long QT
- related: cardiac arrythmia
- tags: #literature #cardiology
Long QT syndrome is among the most common inherited arrhythmias, affecting between 1 in 1000 and 1 in 5000 persons. Prolongation of the QTc interval has many causes, most of which are acquired, such as medication use, structural heart disease, and electrolyte abnormalities. Drugs that have been implicated in QT prolongation include antiarrhythmic agents, antibiotics (including some macrolides and fluoroquinolones), antipsychotic drugs, and antidepressants. A list of drugs categorized by their potential to cause QT prolongation is available at https://crediblemeds.org. The presence of a prolonged QTc interval (>440 ms in men and >460 ms in women) alone is insufficient to diagnose long QT syndrome. Diagnosis requires the presence of a QTc interval greater than 500 ms on repeated 12-lead ECGs accompanied by unexplained syncope or ventricular arrhythmia. Patients with a QTc interval greater than 500 ms are at greatest risk for SCD. β-Blockers are first-line therapy; however, patients with cardiac arrest or those who have recurrent events (syncope or VT) refractory to β-blocker therapy are candidates for ICD placement. These patients should not participate in competitive athletics.
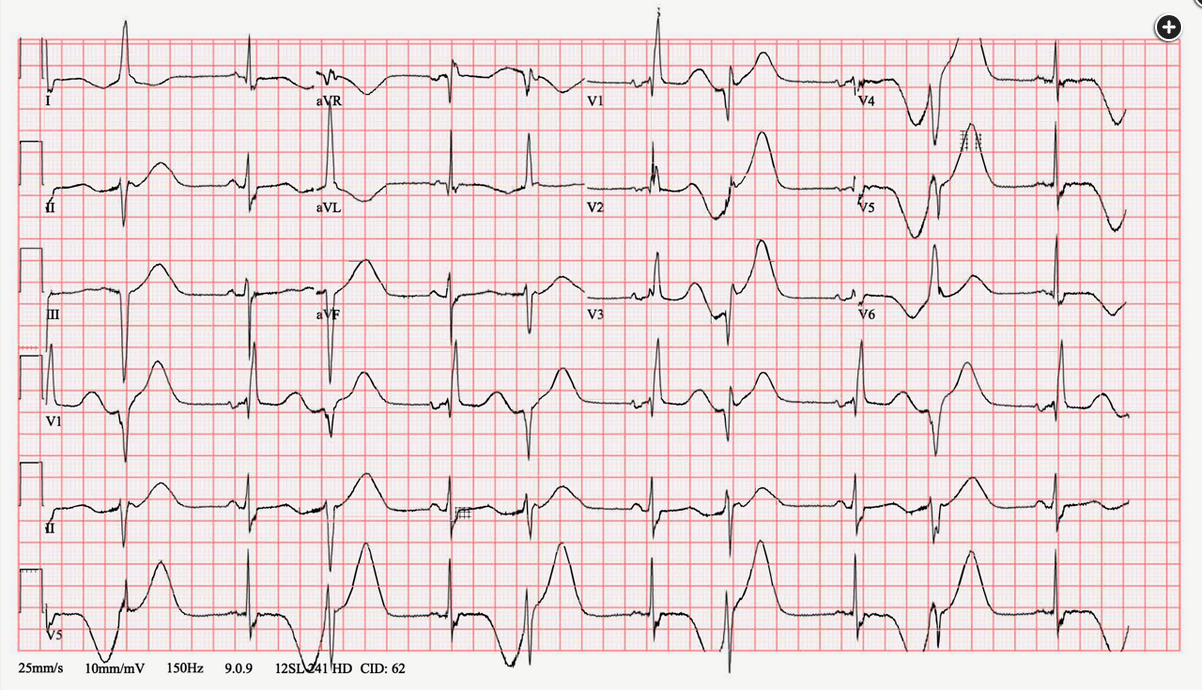
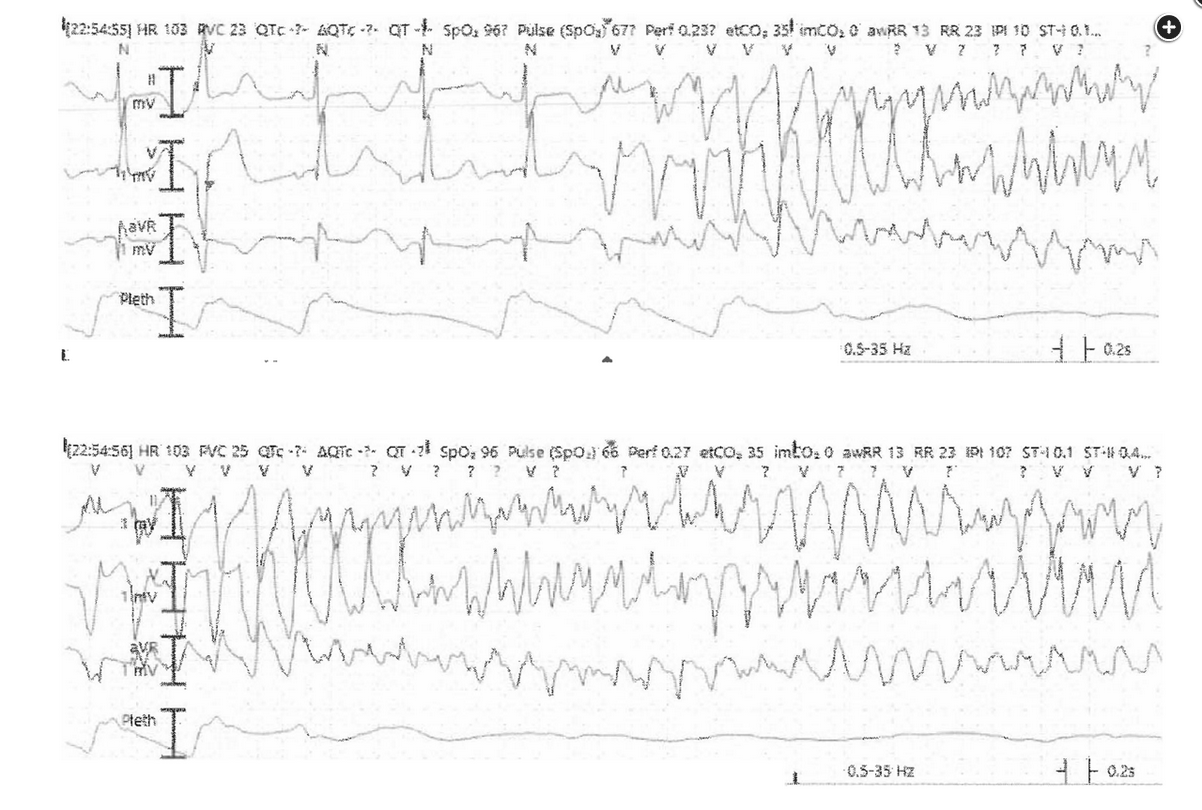
Figure 2 demonstrates a wide complex tachycardia with morphologically distinctive “twisting of the points” characteristic of torsades de pointes (TdP). The primary risk factor for this arrhythmia is marked QT interval prolongation on admission ECG in a patient with underlying structural heart disease and severe hypokalemia. In addition to addressing reversible risk factors for recurrent arrhythmia (ie, correcting potassium in this patient), treatment with IV magnesium is most appropriate at this time.
A prolonged QT interval (corrected QT [QTc] >480 and >470 ms in women and men, respectively) can be due to either genetic or acquired causes. Acquired long QT syndrome is most commonly associated with drugs—also referred to as drug-induced long QT syndrome—which in combination with other risk factors can lead to life-threatening arrhythmias, including TdP. Other risk factors include advanced age, baseline conduction abnormalities, advanced structural heart disease, inadequate dose adjustment in the presence of liver or kidney disease, electrolyte derangements (hypokalemia, hypomagnesemia, or hypocalcemia), and bradycardic rhythms.
Figure 3 provides a summary of common drugs associated with symptomatic TdP. Patients receiving multiple antiarrhythmic or psychiatric medications appear to be at greatest risk, in addition to patients who are hospitalized and critically ill receiving multiple other agents that cause QT prolongation. Of note, targeted cancer therapy of hematologic and solid tumors (renal cell carcinoma, gastrointestinal tumors) with small-molecule tyrosine kinase inhibitors has become quite common, and this class of chemotherapy agents appears to carry the highest risk of QT prolongation and arrhythmia. The now-disproven use of combination therapy with hydroxychloroquine and azithromycin is thought to be a major contributing factor to arrhythmias seen in patients with SARS-CoV-2 infection.
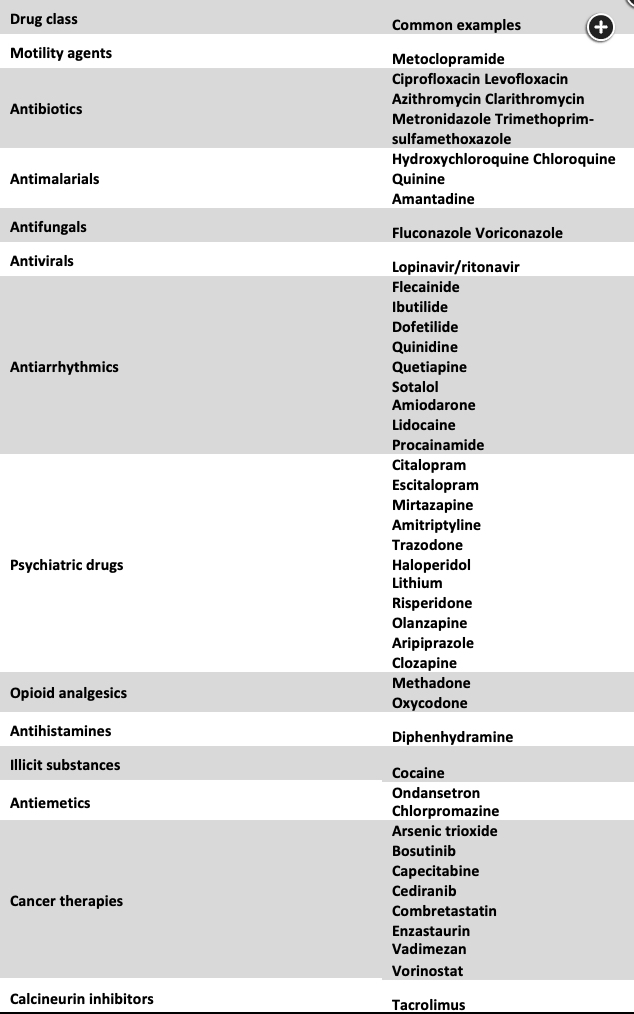
Common drug categories and examples associated with QT interval prolongation. Flecainide and methadone had the highest associated risk of life-threatening arrhythmias in one retrospective review of cases reported to a regional poison control center.
The primary mechanism leading to TdP is early depolarization (ie, a premature ventricular complex) during prolonged ventricular repolarization (ie, a long QTc interval, as in Figure 2). While the risk of malignant arrhythmia in the setting of prolonged QT interval is difficult to predict, QTc >500 ms or drug-induced increase of >30 to 60 ms should prompt concern. Magnesium inhibits cardiac myocyte calcium influx, suppressing automaticity and reducing early and late after-depolarizations. While prospective randomized clinical trials have failed to demonstrate that magnesium increases the rate of return of spontaneous circulation or survival after preor in-hospital cardiac arrest due to refractory ventricular fibrillation, guidelines continue to recommend its use in the setting of medication-induced TdP or marked electrolyte derangements. Aggressive correction of electrolytes and hypoxemia, discontinuation of offending agents, and pharmacologic or transvenous pacing to increase the heart rate should also be considered.
Sotalol is a class III antiarrhythmic drug that may prolong the QT interval and further slow the heart rate, increasing the risk of TdP development. Insulin and glucose can be given to patients with ECG changes and arrhythmia due to hyperkalemia, but this is not the cause of this patient’s change in rhythm. While older observational studies suggested that IV calcium administration may enhance ventricular contractility and improve hemodynamics, there remains no direct evidence that calcium supplementation improves outcomes in patients who are critically ill, and it may be harmful in patients with sepsis and cardiac arrest without hyperkalemia.12345678
Links to this note
Footnotes
-
Al-Khatib SM, Stevenson WG, Ackerman MJ, et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2018;72(14):e91-e220. PubMed ↩
-
Arunachalam K, Lakshmanan S, Maan A, Kumar N, Dominic P. Impact of drug induced long QT syndrome: a systematic review. J Clin Med Res. 2018;10(5):384-390. PubMed ↩
-
Malaty M, Kayes T, Amarasekera AT, et al. Incidence and treatment of arrhythmias secondary to coronavirus infection in humans: a systematic review. Eur J Clin Invest. 2021;51(2):e13428. PubMed ↩
-
Melchers M, van Zanten ARH. Management of hypocalcaemia in the critically ill. Curr Opin Crit Care. 2023;29(4):330-338. PubMed ↩
-
Porta-Sánchez A, Gilbert C, Spears D, et al. Incidence, diagnosis, and management of QT prolongation induced by cancer therapies: a systematic review. J Am Heart Assoc. 2017;6(12):e007724. PubMed ↩
-
Ryan K, Benz P, Zosel A, Farkas A, Theobald J. QTc prolongation in poison center exposures to CredibleMeds list of substances with “known risk of torsades de pointes.” Cardiovasc Toxicol. 2022;22(9):866-877. PubMed ↩
-
Thomas SH, Behr ER. Pharmacological treatment of acquired QT prolongation and torsades de pointes. Br J Clin Pharmacol. 2016;81(3):420-427. PubMed ↩