lithium toxicity
- related: toxicology and toxic ingestions
- tags: #literature #pharm #icu
Lithium is a mood stabilizer that has been used in the United States to treat mania and bipolar disorder since the 1970s. Because of the narrow therapeutic window, there are more than 6,000 cases of lithium toxicity reported to Poison Control annually, and most patients prescribed lithium will experience an episode of toxicity during their course of treatment.
Symptoms of severe lithium toxicity include seizures, coma, stupor, hemodynamic collapse or shock, rigidity or hypertonicity, or life-threatening arrhythmias. Management of lithium toxicity is centered on supportive care and removal of lithium either through IV fluids to restore or maintain intravascular volume and increase renal excretion or removal with hemodialysis.
The patient in this question has severe lithium toxicity, with levels greater than 5 mEq/L (5 mmol/L) associated with altered mental status, difficulty walking, severe bradycardia, and acute renal insufficiency. This patient is at high risk for a poor neurologic outcome because of high lithium levels and impaired renal function, which impede her ability to eliminate lithium. At this time, emergency hemodialysis should be pursued (choice A is correct). Other supportive measures should include admission to the ICU and IV fluid hydration, with as-needed therapy with benzodiazepines for seizures, atropine and/or dopamine for bradycardia, and consideration of temporary transvenous pacer placement.
Although gastrointestinal decontamination is recommended for some cases of lithium toxicity, its effects are limited to patients who are awake and without symptoms who present early (within 4 h of ingestion). The patient in this scenario is critically ill, receiving ventilation, has been receiving chronic lithium therapy, and reports progressive symptoms consistent with lithium toxicity that has developed over a period of days (choice C is incorrect).
There are case reports of the use of IV lipid emulsion therapy to treat overdoses with lipophilic medications such as local anesthetics and β-blockers with some degree of success, but there is no evidence about the use of this therapy in lithium toxicity (choice D is incorrect).
Digoxin-specific antibody is used to treat digitalis (cardiac glycoside) toxicity, but this patient has no known history of exposure to this medication. In addition, classic features of digitalis poisoning are absent in this case, including hyperkalemia and the “digitalis effect” on ECG: T-wave changes, shortened QT interval, plus scooped ST segments and depression (choice B is incorrect).123
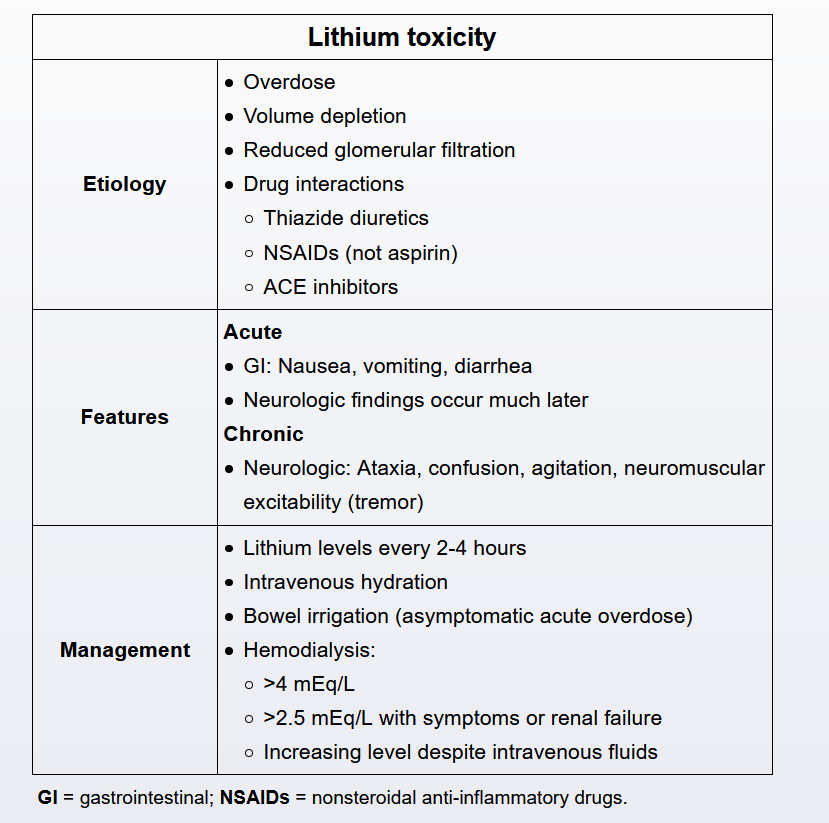
Initial management includes evaluating and stabilizing the airway and circulation. Saline infusion is the first-line therapy to ensure significant lithium clearance. Hemodialysis is indicated for serum lithium levels > 4 mEq/L (4 mmol/L) OR levels > 2.5 mEq/L PLUS either signs of significant lithium toxicity (eg, seizures, depressed mental status) or inability to excrete lithium (eg, renal disease, decompensated heart failure).
A 45-year-old woman with a history of bipolar disorder, posttraumatic stress disorder, asthma, and nicotine dependence presented to the emergency department with altered mental status, expressive aphasia, and bradycardia. History is obtained from the patient’s husband who states that she has had difficulty sleeping, fatigue, and difficulty expressing herself for the past couple of days. The patient’s home medications include ibuprofen as needed, extended-release lithium, lamotrigine, venlafaxine, and zolpidem.
Her vital signs in the emergency department are a heart rate of 25/min, BP of 95/45 mm Hg, respiratory rate of 8/min, and SpO2 of 94% with 4 L via nasal cannula. On examination, the patient has a Glasgow Coma Scale score of 6 with minimal gag reflex. The ECG is shown in Figure 1, and laboratory test results are shown in Figure 2. The patient undergoes intubation and mechanical ventilation and is receiving IV crystalloid fluids.
What is the most appropriate next step in management?
Links to this note
Footnotes
-
Decker BS, Goldfarb DS, Dargan PI, et al; EXTRIP Workgroup. Extracorporeal treatment for lithium poisoning: systematic review and recommendations from the EXTRIP Workgroup. Clin J Am Soc Nephrol. 2015;10(5):875-887. PubMed ↩
-
Jovic-Stosic J, Gligic B, Putic V, et al. Severe propranolol and ethanol overdose with wide complex tachycardia treated with intravenous lipid emulsion: a case report. Clin Toxicol (Phila). 2011;49(5):426-430. PubMed ↩