparathyroidism: abnormal sensor to PTH in kidney and bone
- lab looks like secondary hyperparathyroidism
- high PTH, low Ca, high phos
- Albright’s Hereditary Osteodystrophy: pseudohypoparathyroidism
- mental retardation, short stature, round faces, short 4th/5th metacarpals
A 10-year-old boy is brought to the emergency department following an episode of generalized tonic-clonic seizure. Intravenous benzodiazepine was administered, terminating the patient’s seizure. He has had no trauma, fever, headache, vomiting, or cough. For the last 2-3 months, the patient has had muscle pain and cramping that is exacerbated by exercise and relieved after a short rest. His mother states that for the past year his school performance has been deteriorating. Physical examination shows a sedated child who is arousable to painful stimuli. There are no dysmorphic features. Eye examination reveals pupils that are 3 mm in diameter and briskly reactive to light; bilateral cataracts are seen. The heart, lungs, and abdomen are normal. The patient moves all extremities on painful stimulation. Deep tendon reflexes are 3+ throughout. Serum calcium is 6 mg/dL, serum albumin is 3.8 g/dL, serum phosphorus is 8.2 mg/dL, and parathyroid hormone level is 150 pg/mL (normal: 10-65). A non-contrast CT scan of the head reveals calcification of the basal ganglia. Which of the following is the most likely cause of this patient’s hypocalcemia?