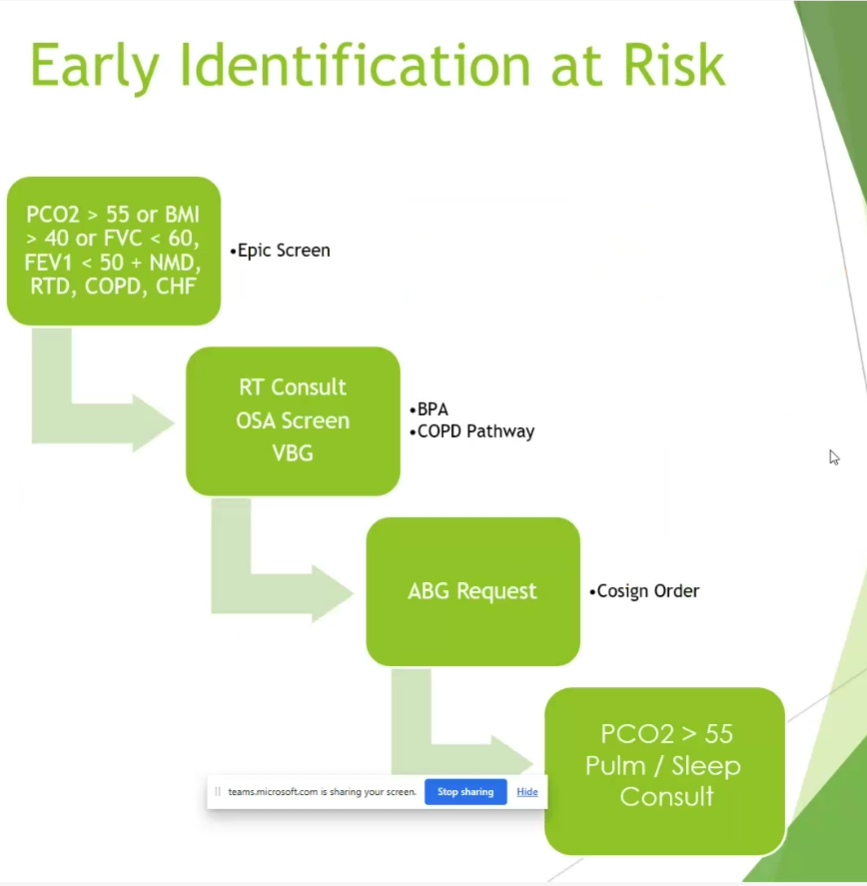
Namen hypoventilation syndrome 2025
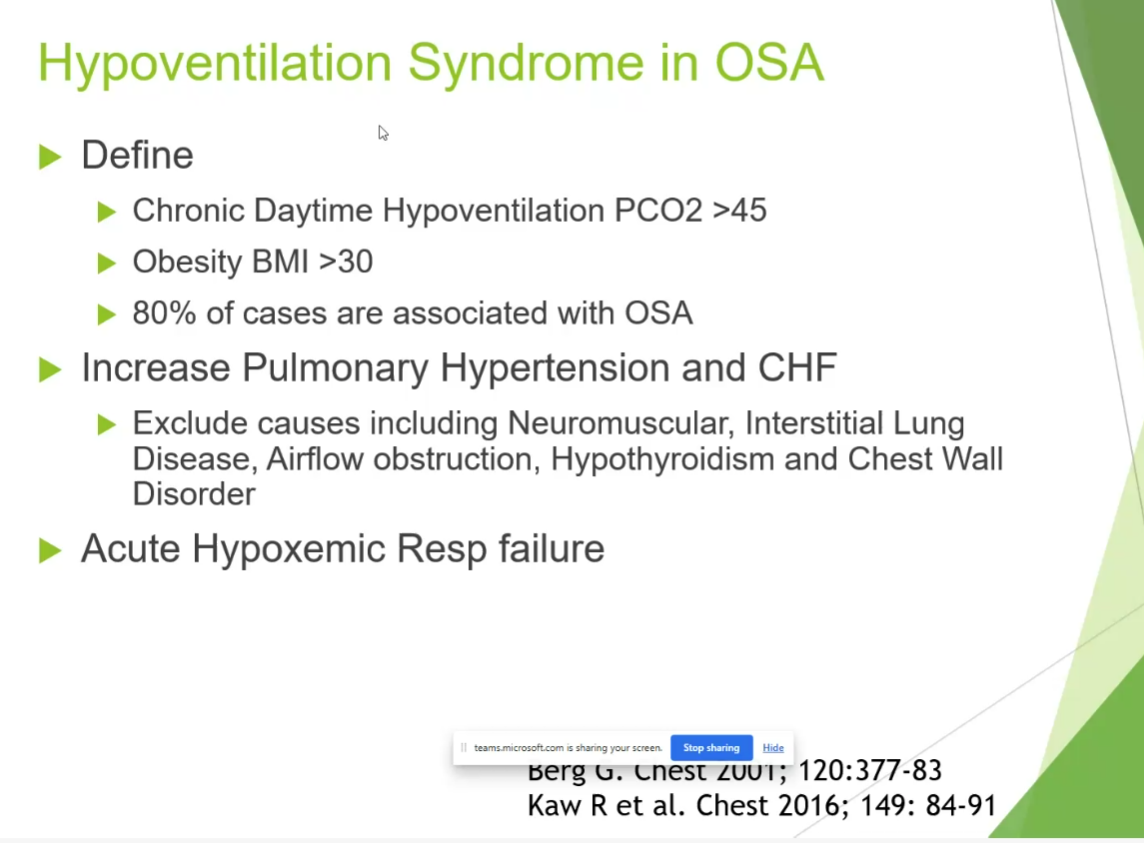
Conditions and Challenges
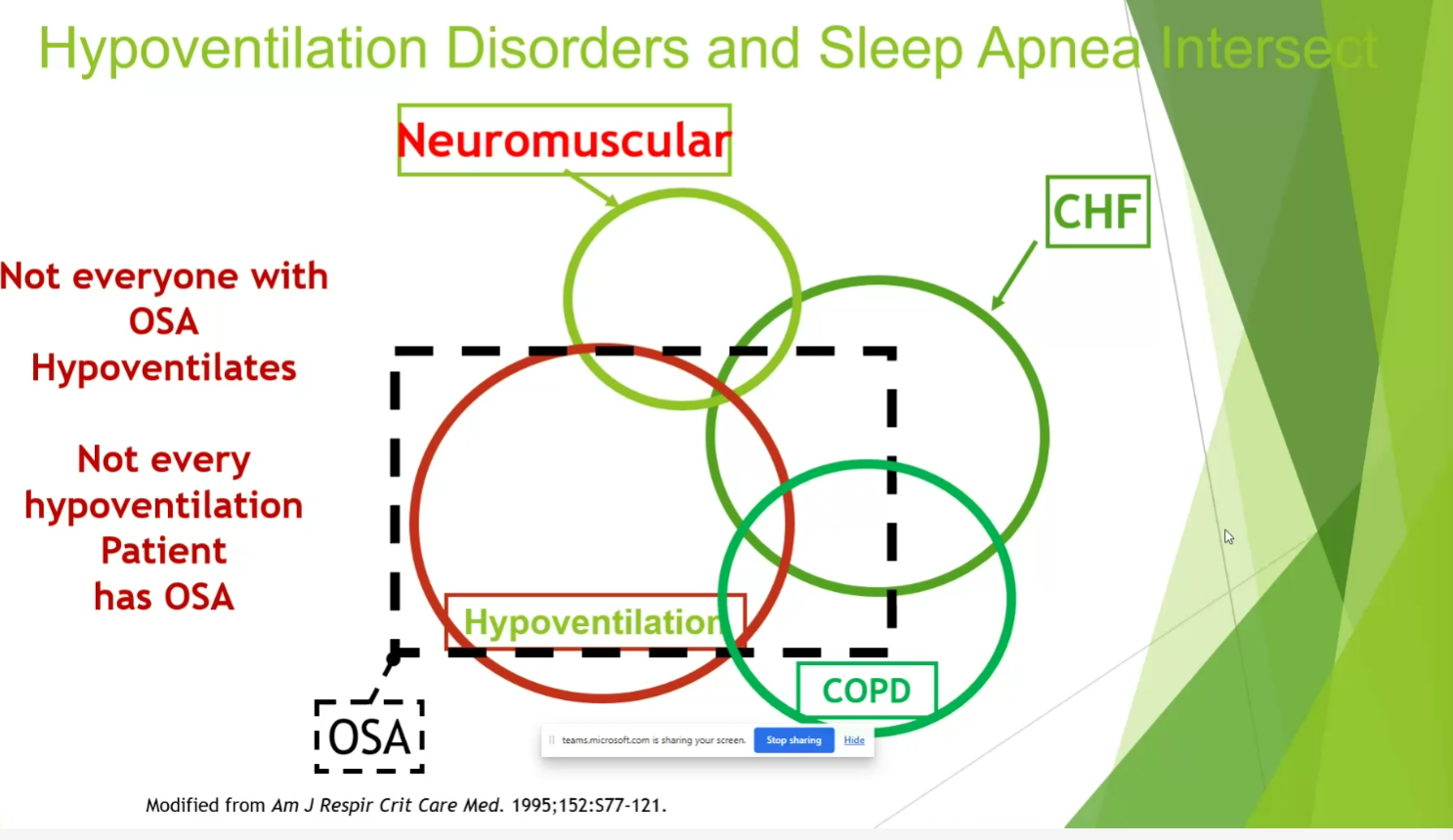
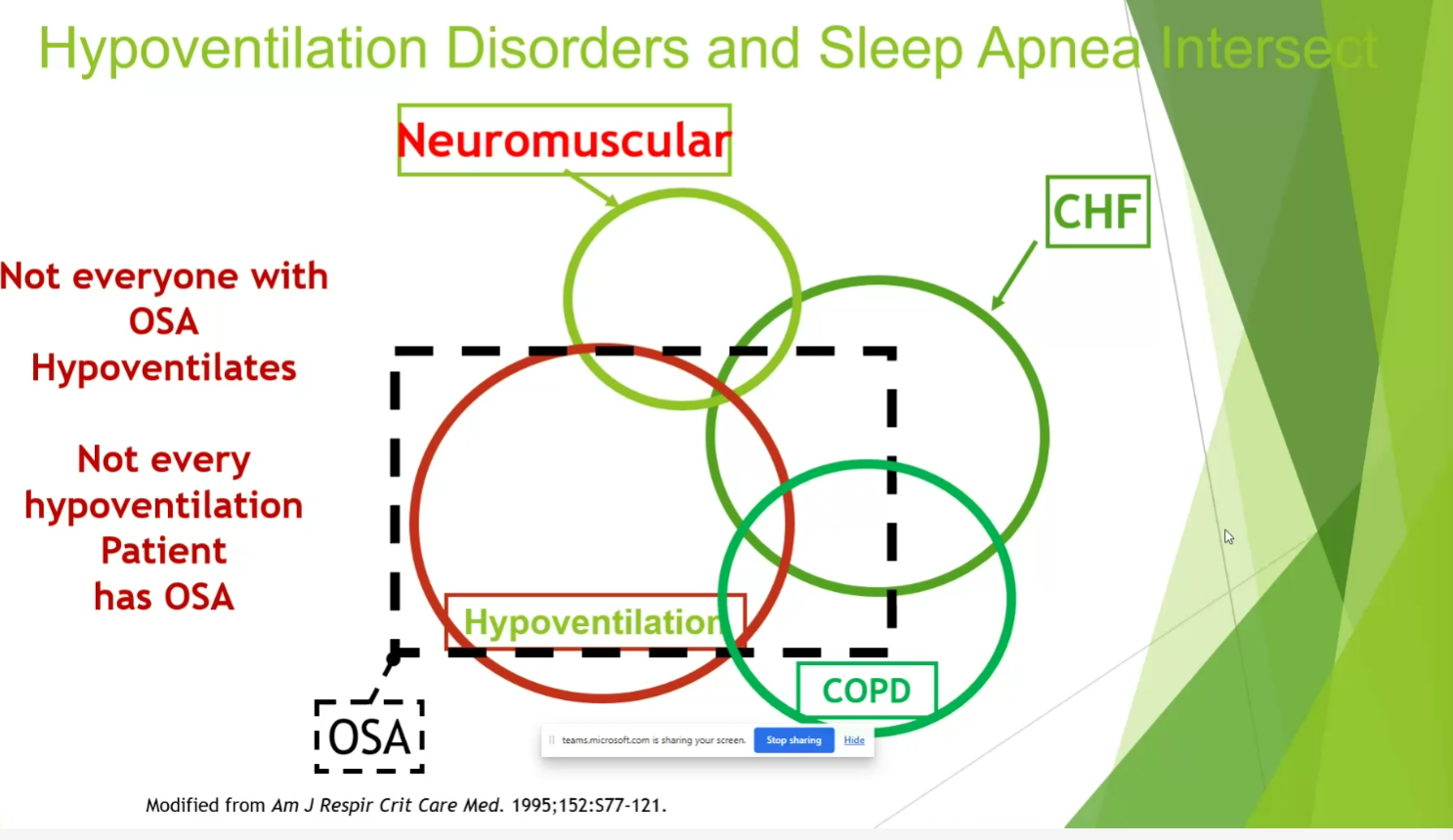
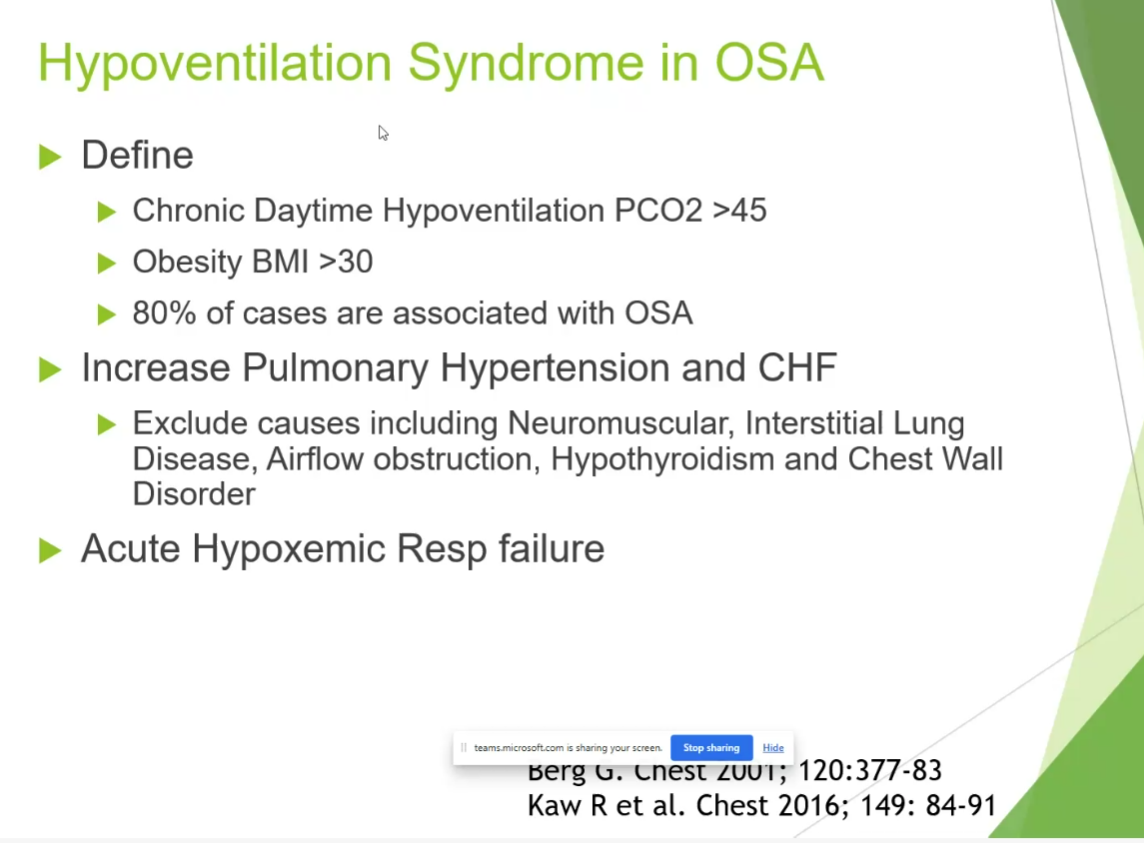
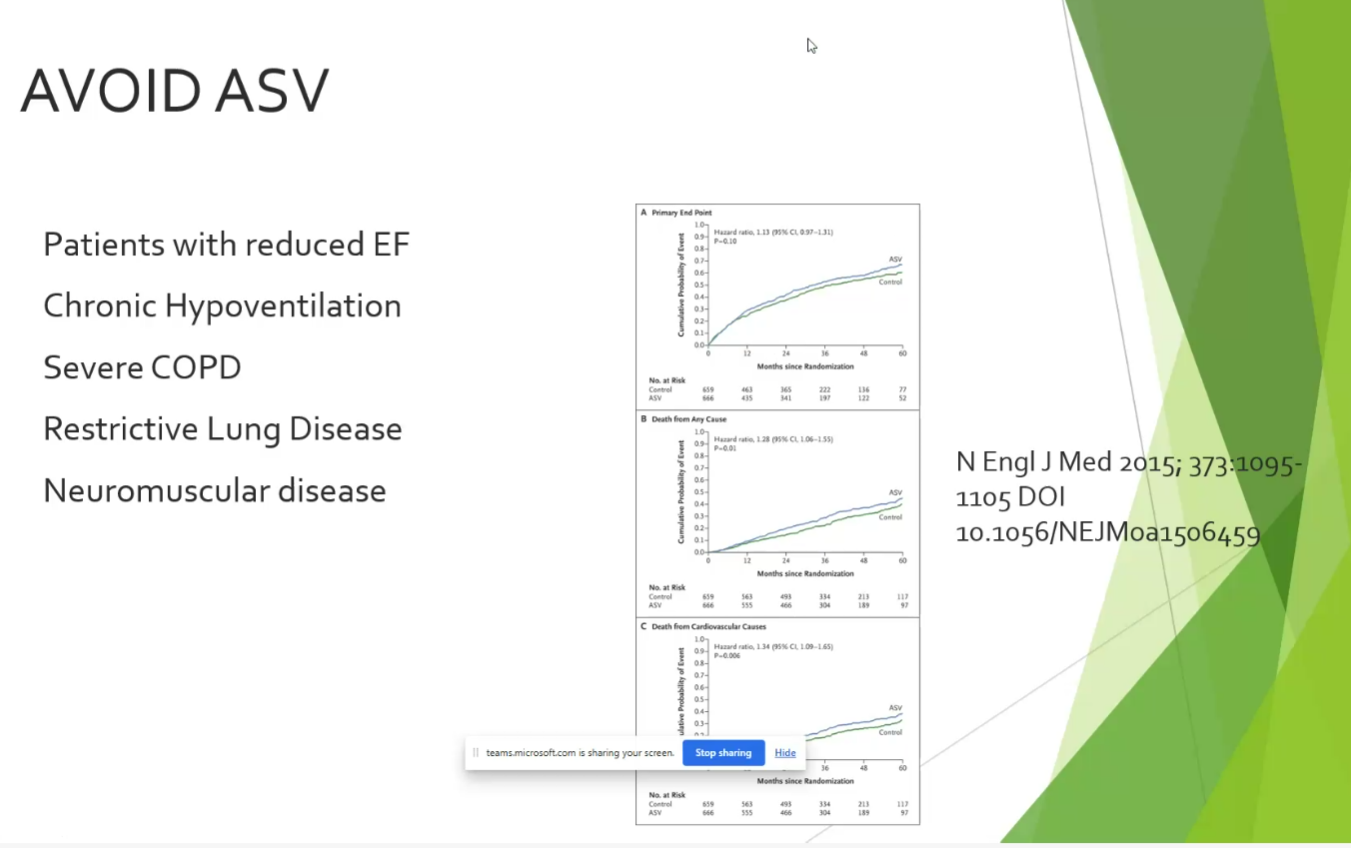
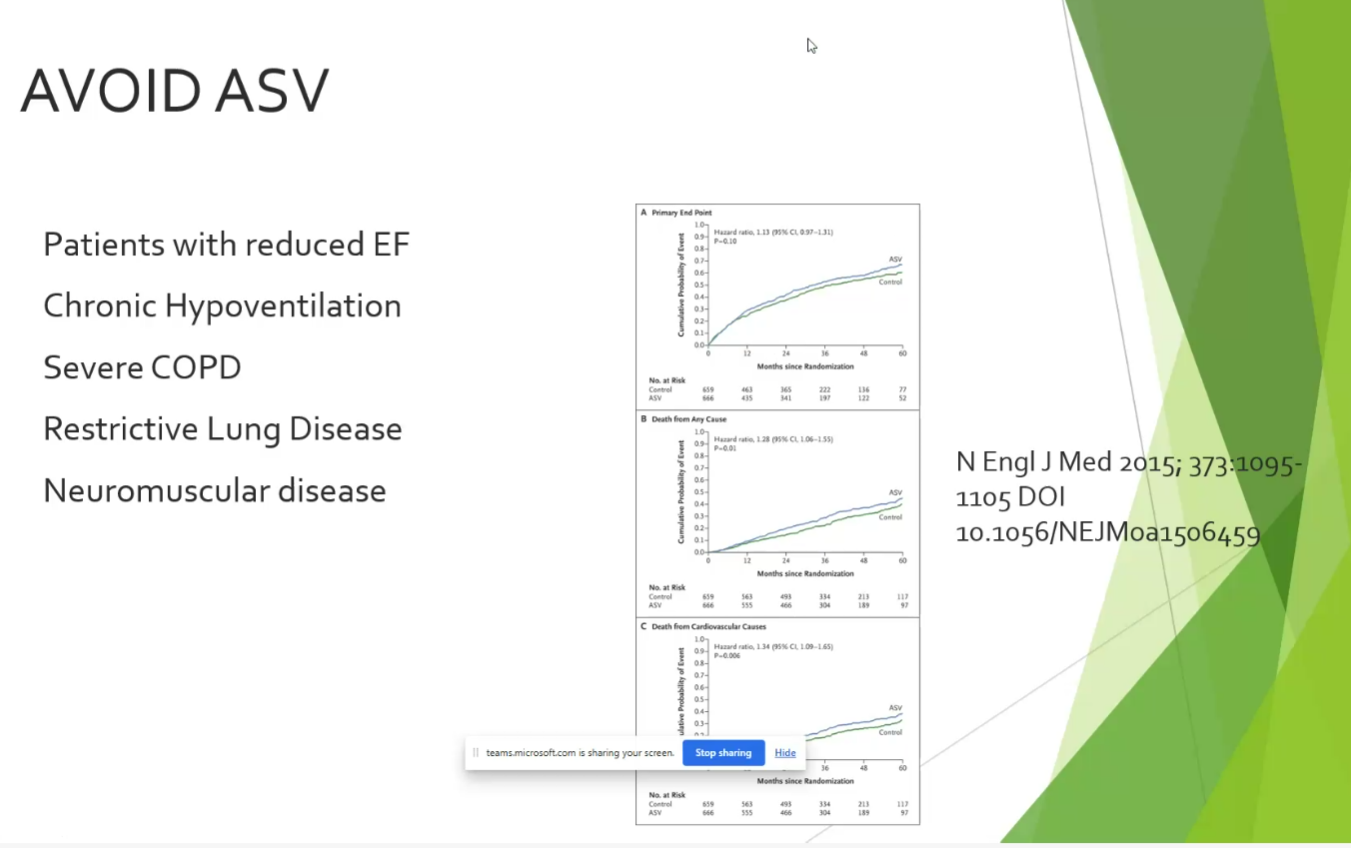
- up to 40% CHF, 15-20% NMD, up to 50% COPD, most of OSA
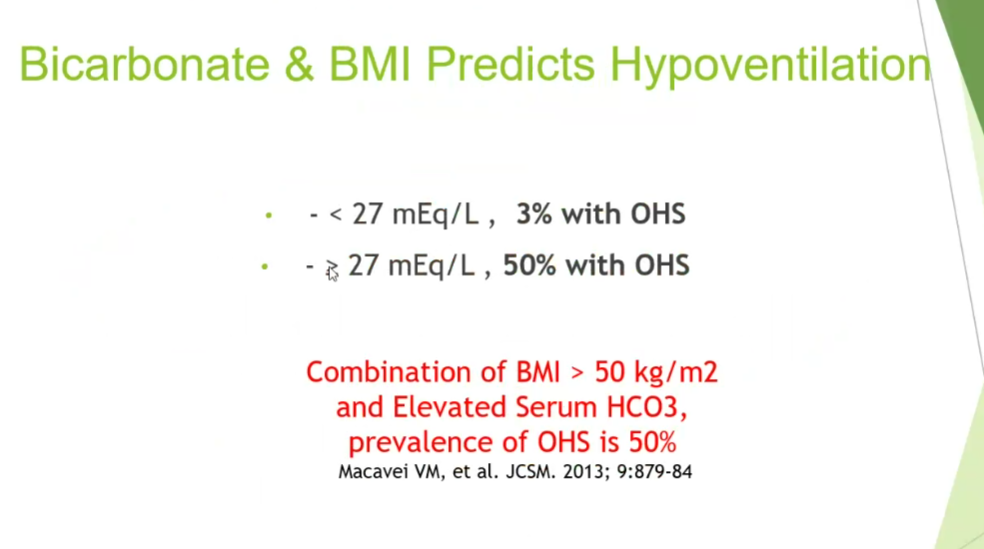
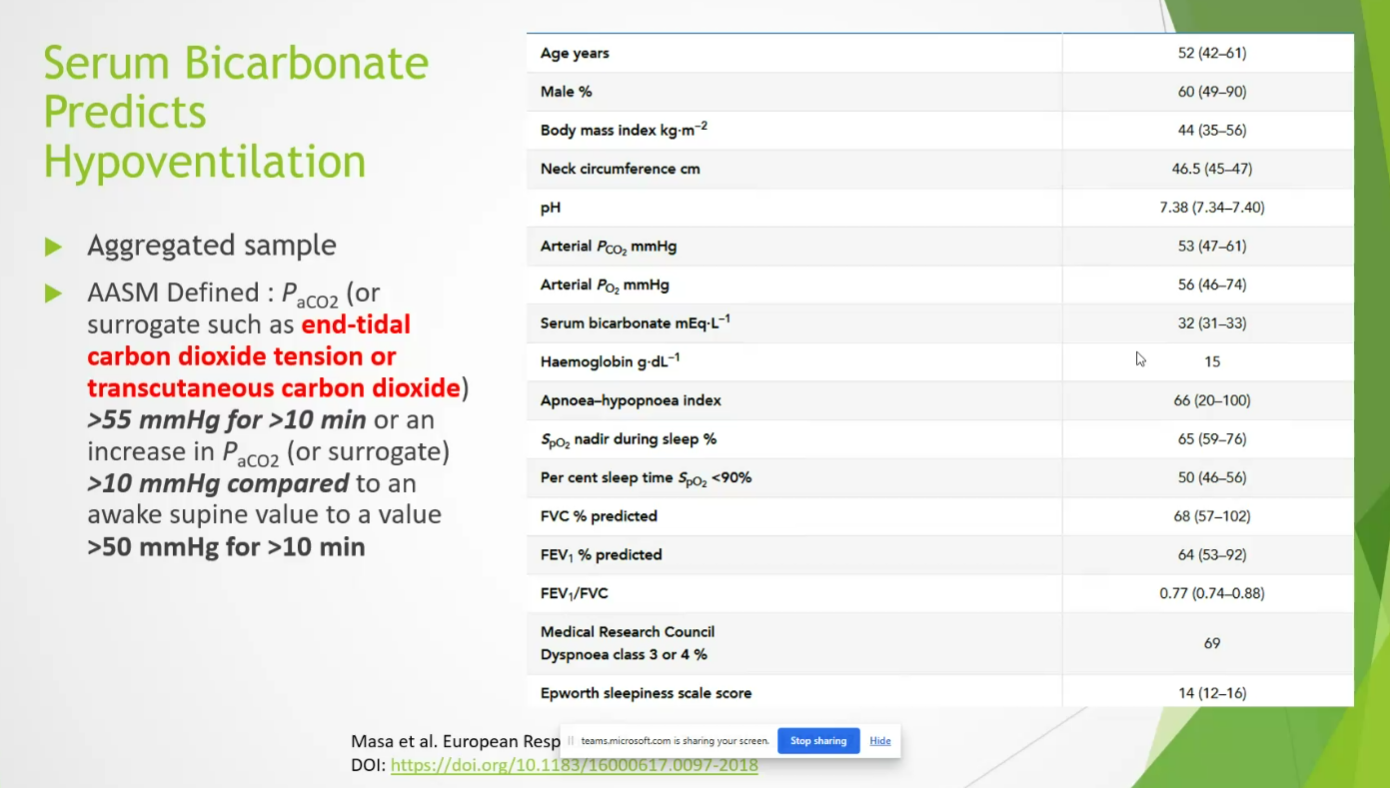
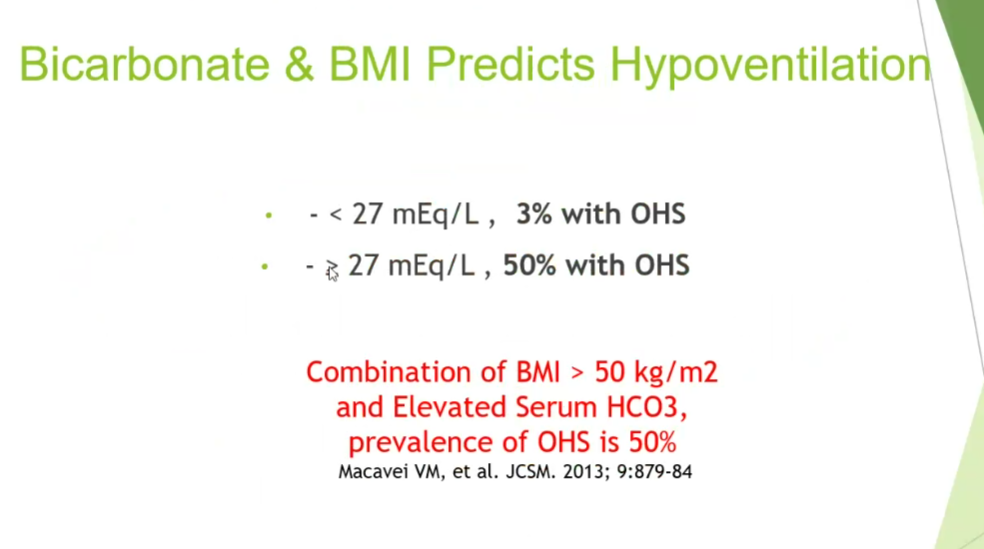
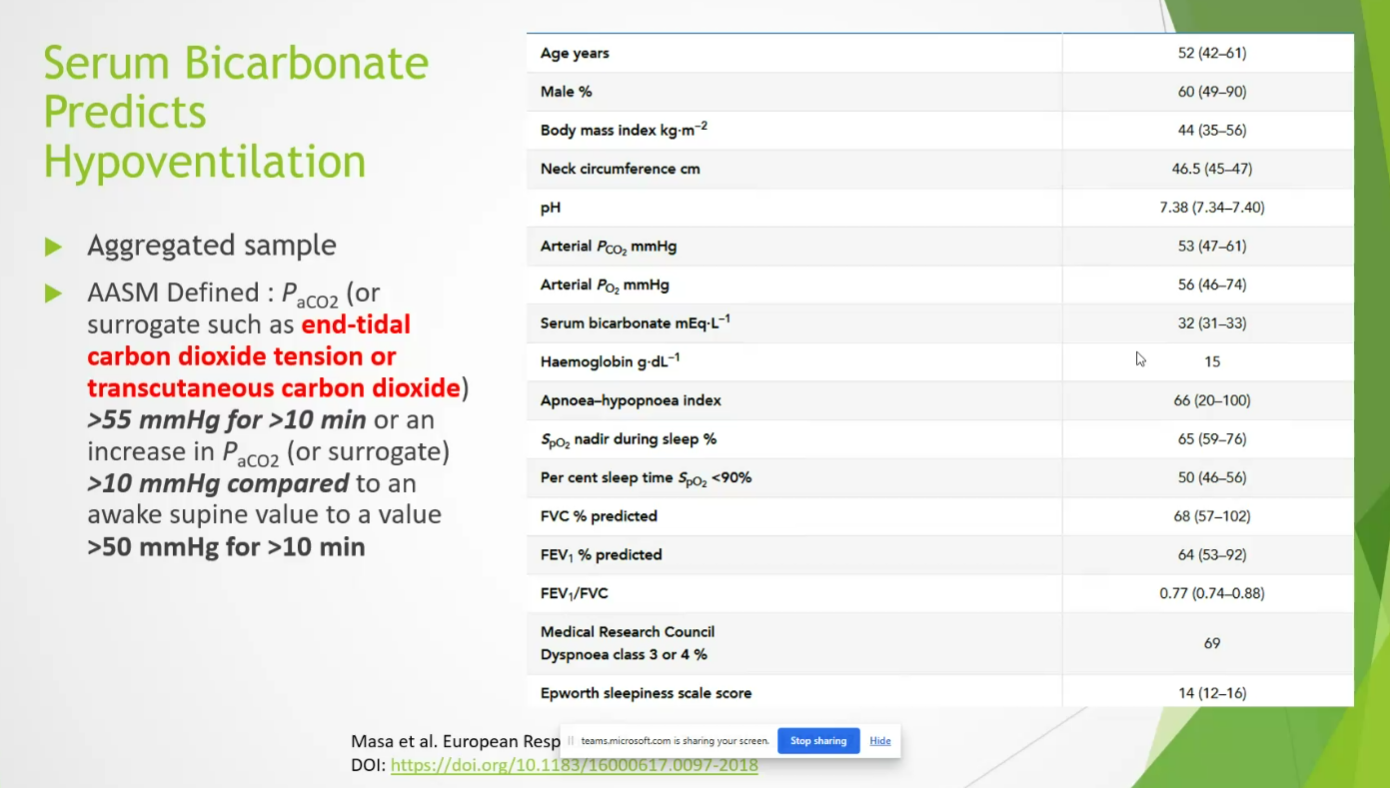
- bicarb predicts in pts with elevated BMI
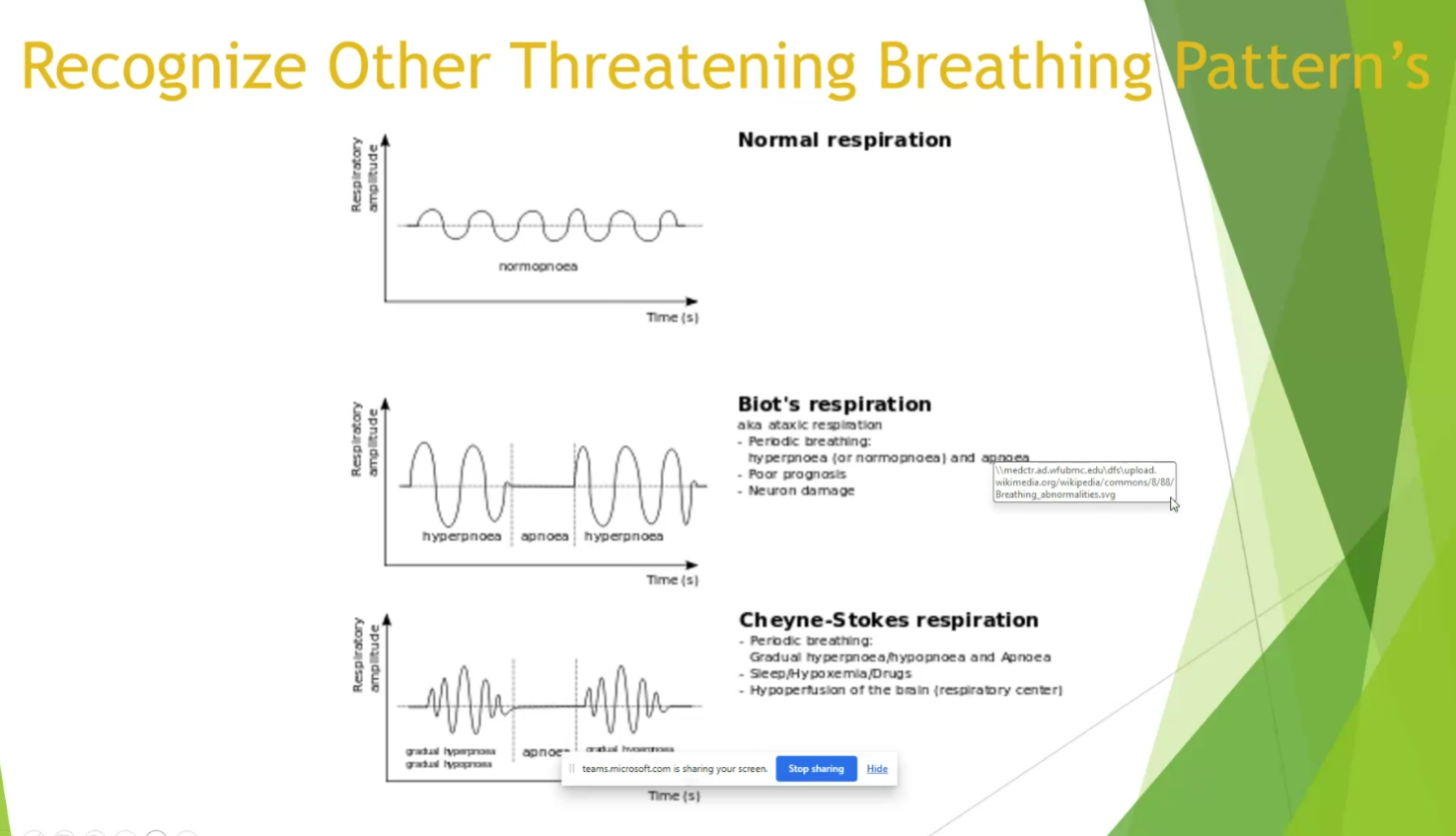
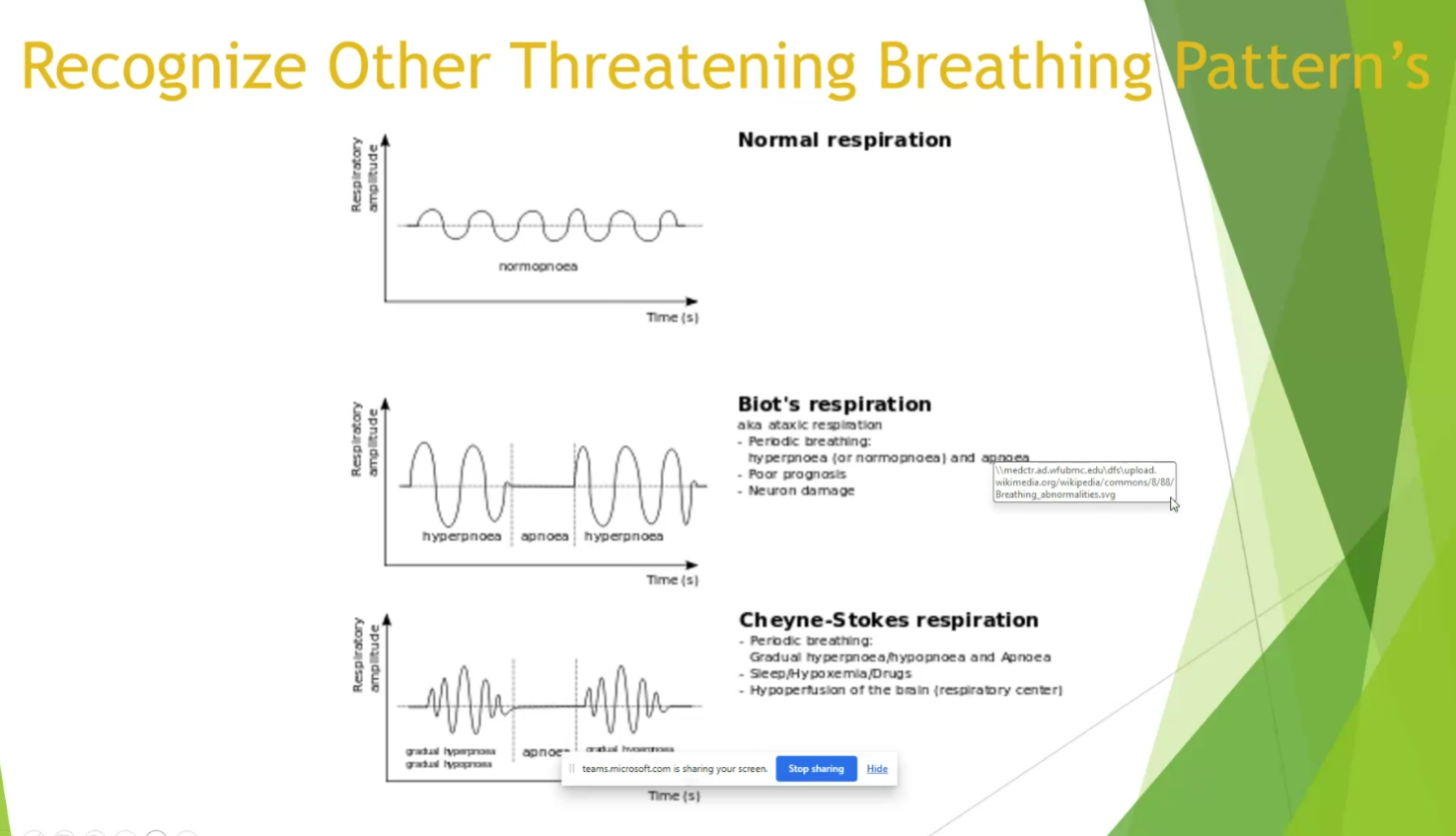
- ataxic breathing
- central pauses can become as long as 2-3 min with agonal breathing
- often in opioid users
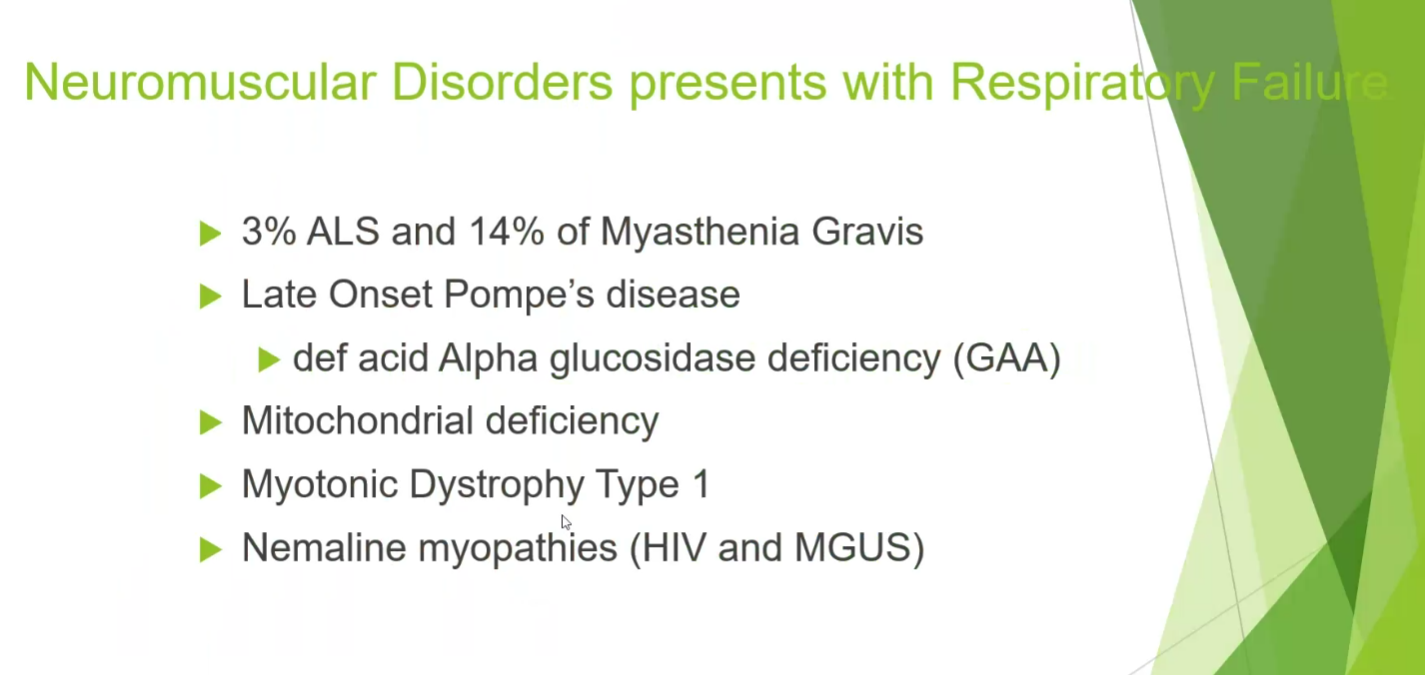
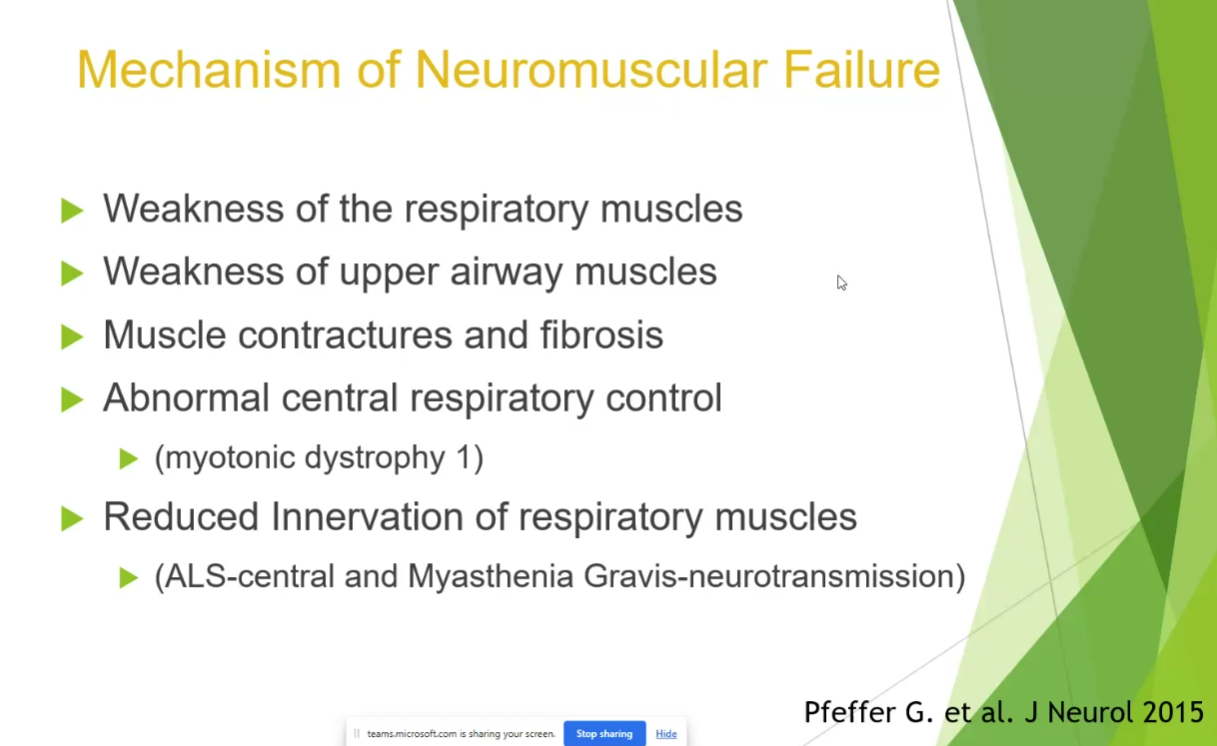
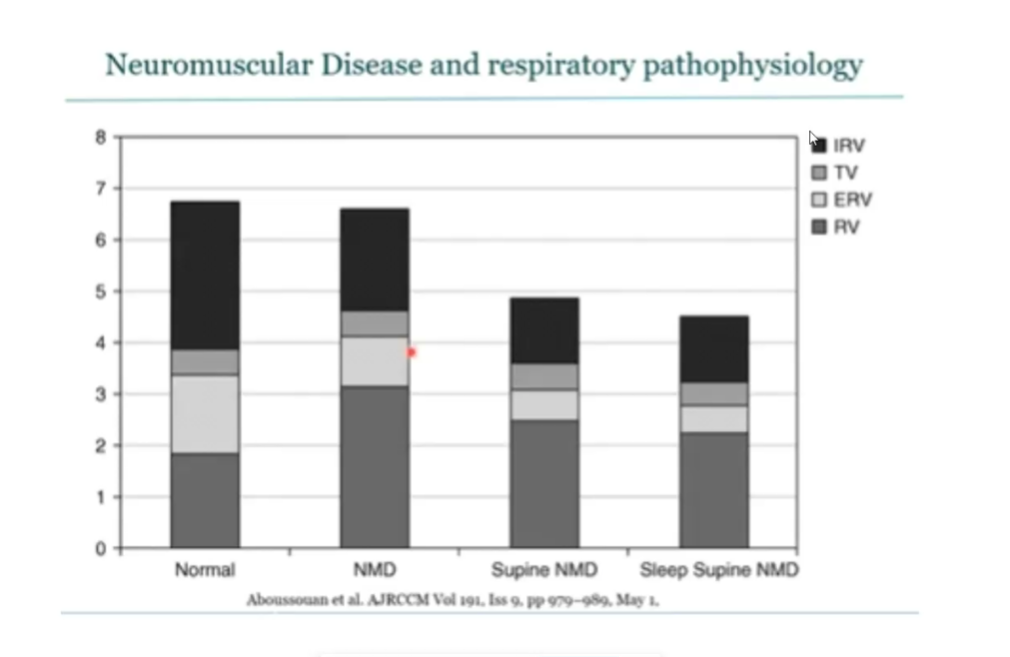
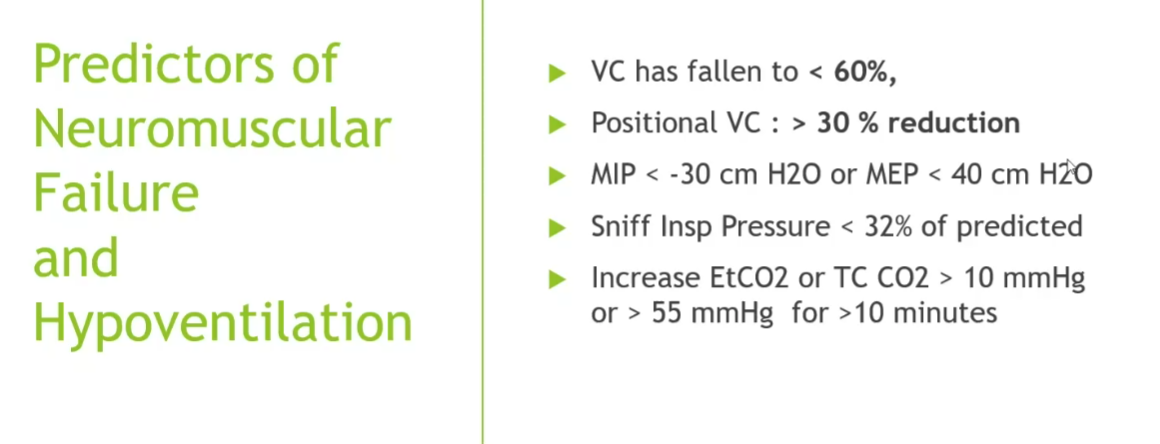
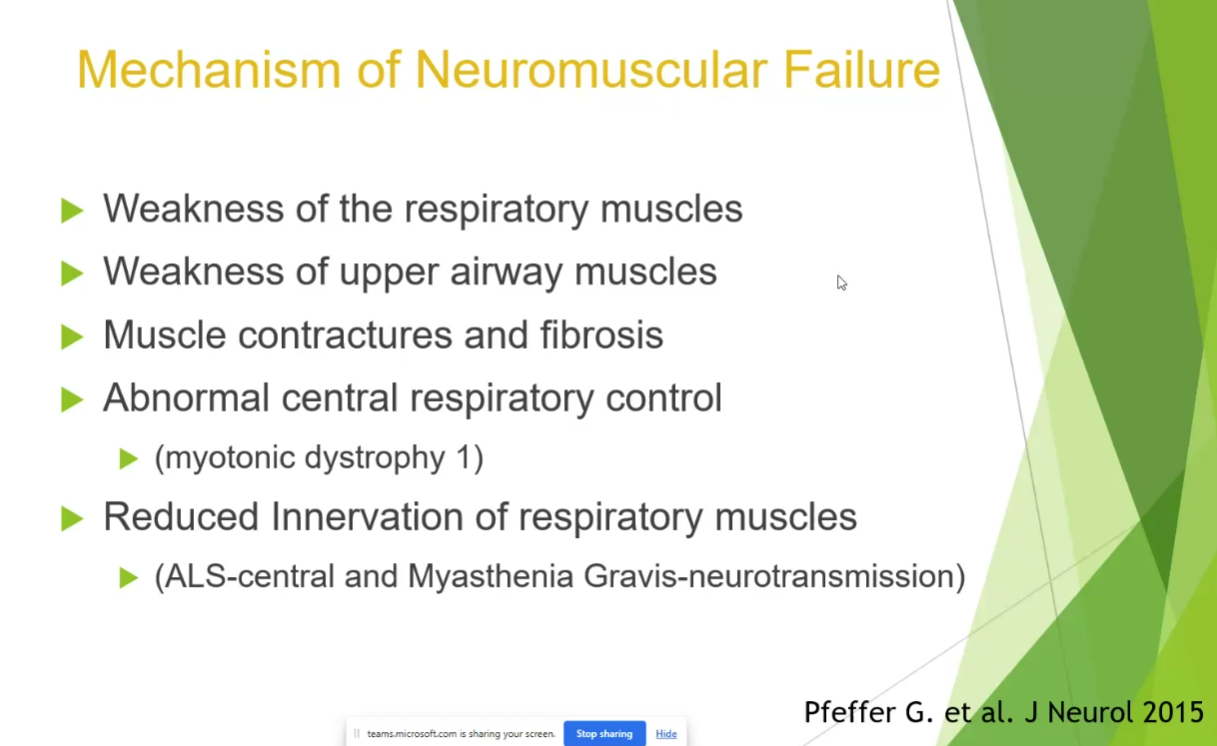
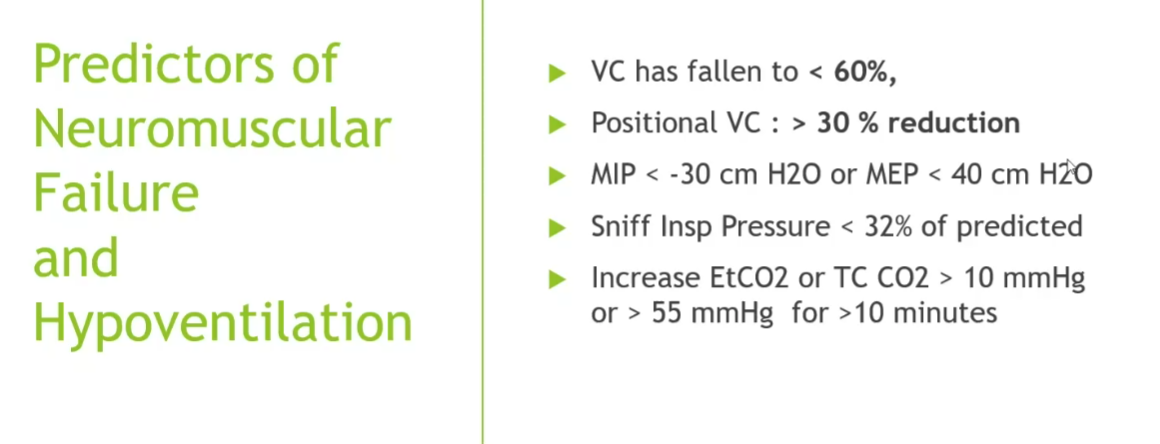
Neuromuscular disorders
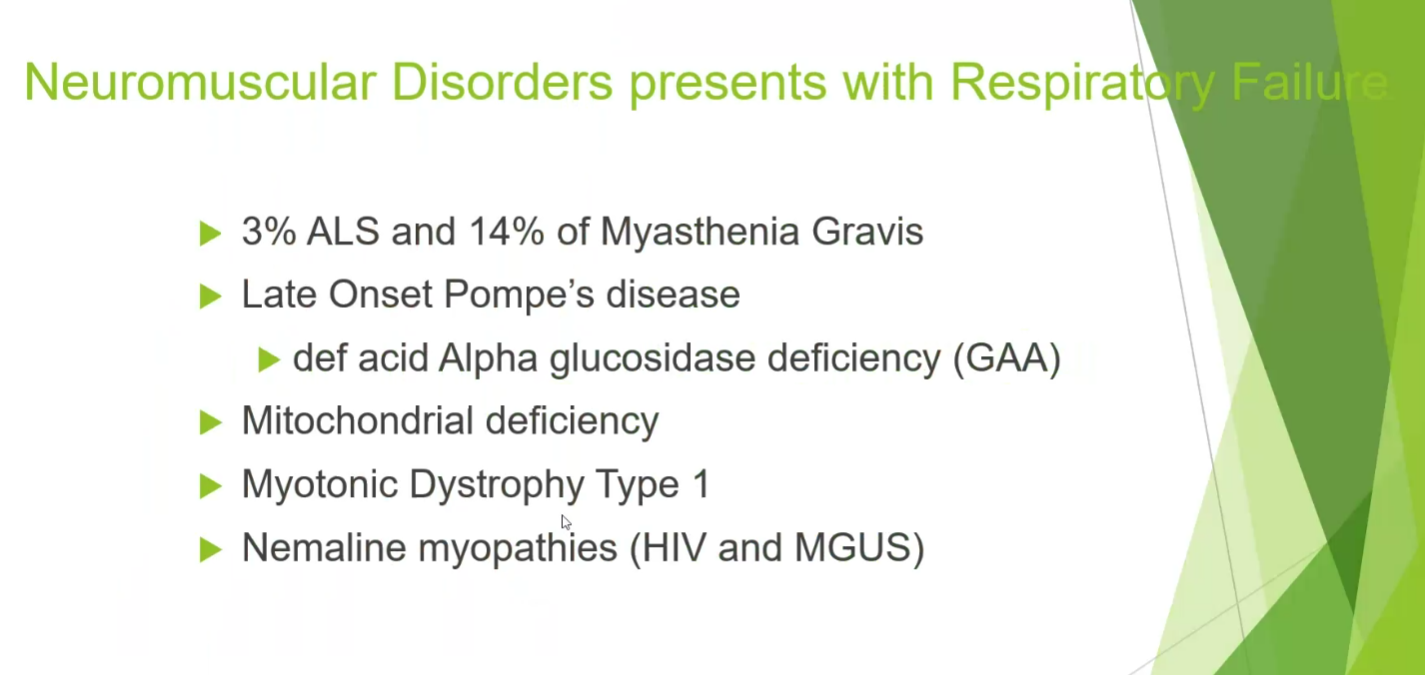
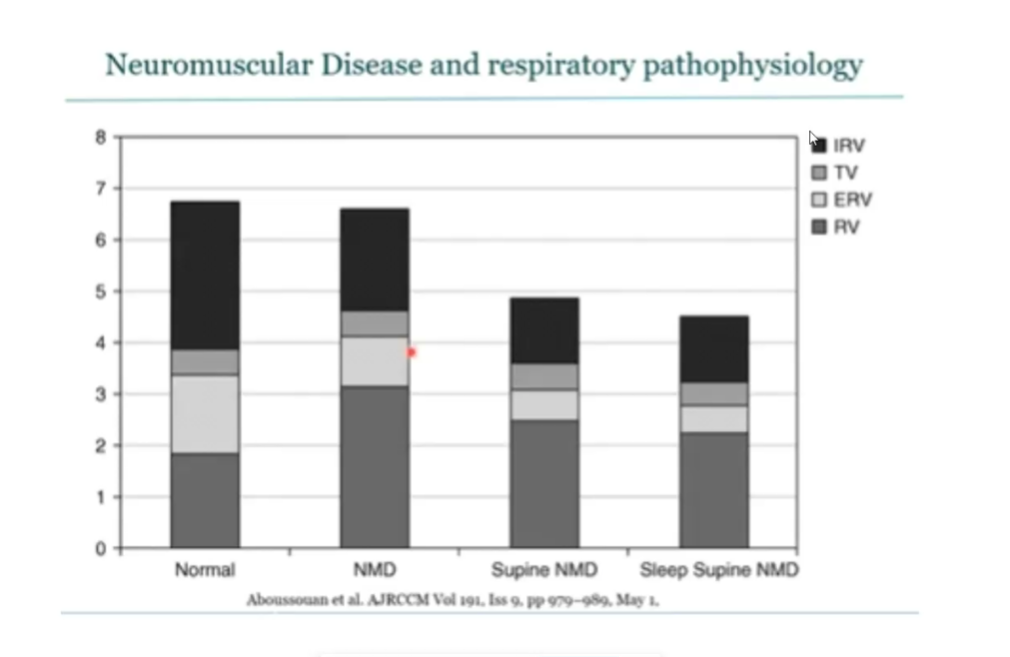
- laying flat can show dramatic drops
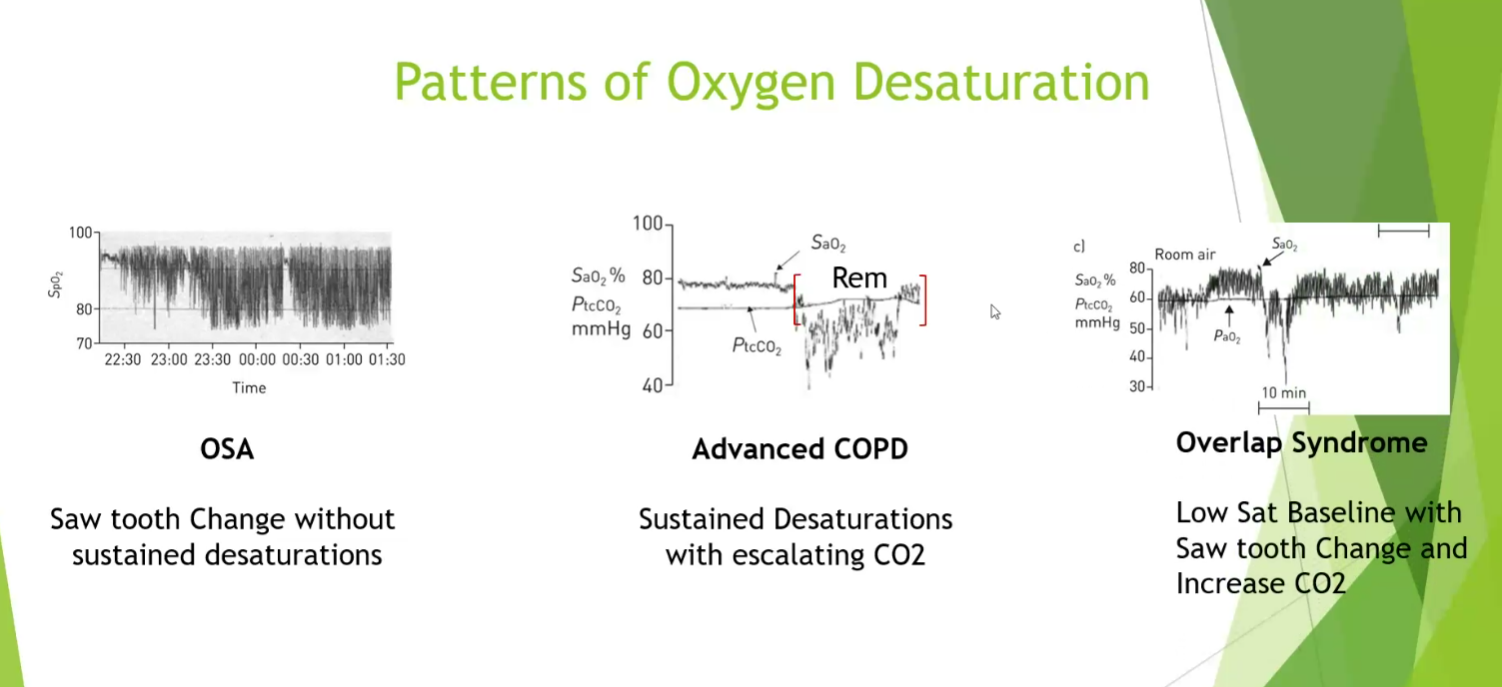
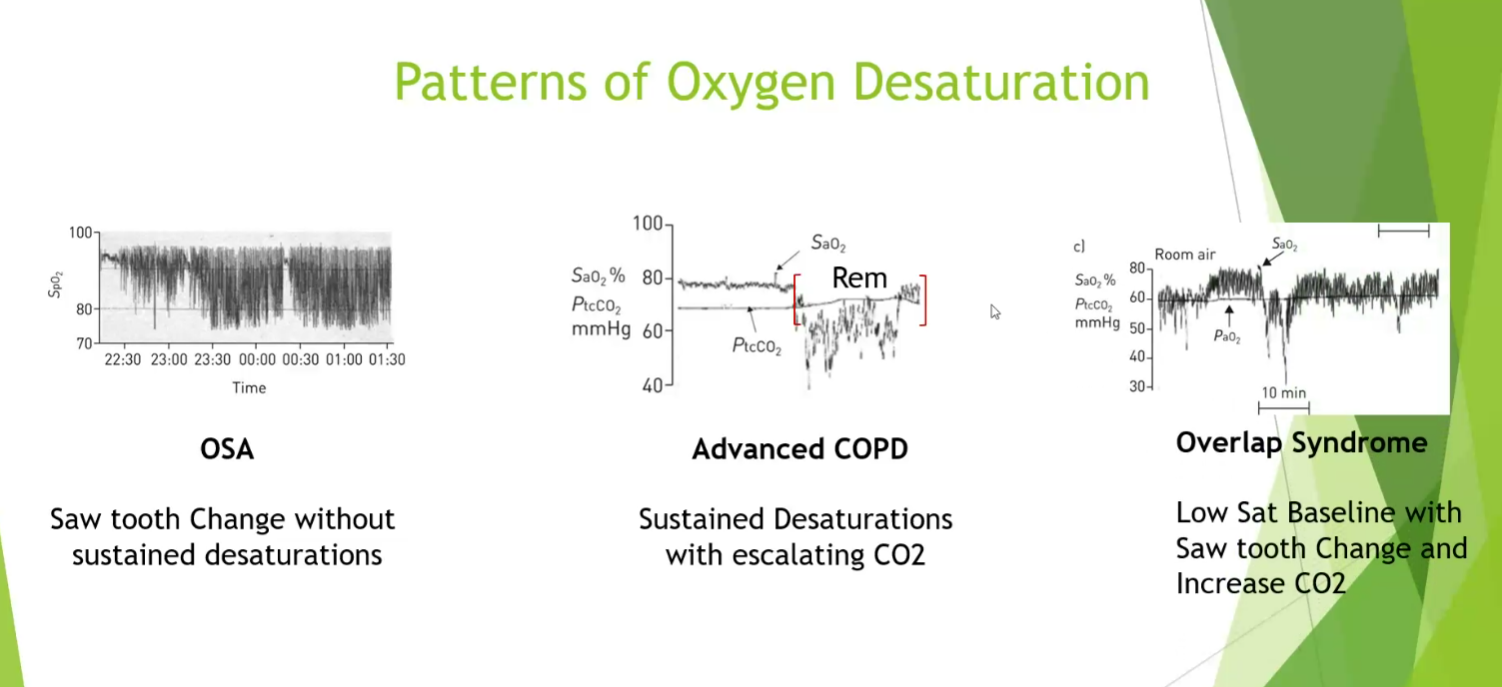
- OSA: quick drops and recovery
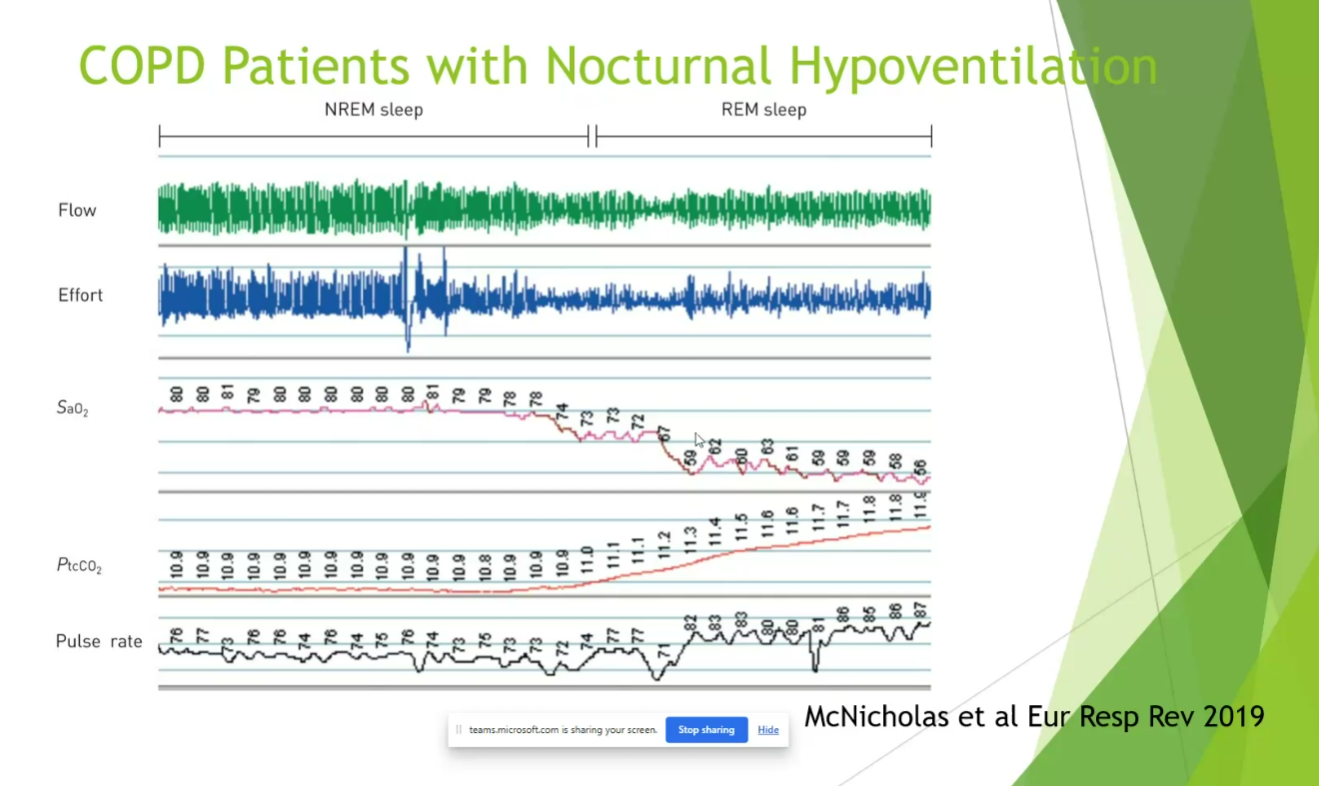
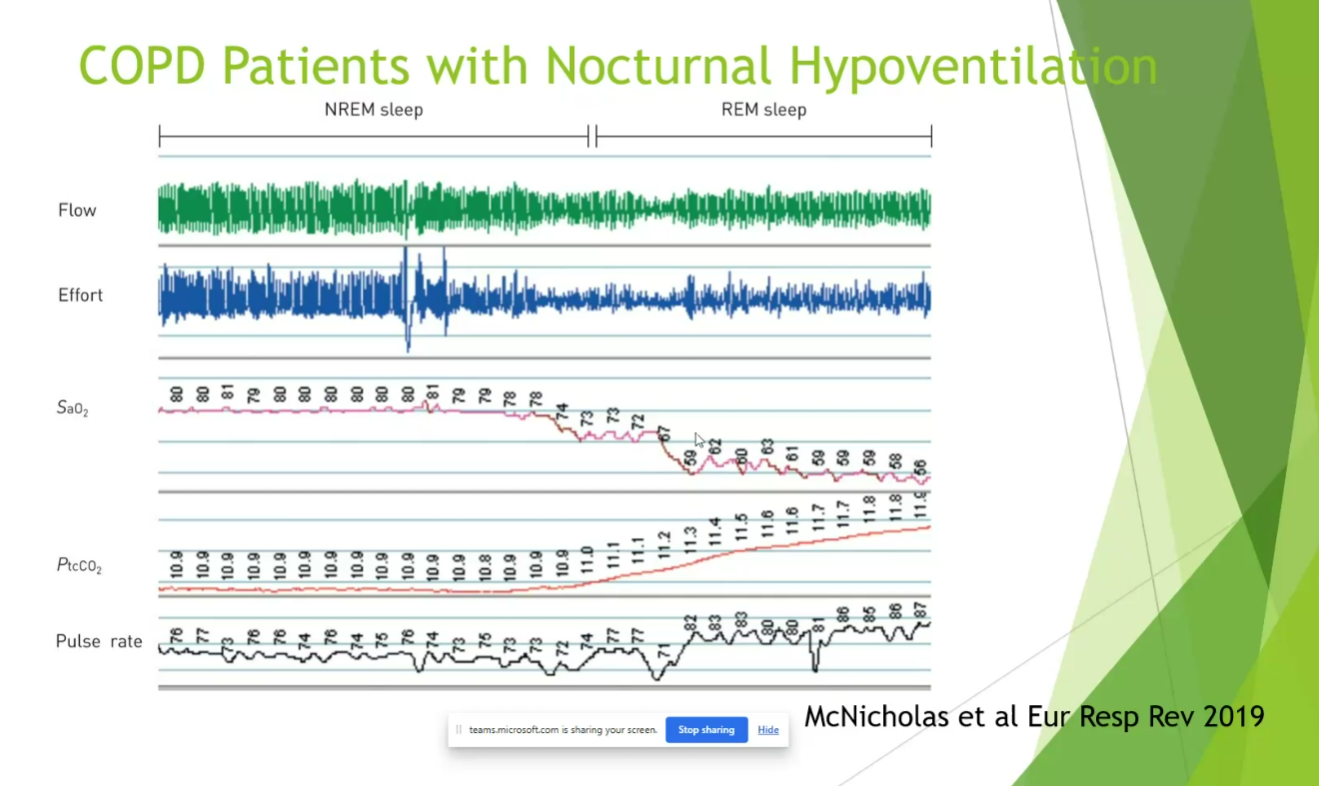
- COPD: sustained desat with CO2 go up
- Combined: dramatic changes in both CO2 and desat
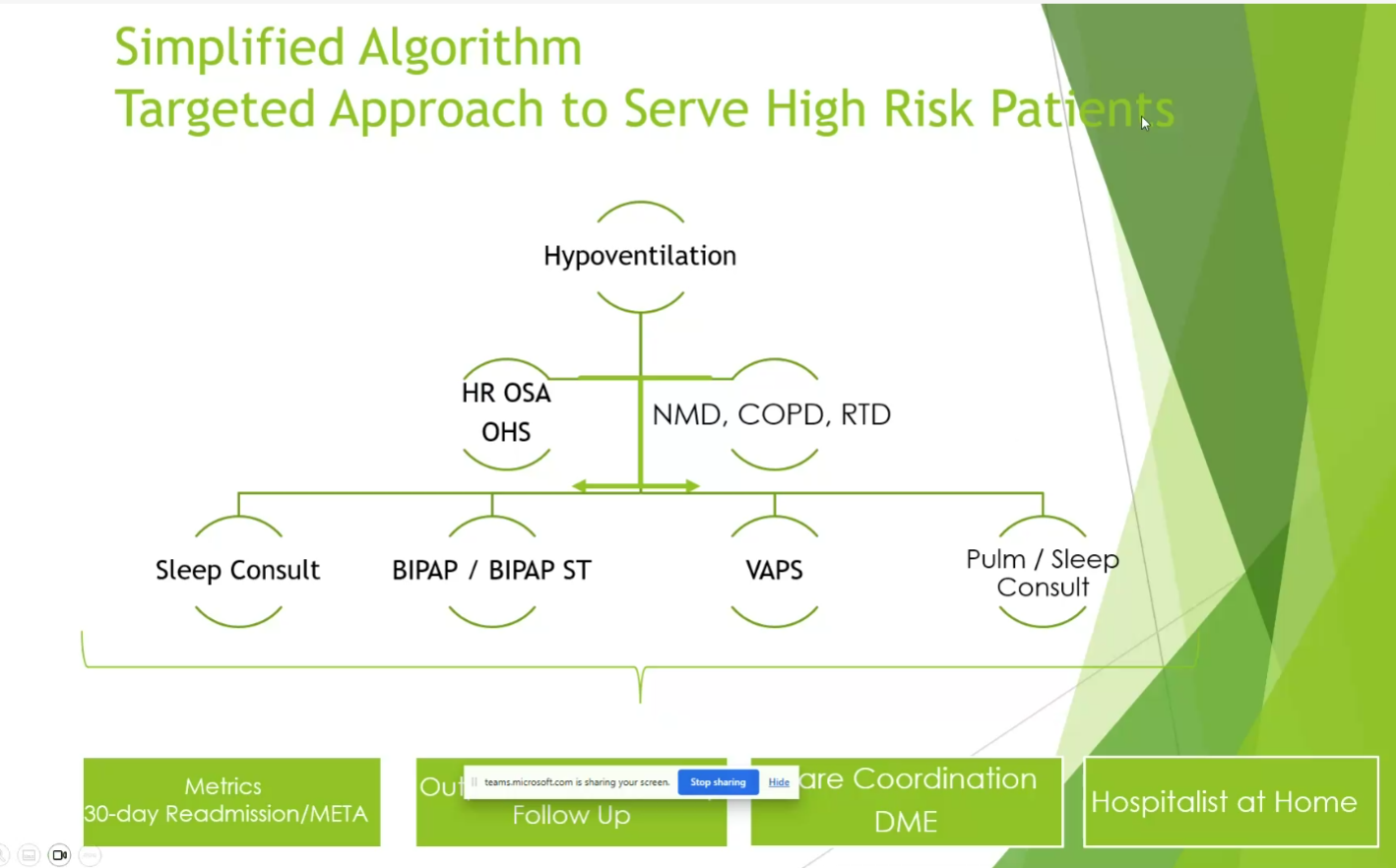
- not every needs NIV
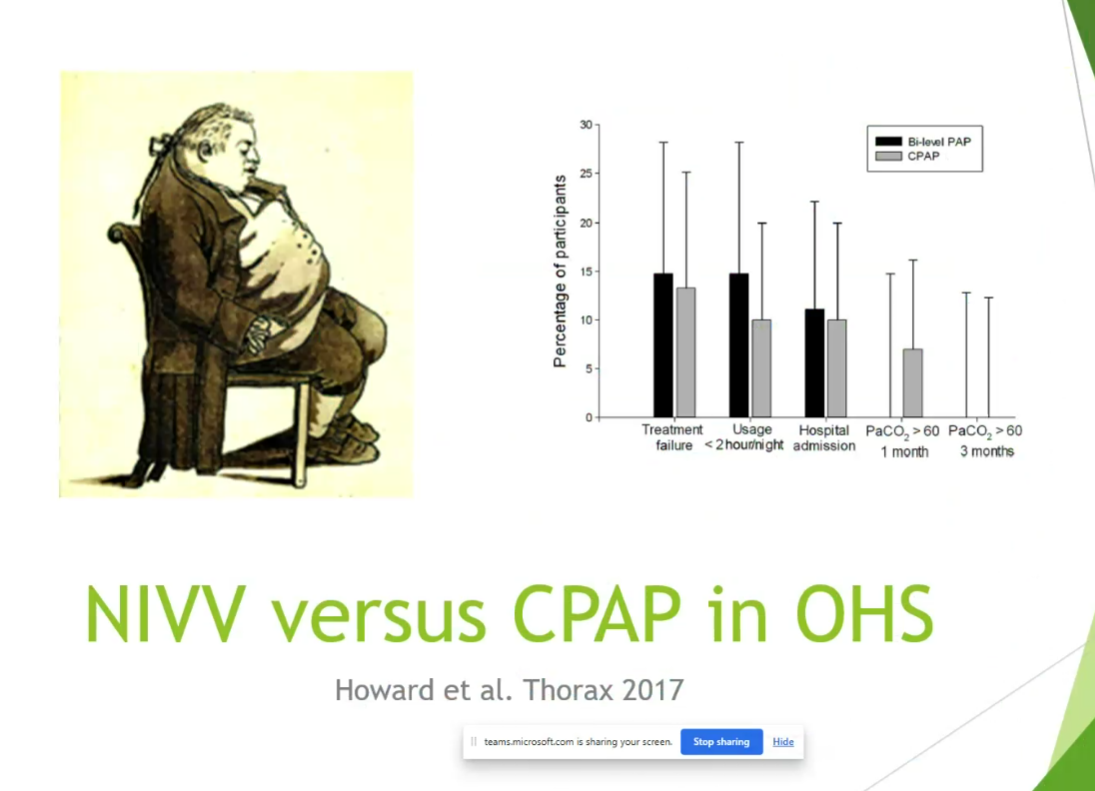
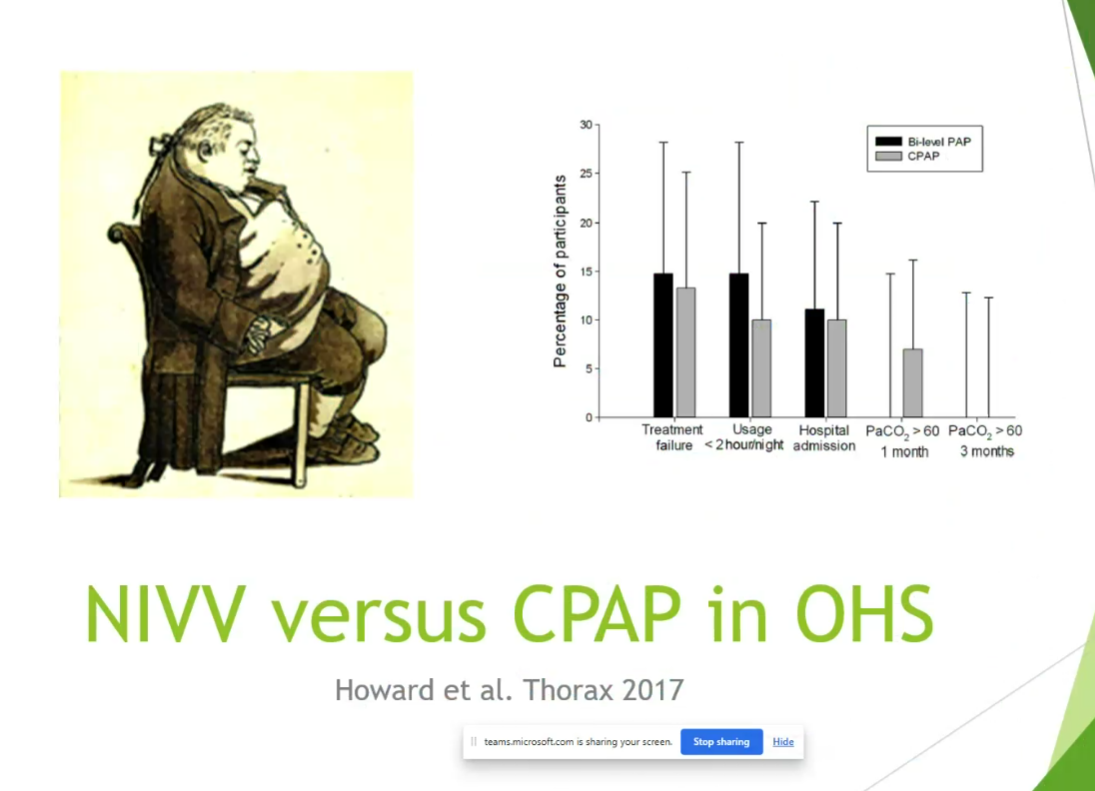
- CPAP effective in a lot of cases, will improve CO2 but not as fast as Bipap.
- CPAP can treat OHS with elevated CO2 if stable
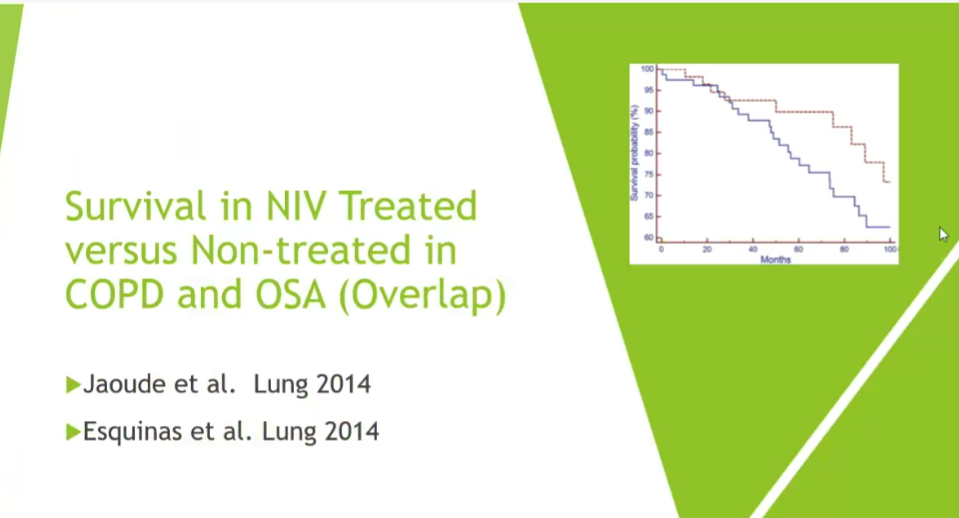
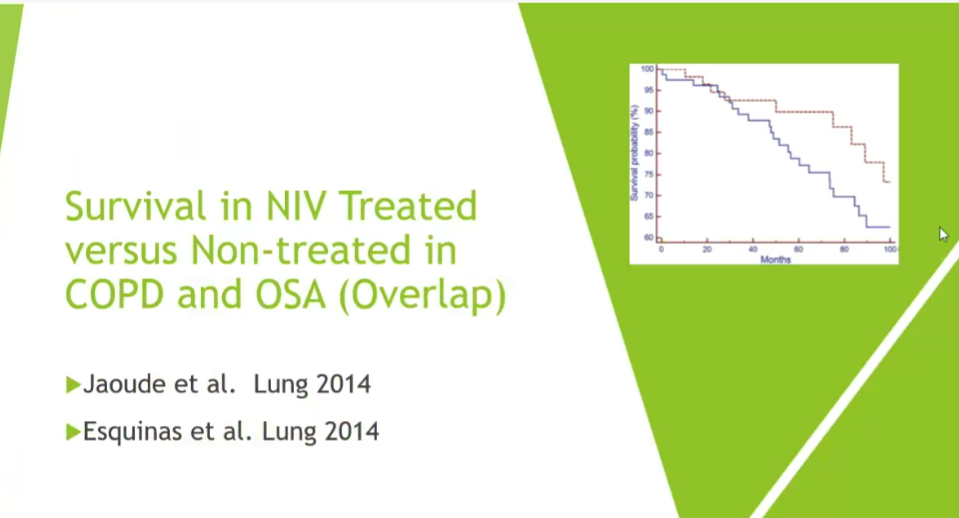
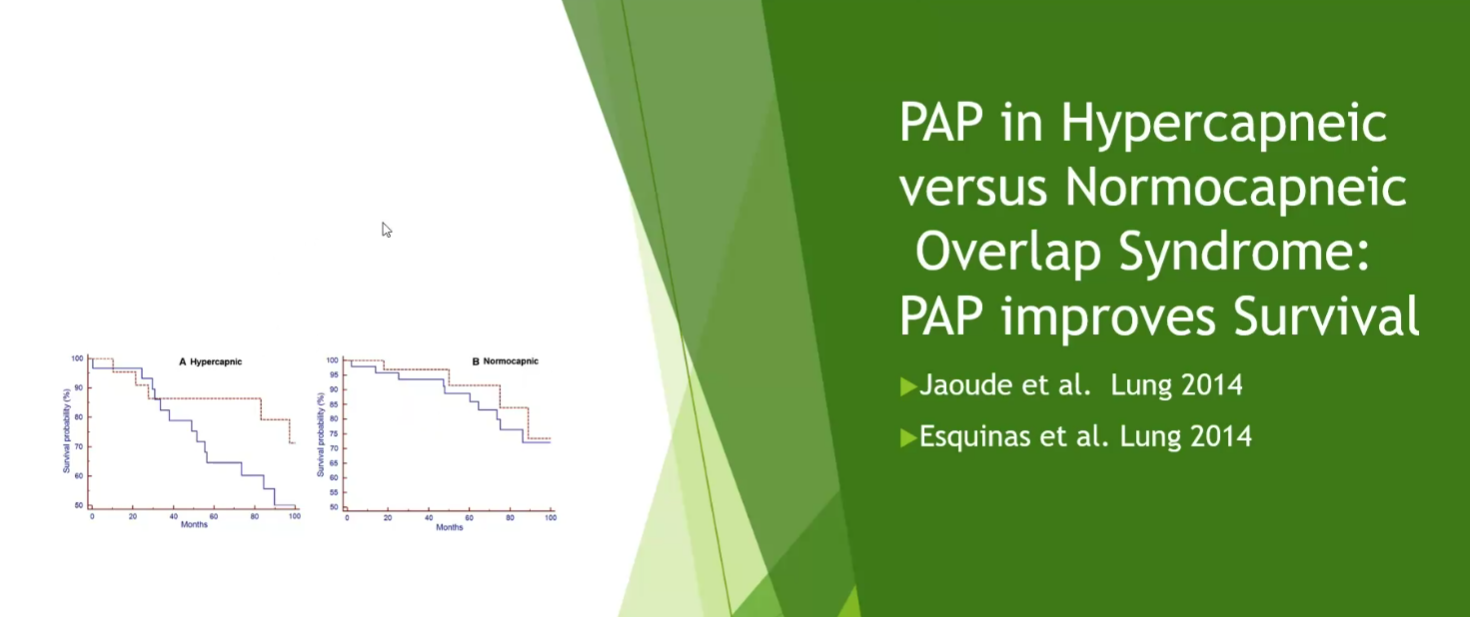
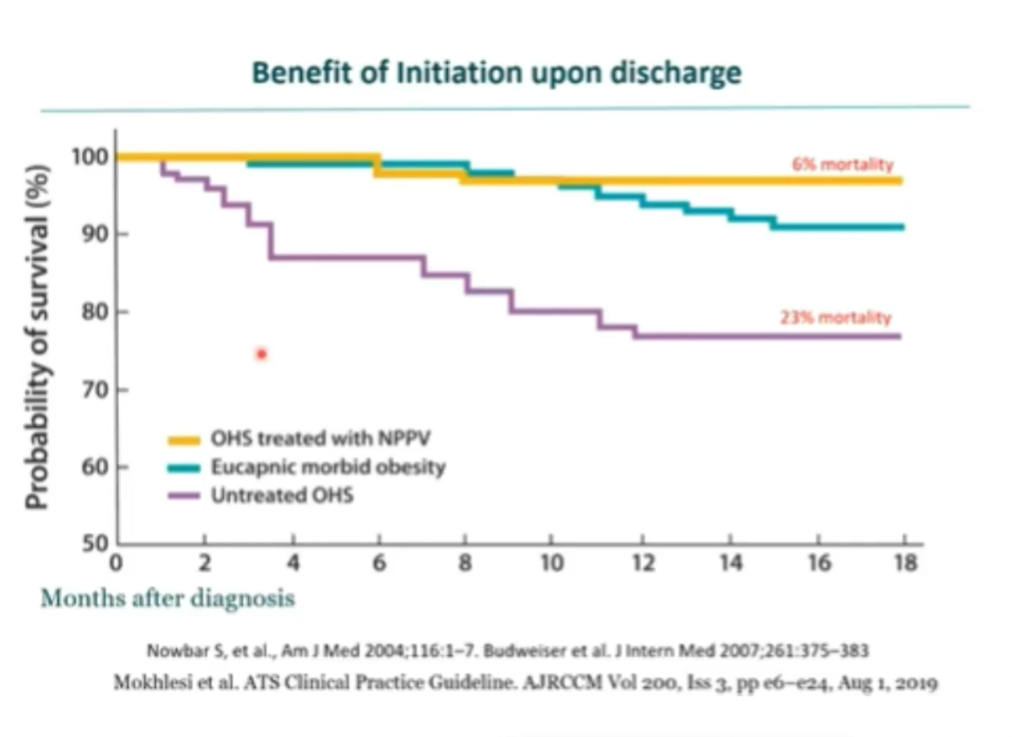
- survival in NIV treated groups is higher with NIV when there is overlap
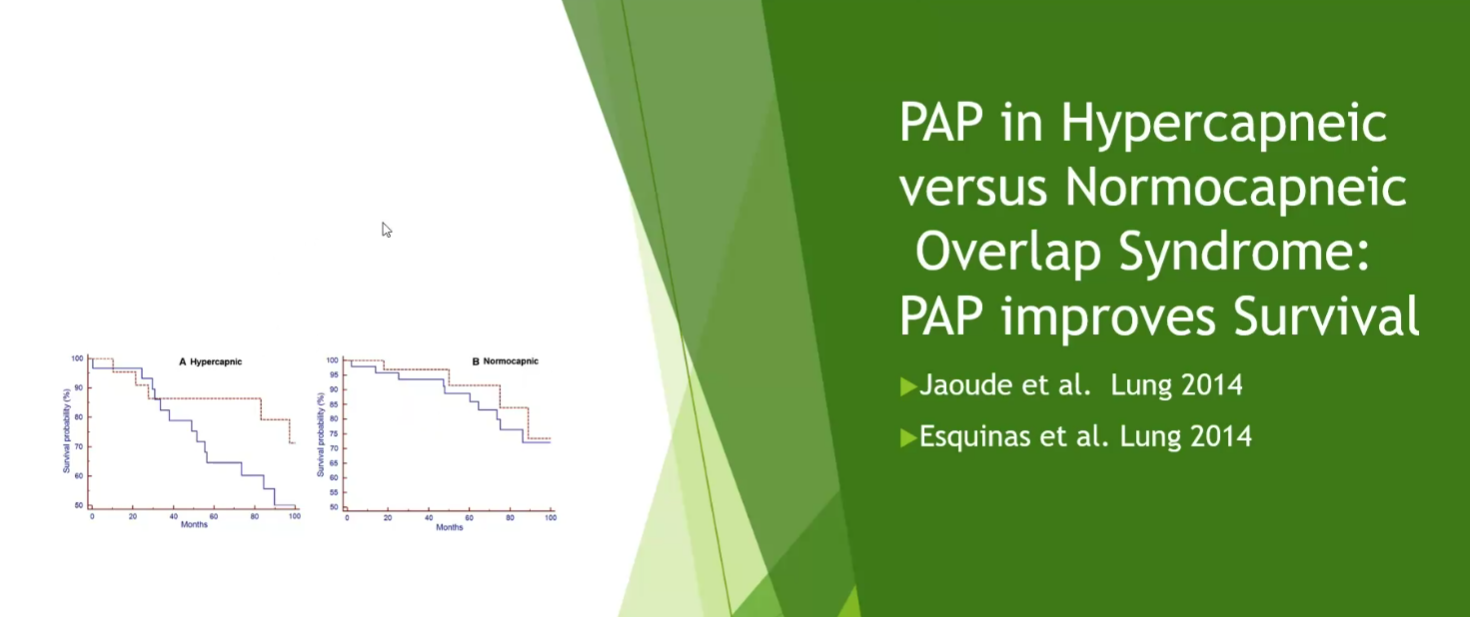
- normocapneic patient doesn’t receive as much benefit from bipap
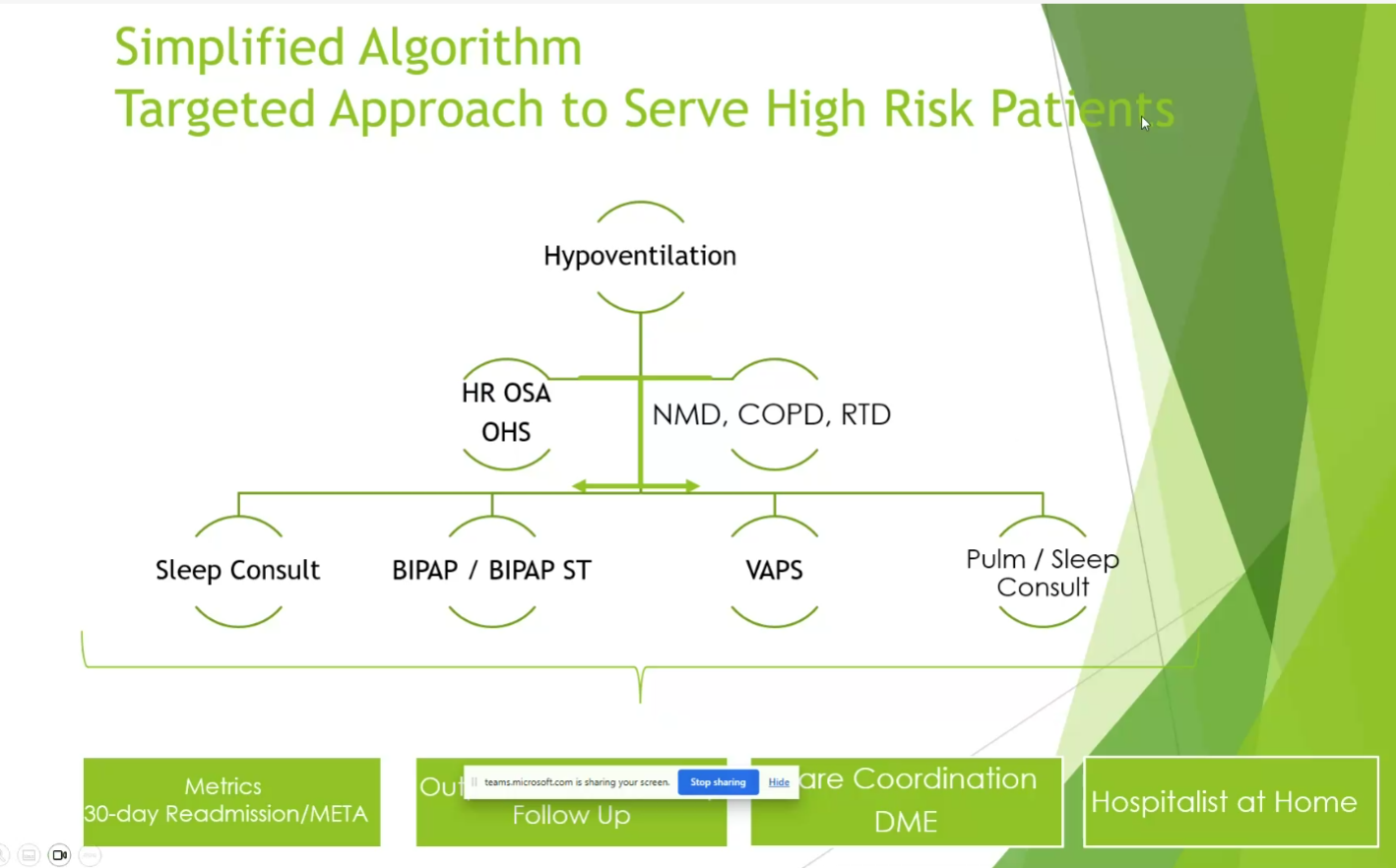
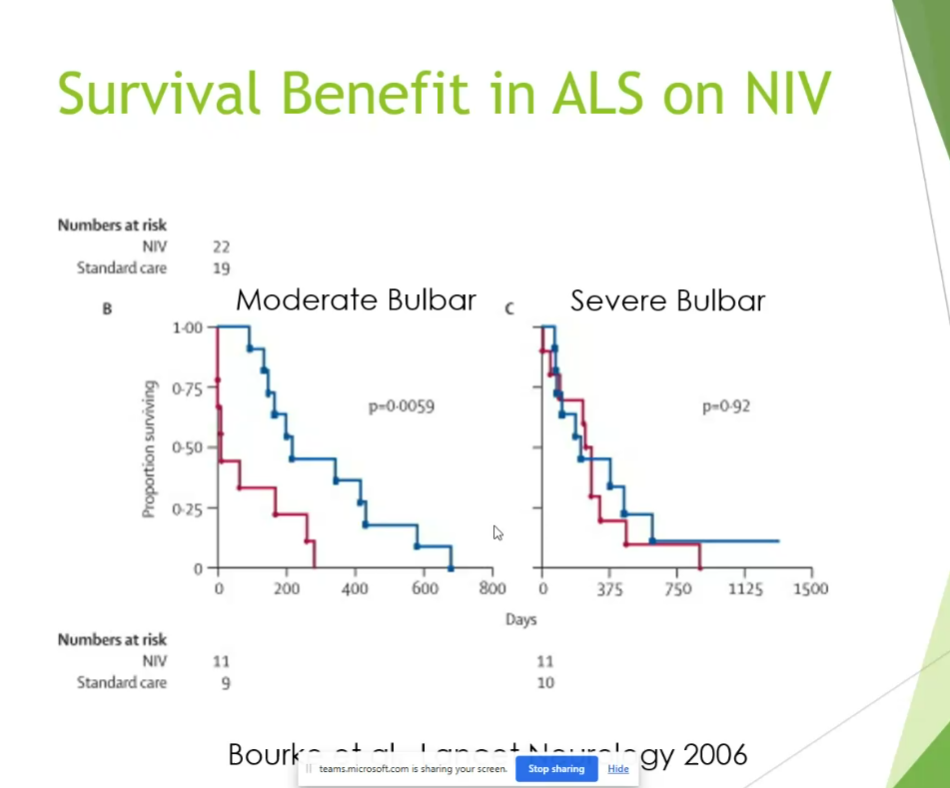
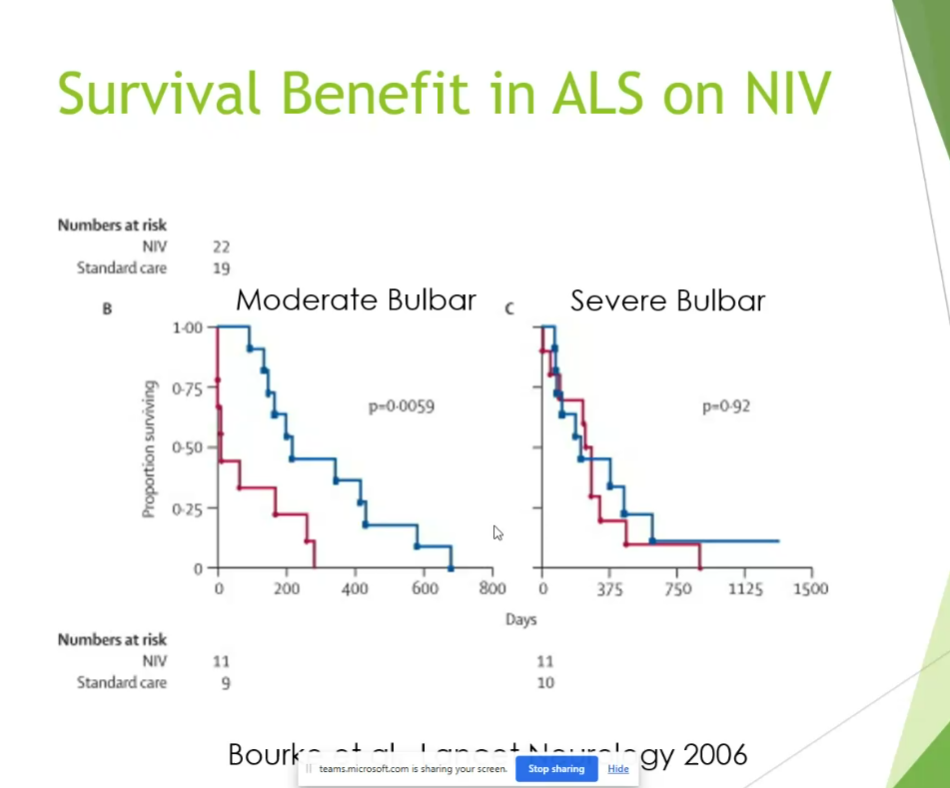
- ALS pts with severe bulbar symptoms don’t benefit as much
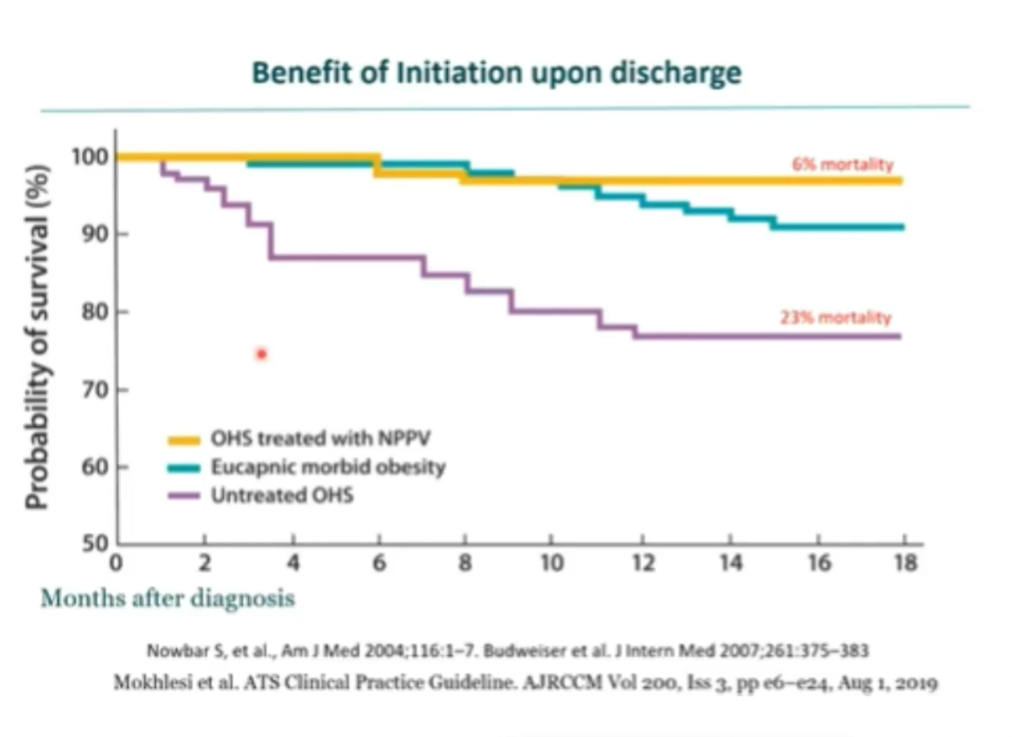
- reduction in mortality less so in eucapnic morbid obesity

- correcting CO2 maximally even shows benefit
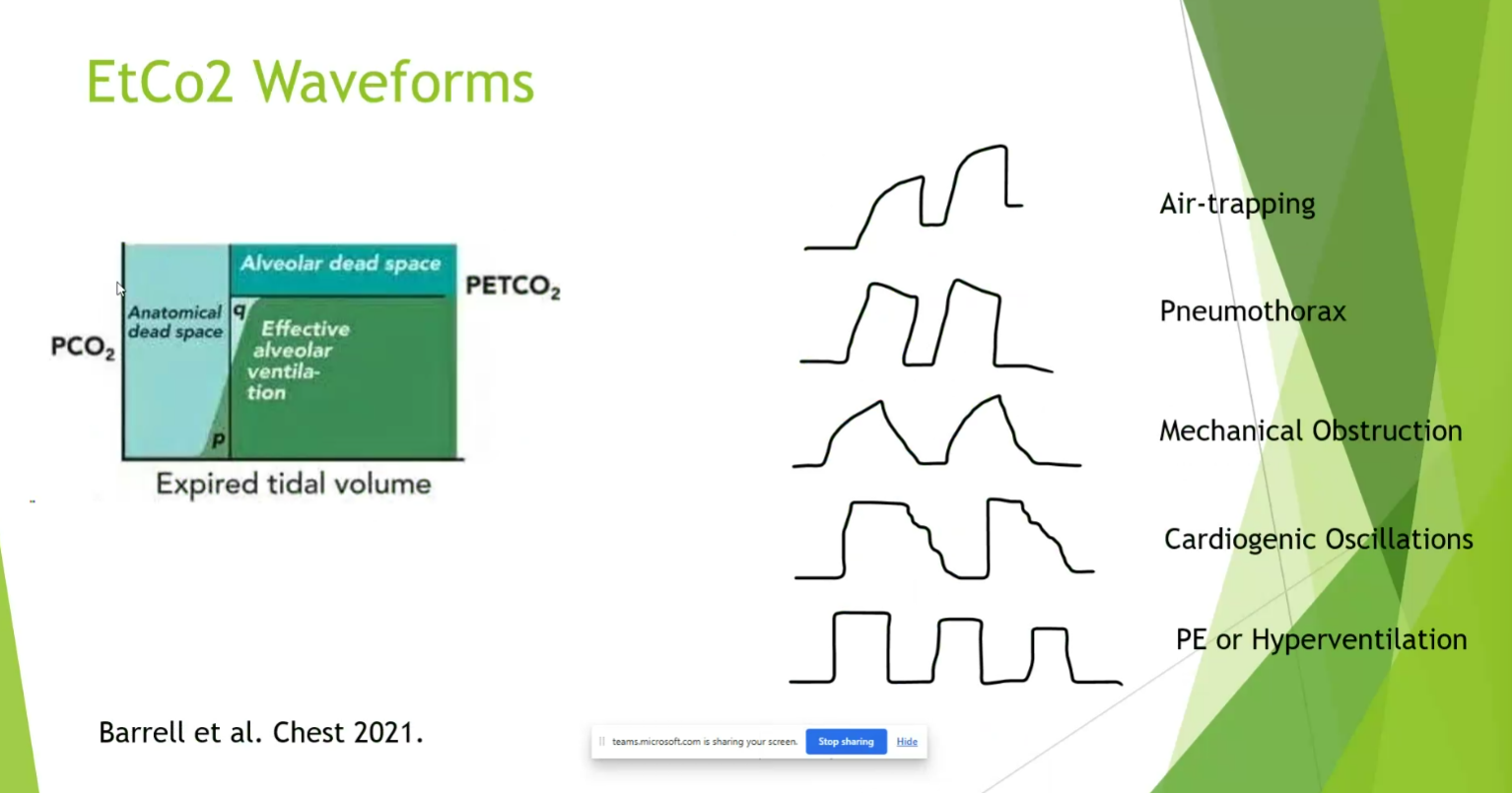
Monitoring

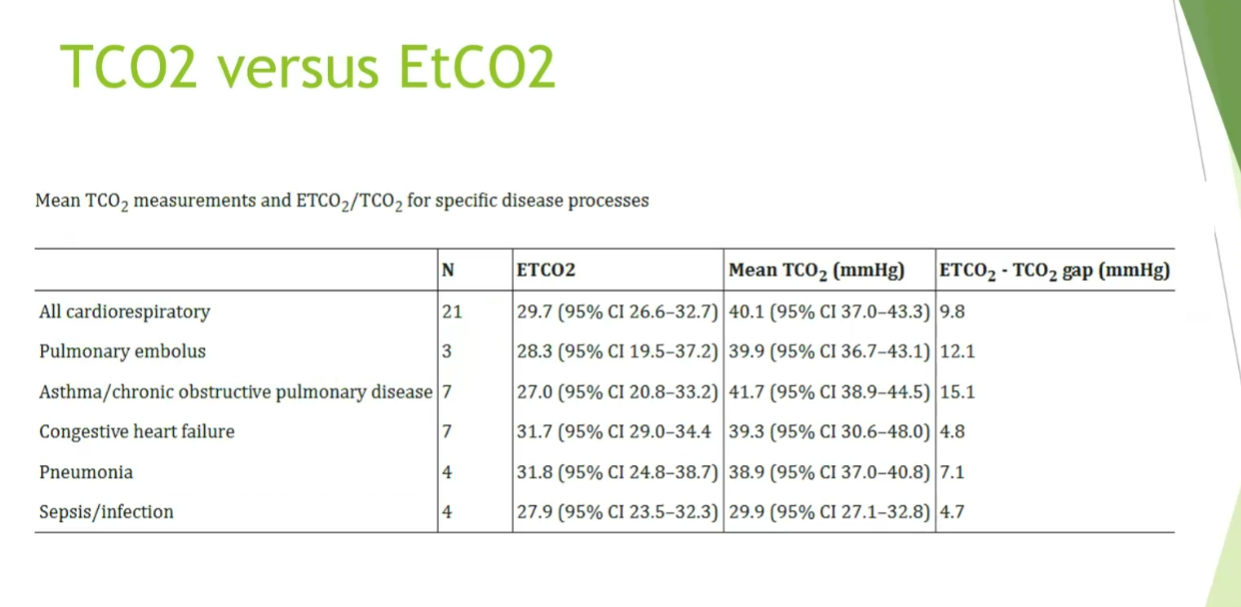
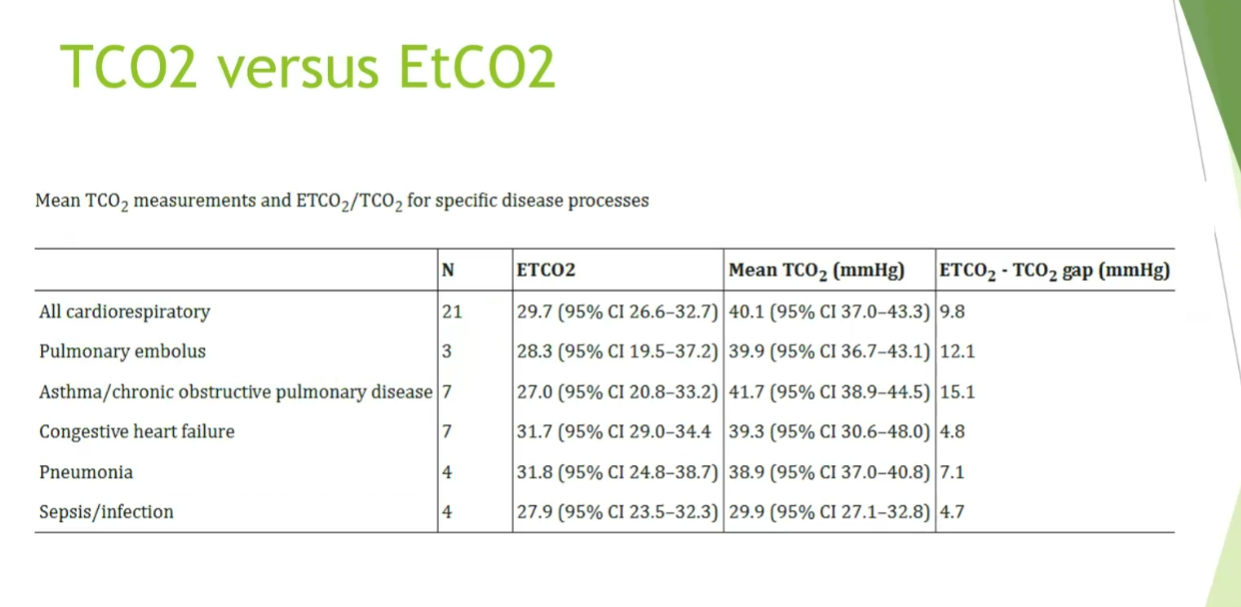
- mean co2 and tCO2 can be quite different between different conditions
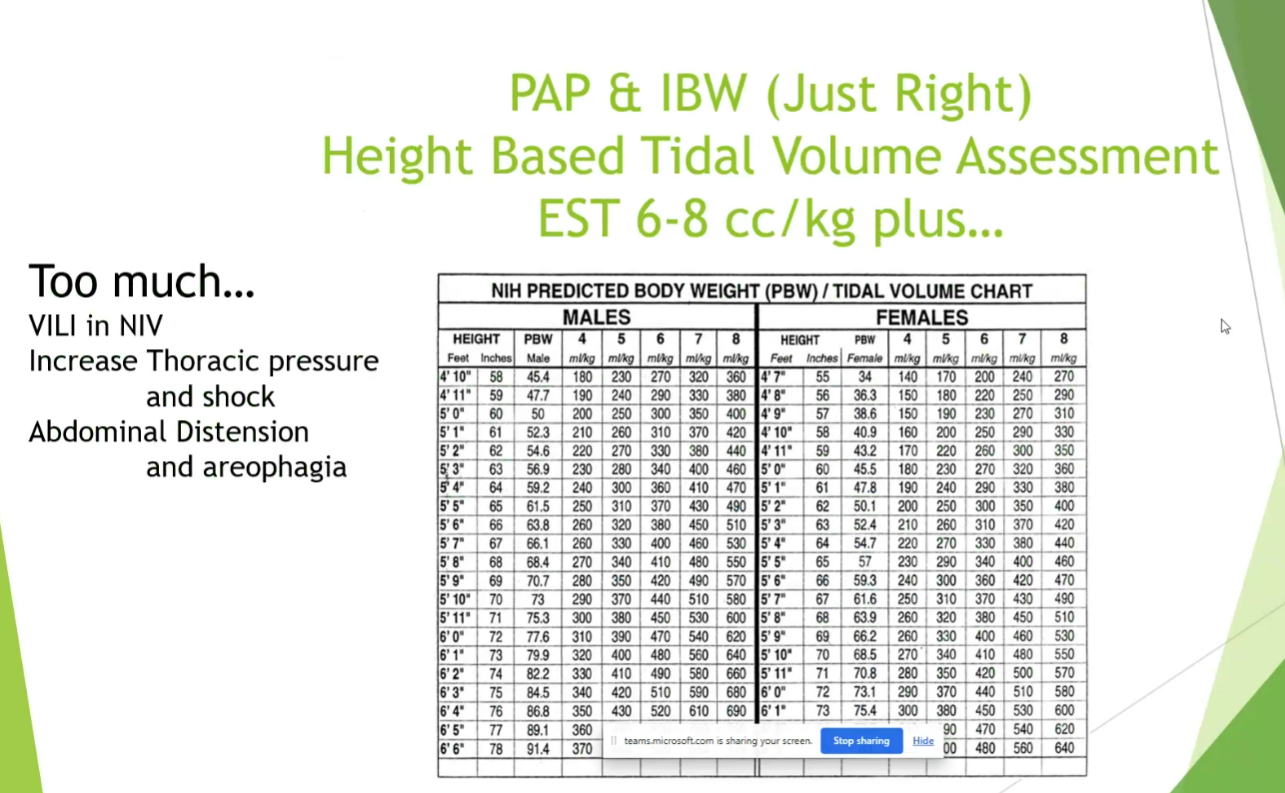
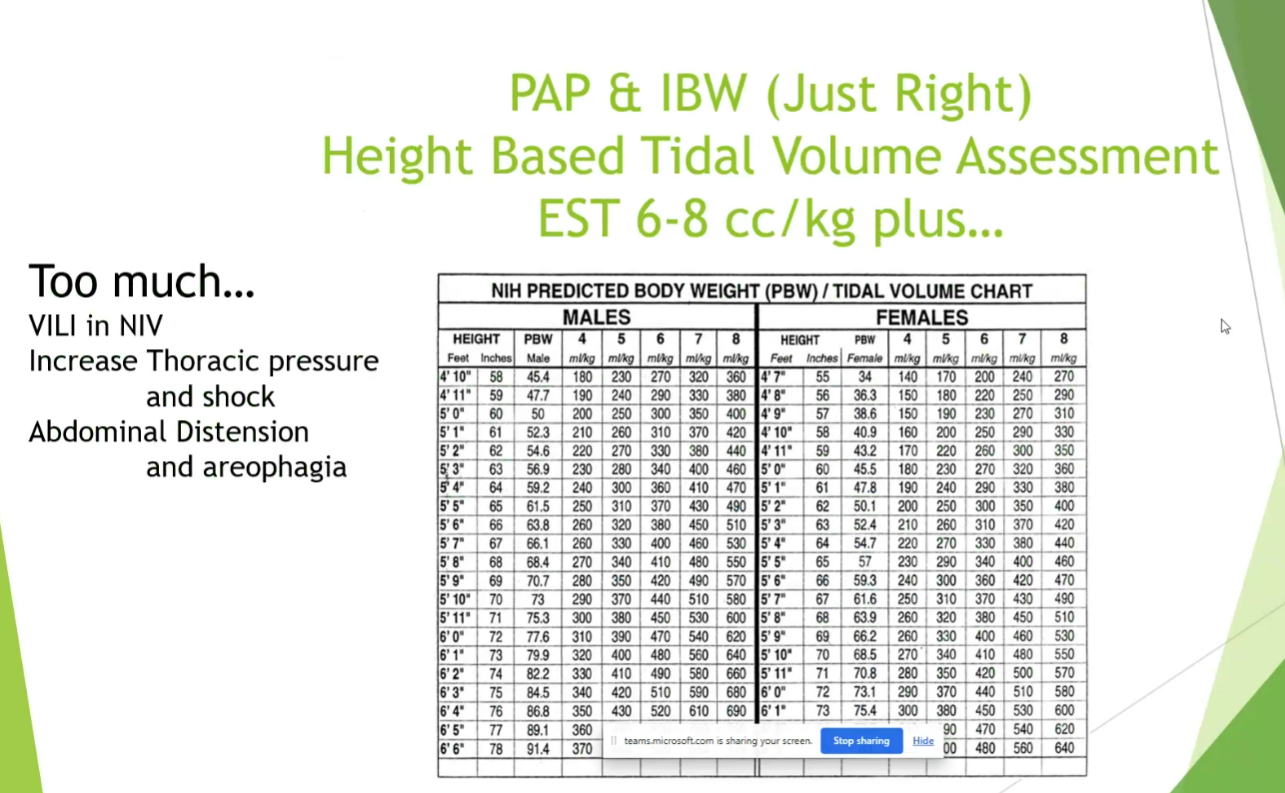
- pressure based on TV
- intestinal obstruction: should probably not do NIV if they don’t have NG in place
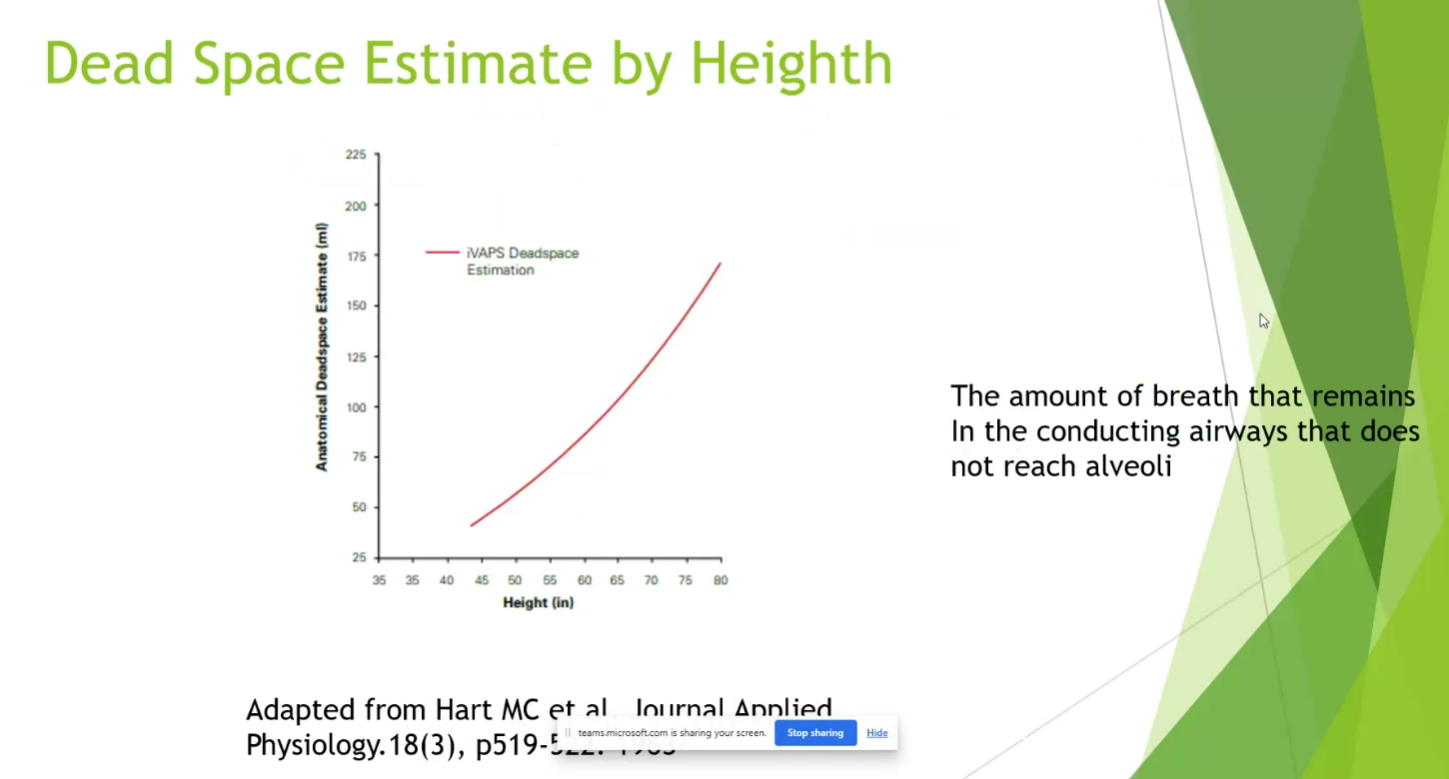
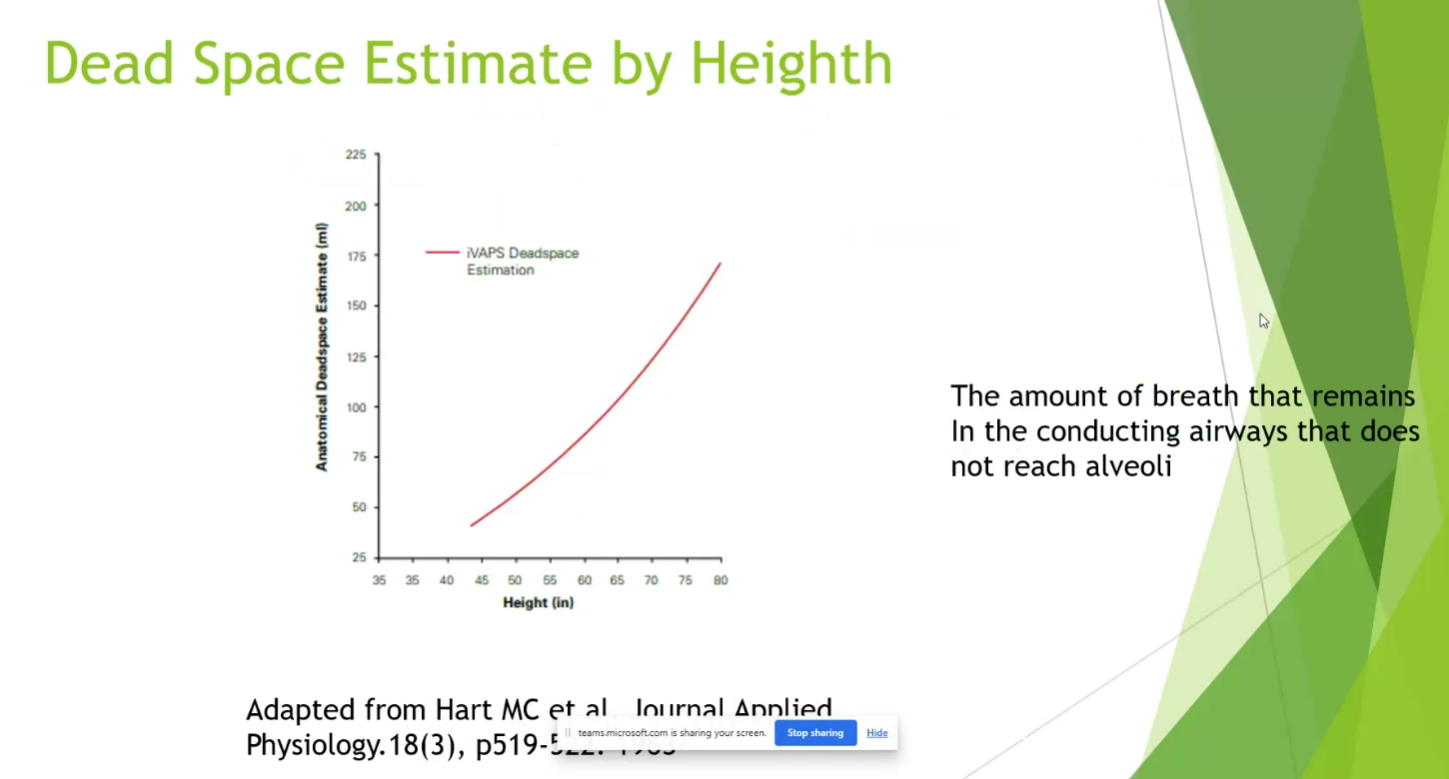
- 6-8 cc/kg + patient’s dead space (around 150cc) should be upper limit target of TV
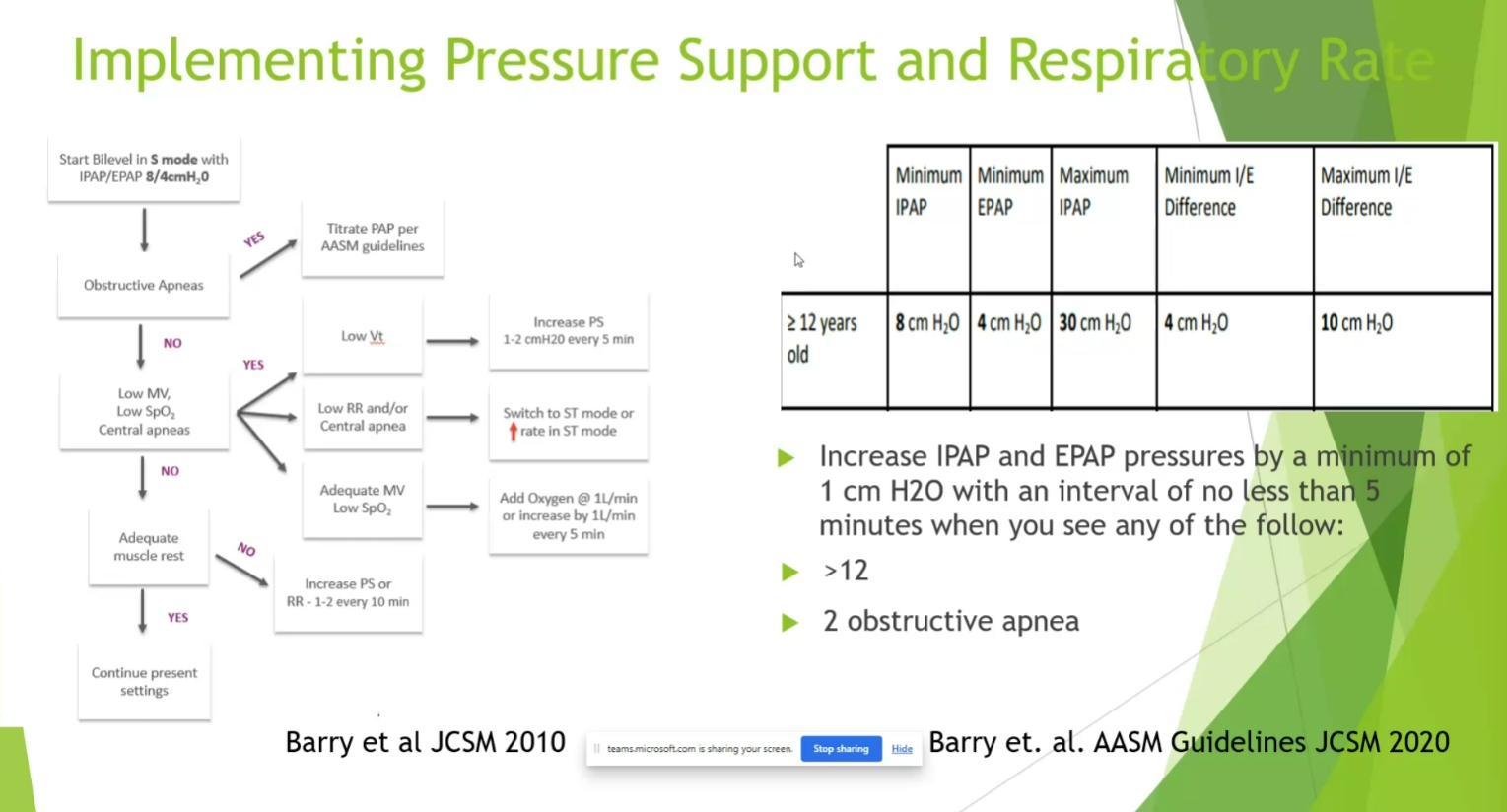
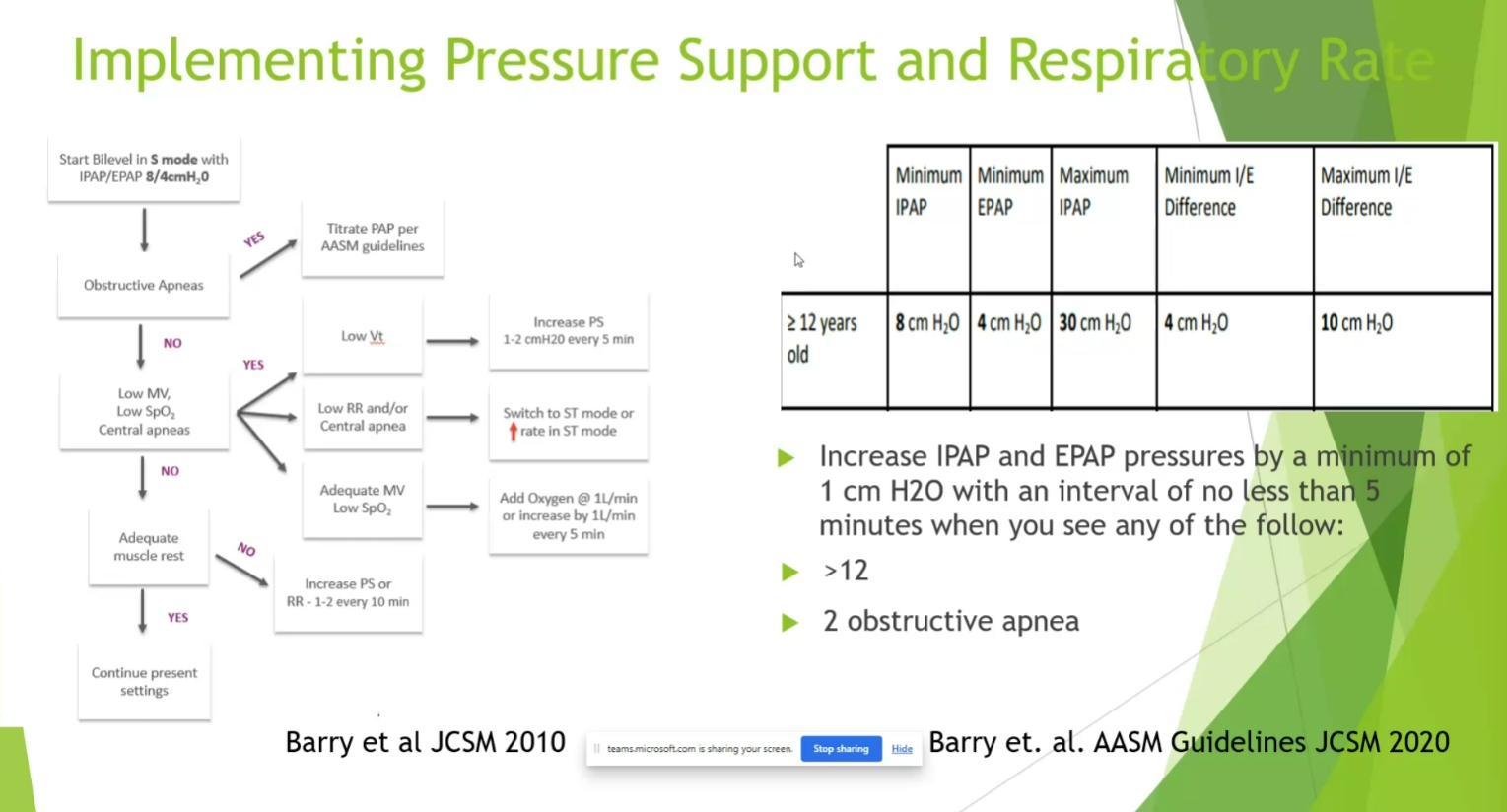
- BMI over 30: start EPAP of 8 or 10 to overcome upper airway obstruction
- look at flow loop to make sure there’s no obstruction on inspiratory flow loop

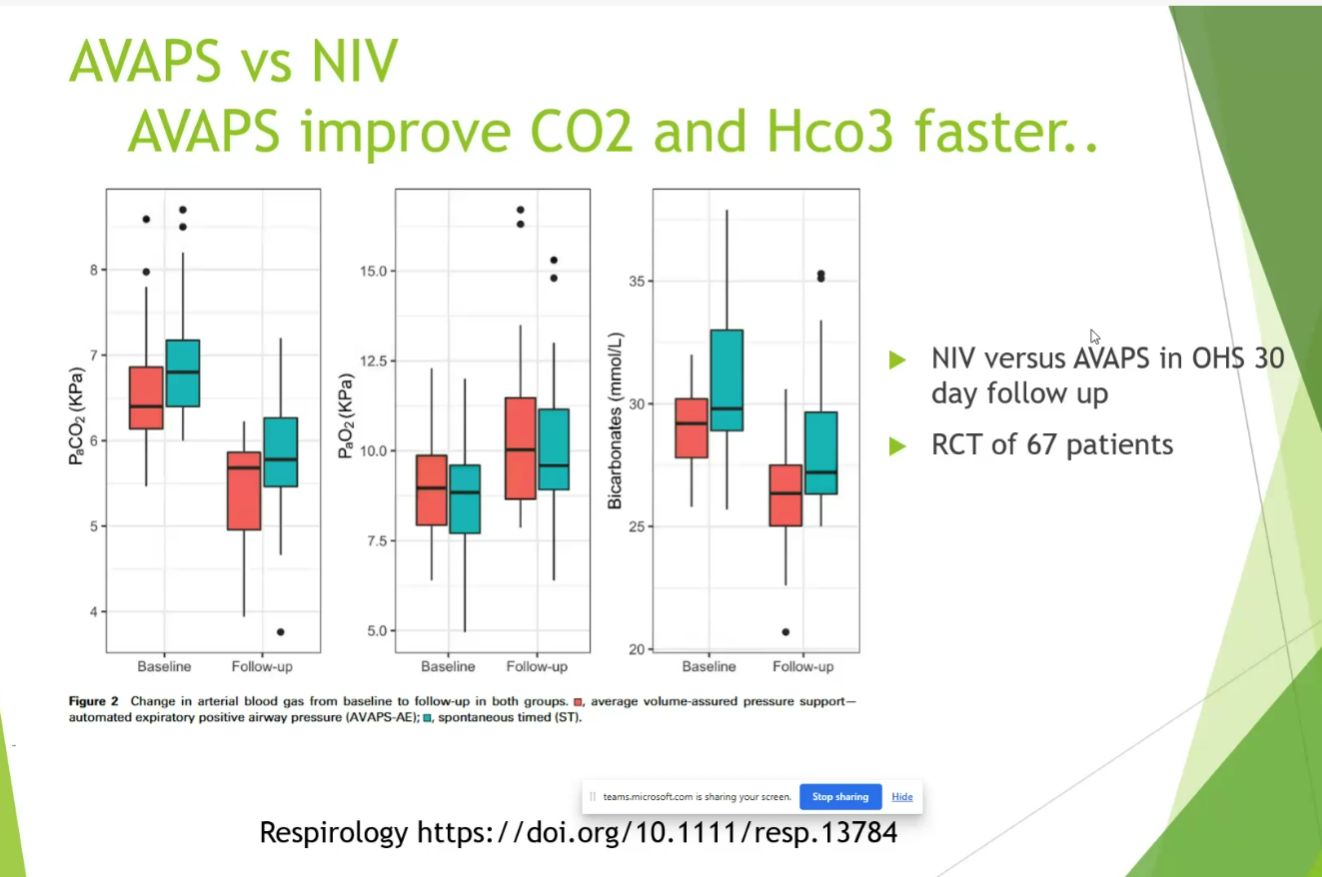
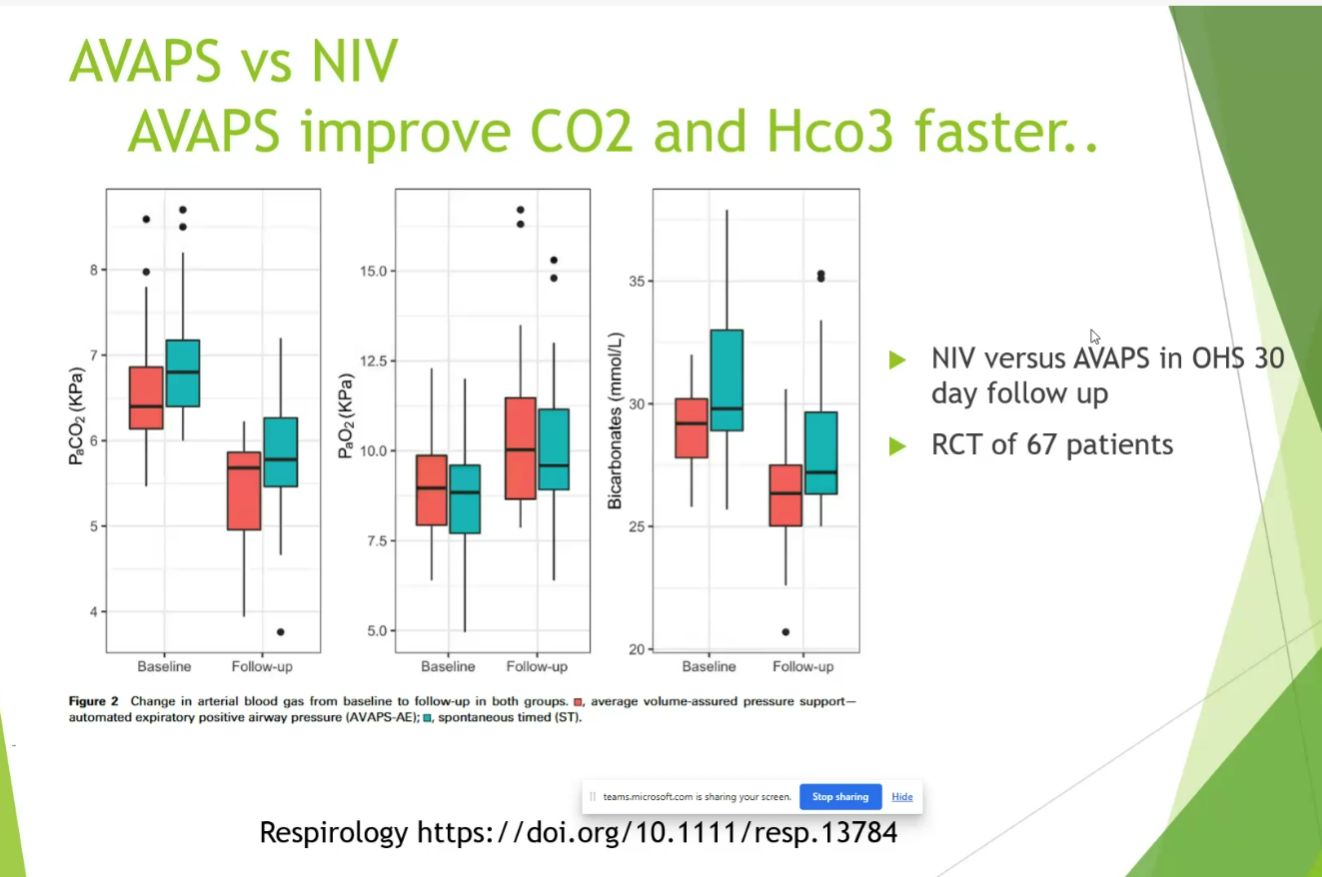
- no dramatic change from NIV with AVAPS
- Drift: lower and lower PS to assure tidal volume with AVAPS. Trilogy/AVAPS bug that can cause recurring admission
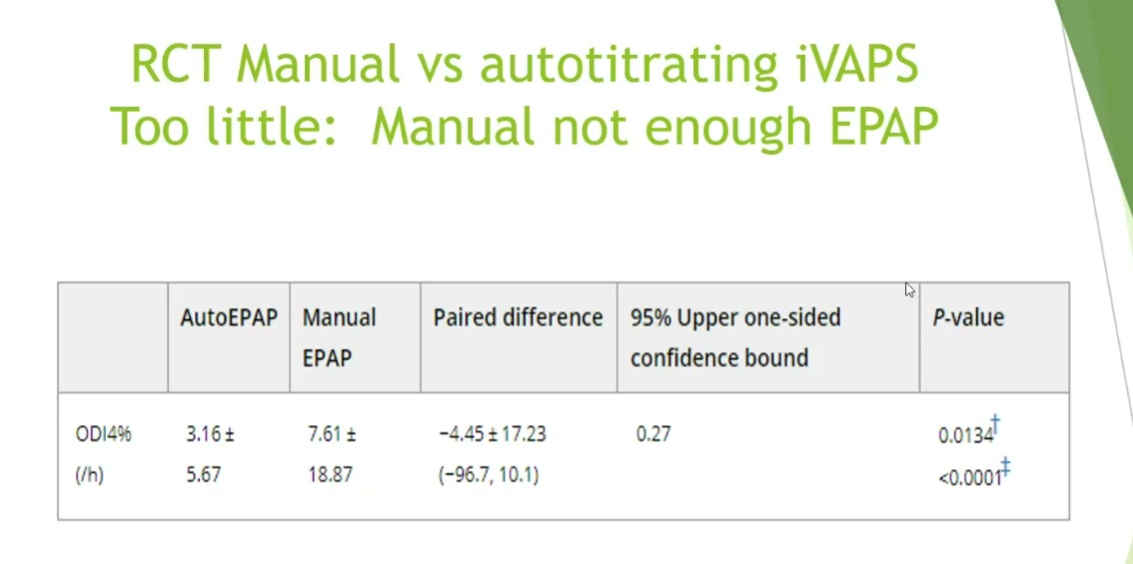
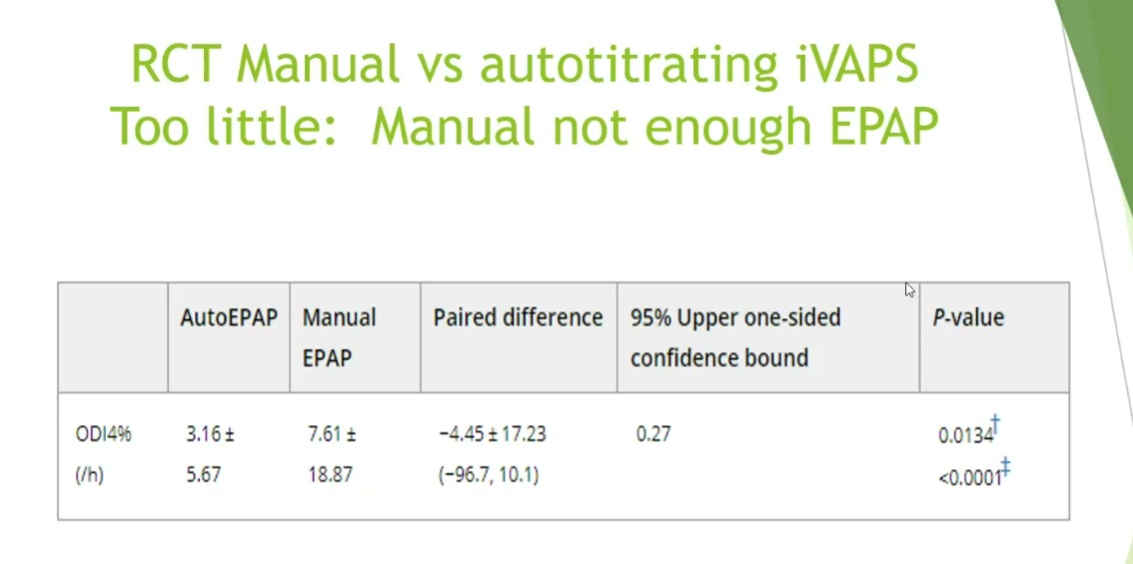
- AVAPS gets patient to PEEP faster than trained technicians at night in NMD, COPD, OHS
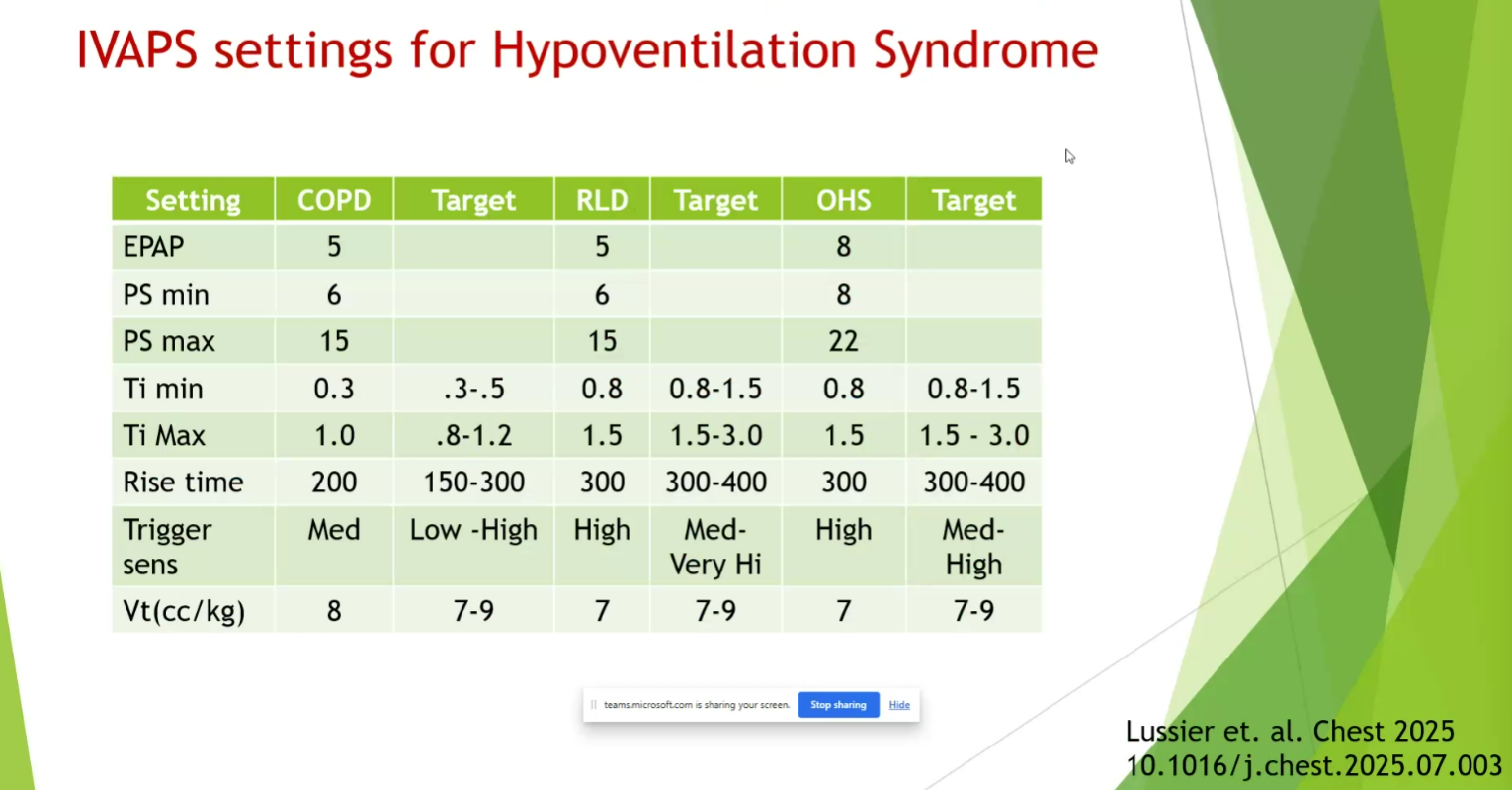
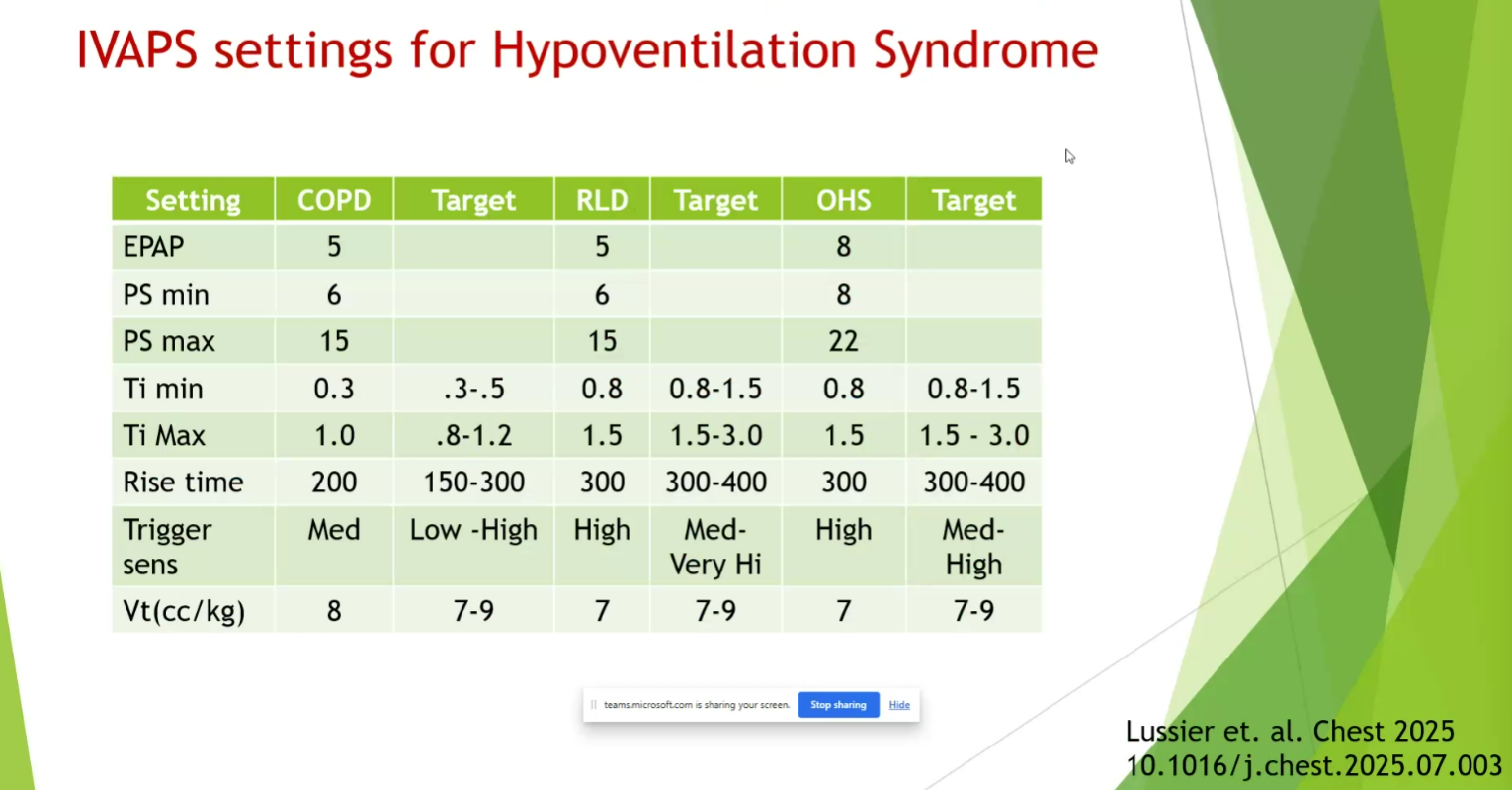
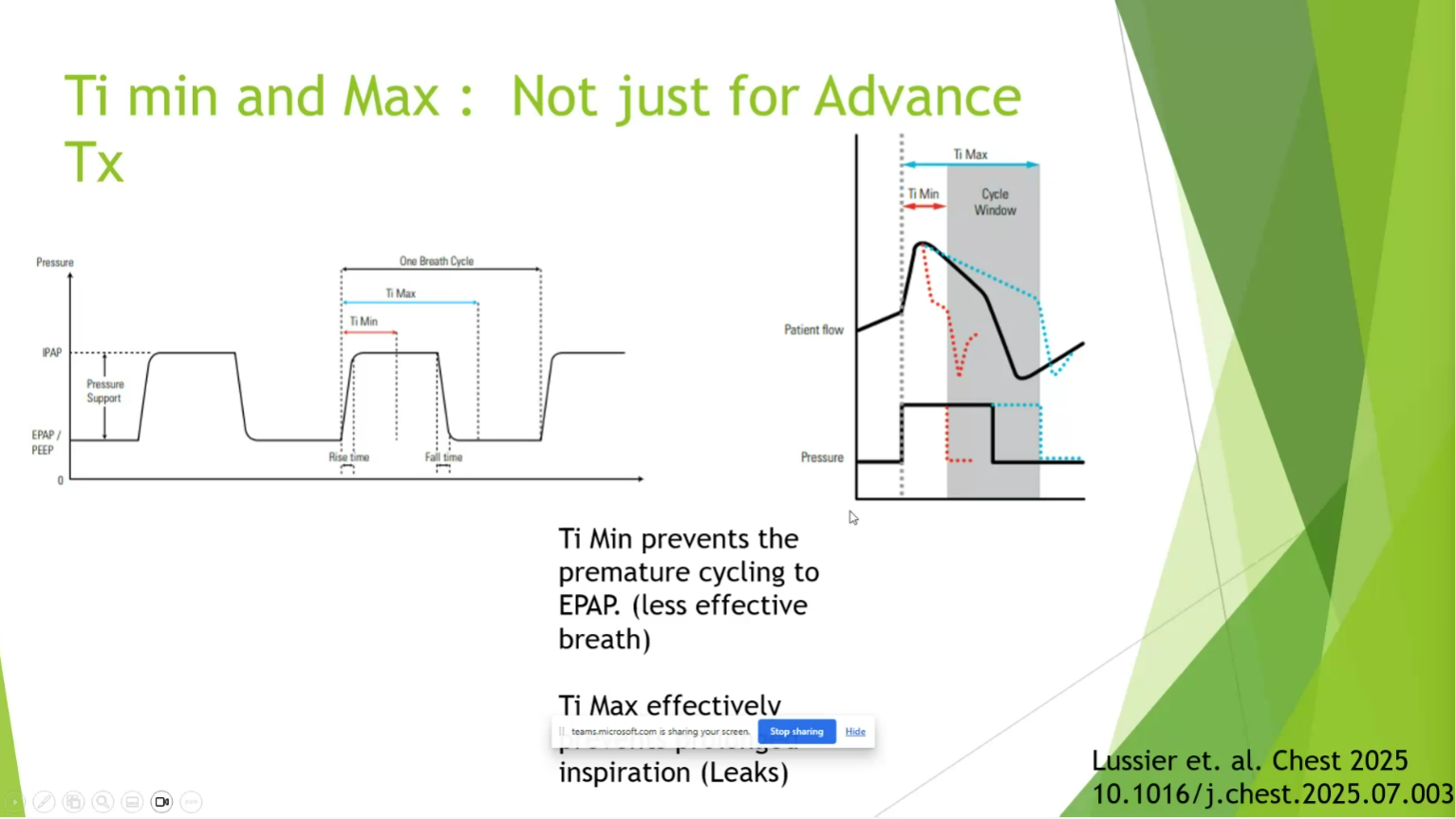
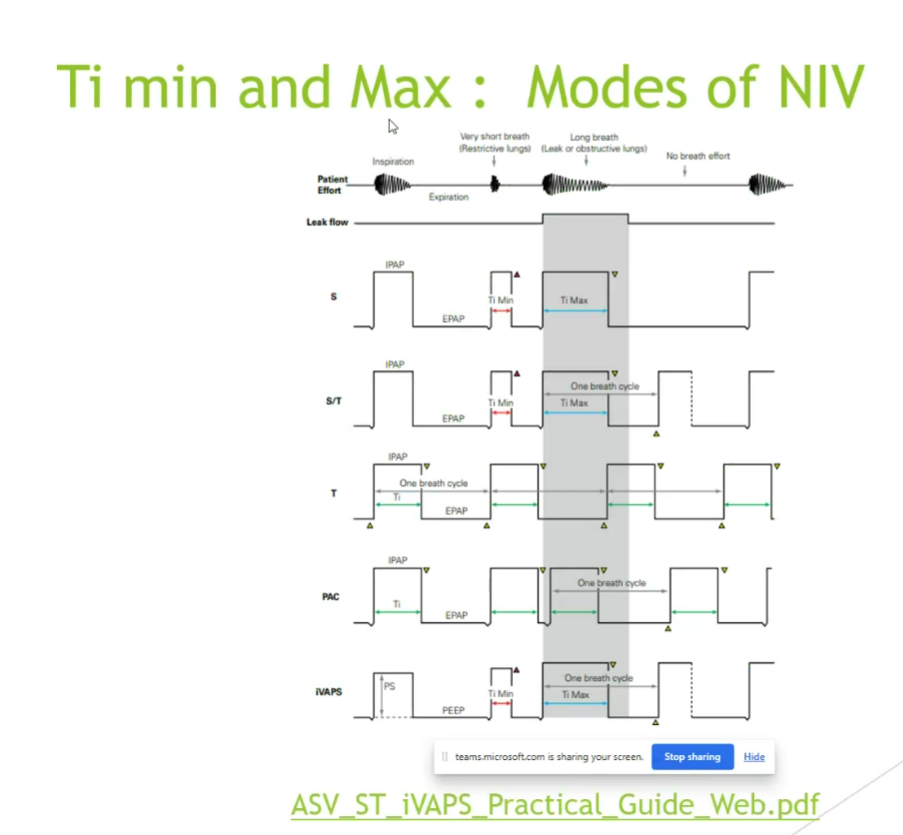
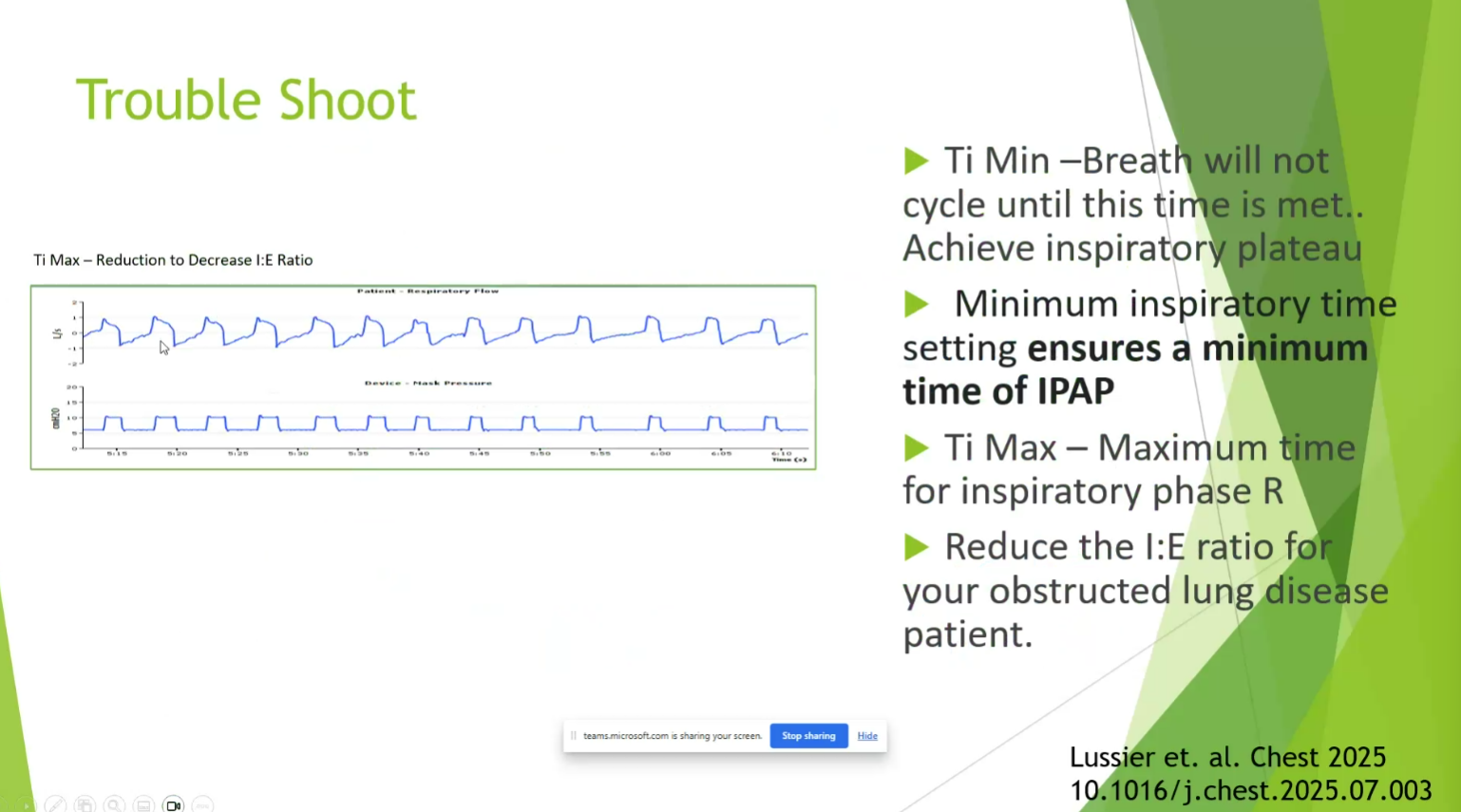
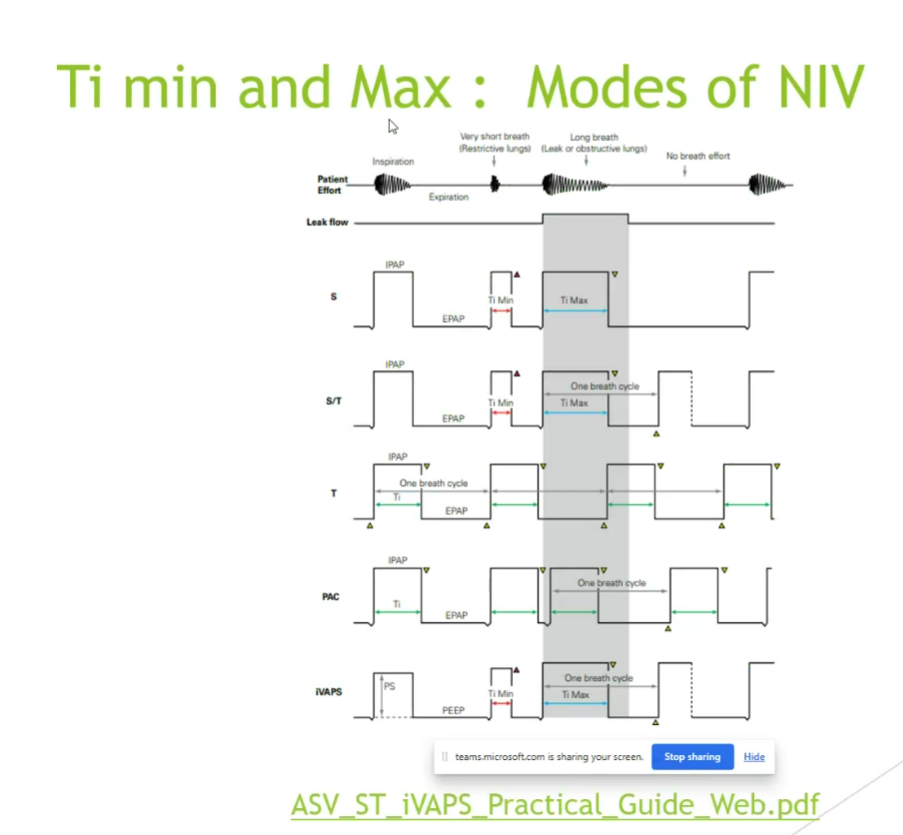
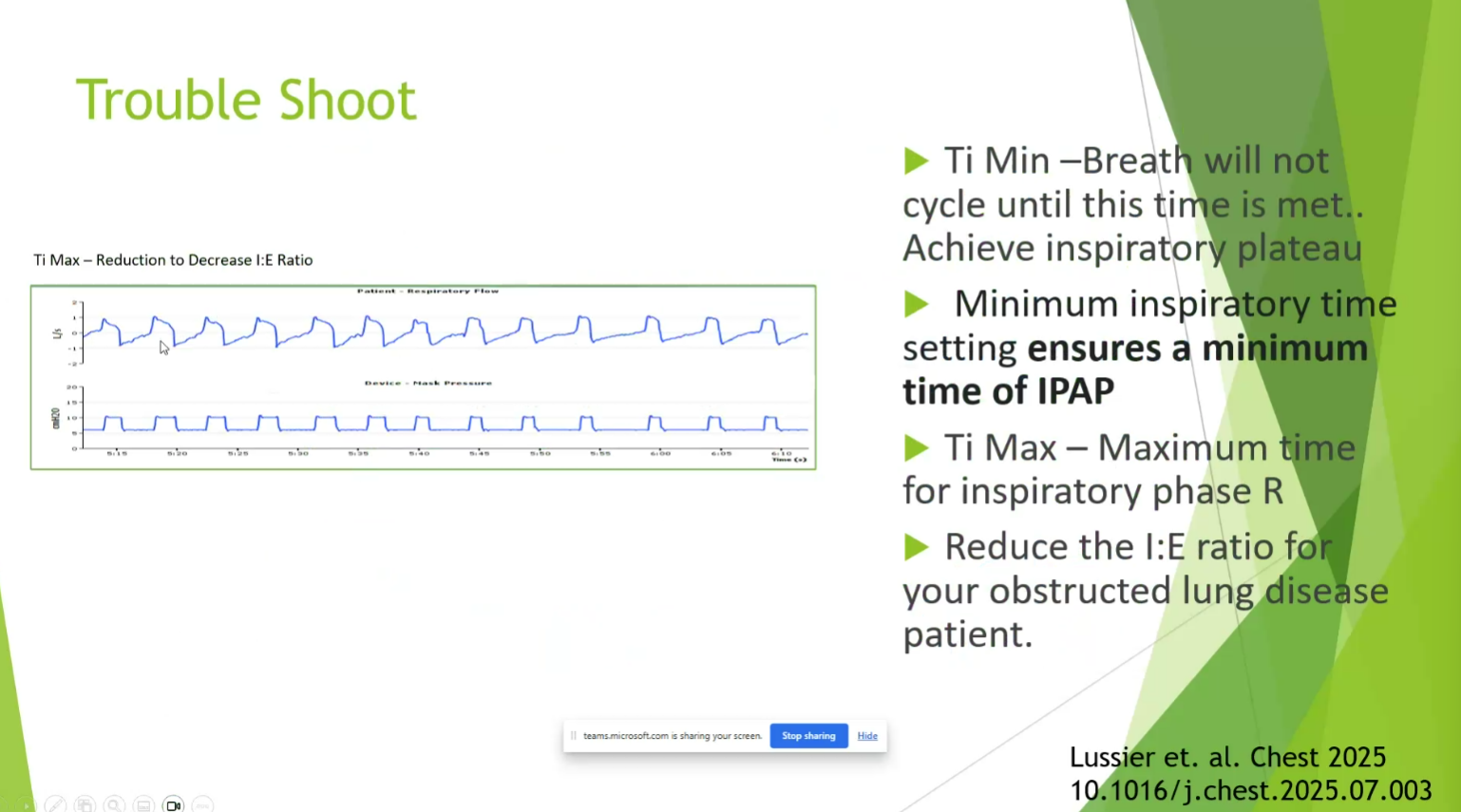
- RLD and OHS: really extend Timin and Timax for diaphragmatic support. Get TiMax to 15
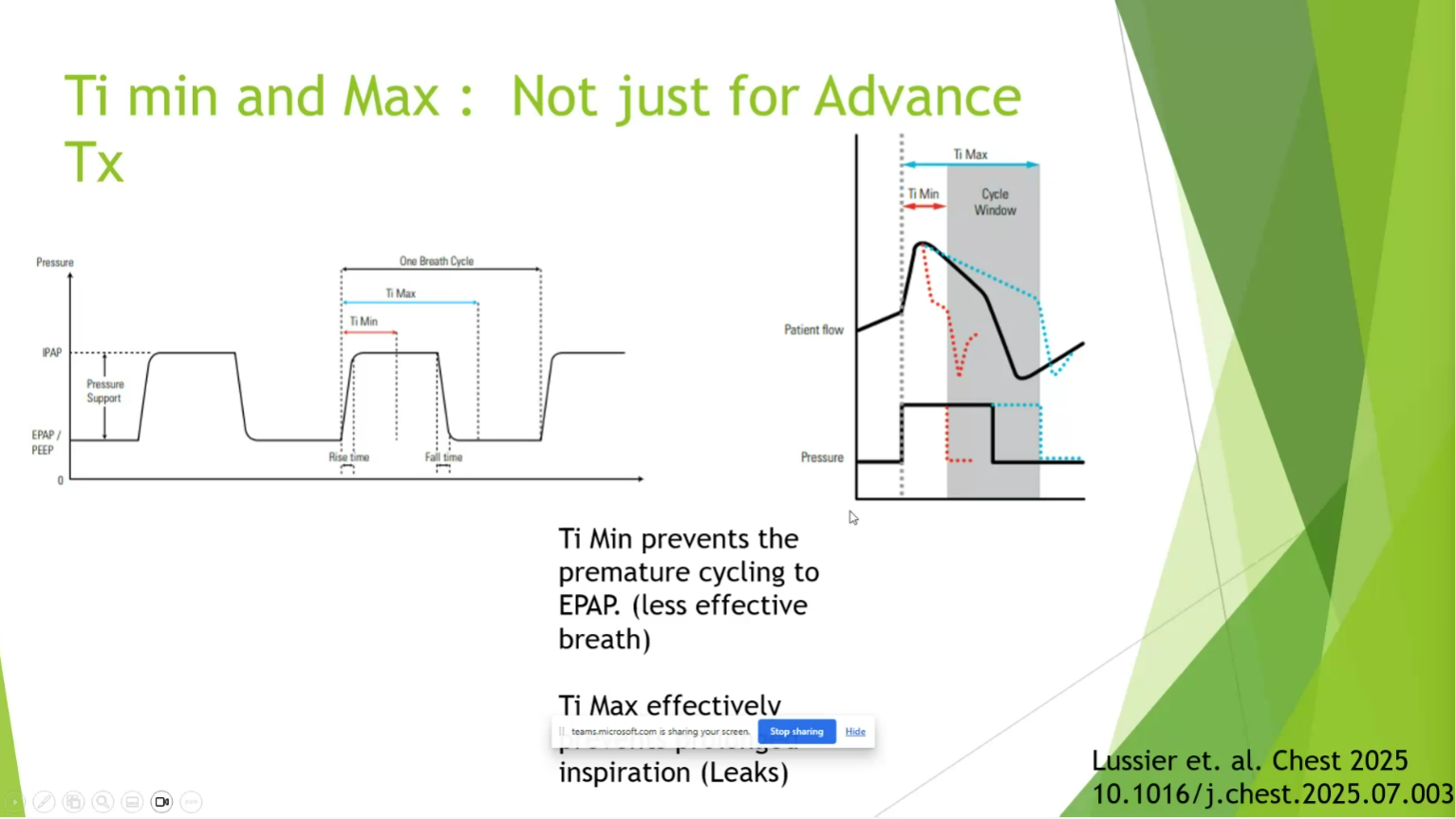
- Ti min prevents premature cycle
- Timax prevents inspiration leaks?
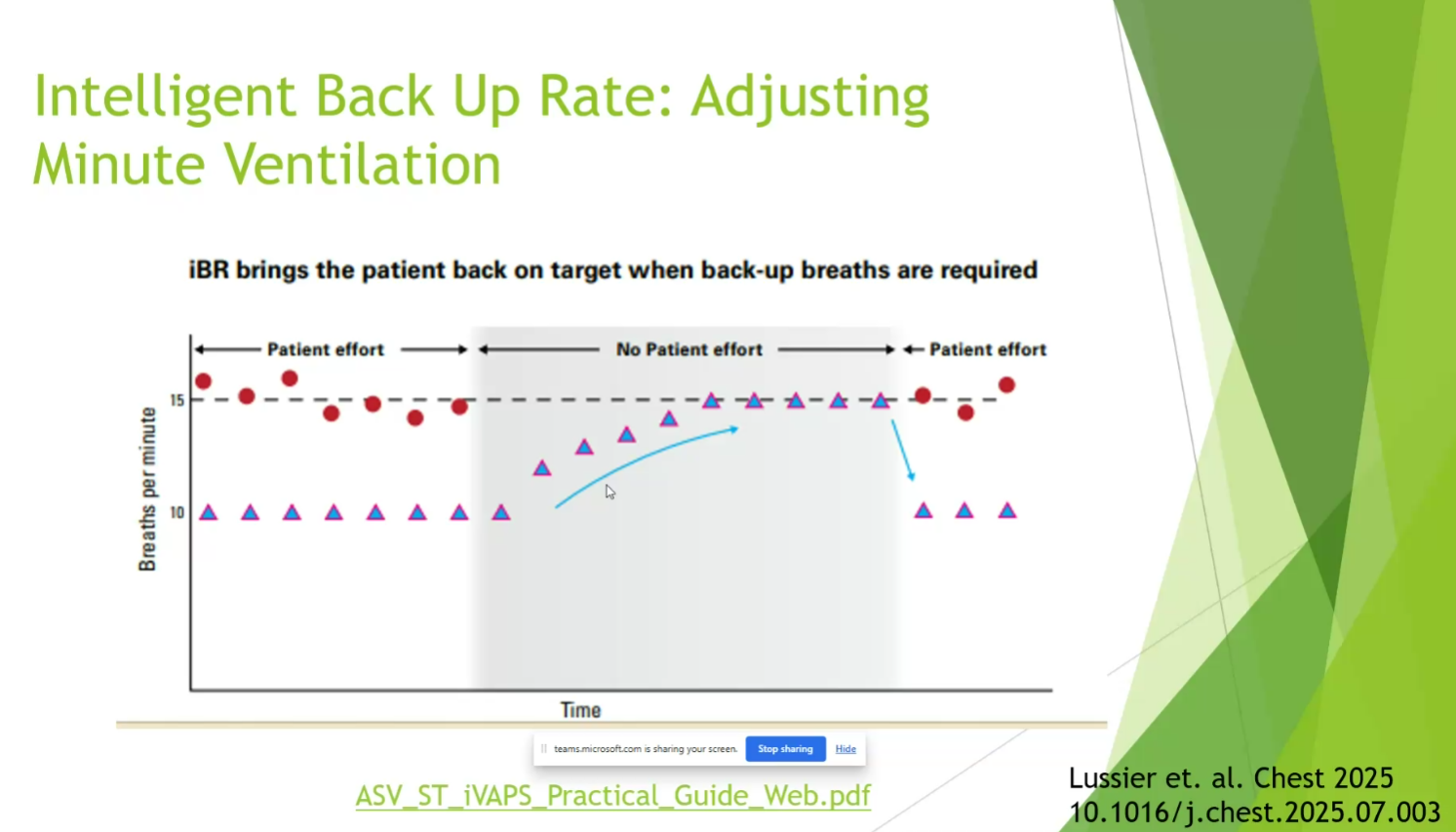
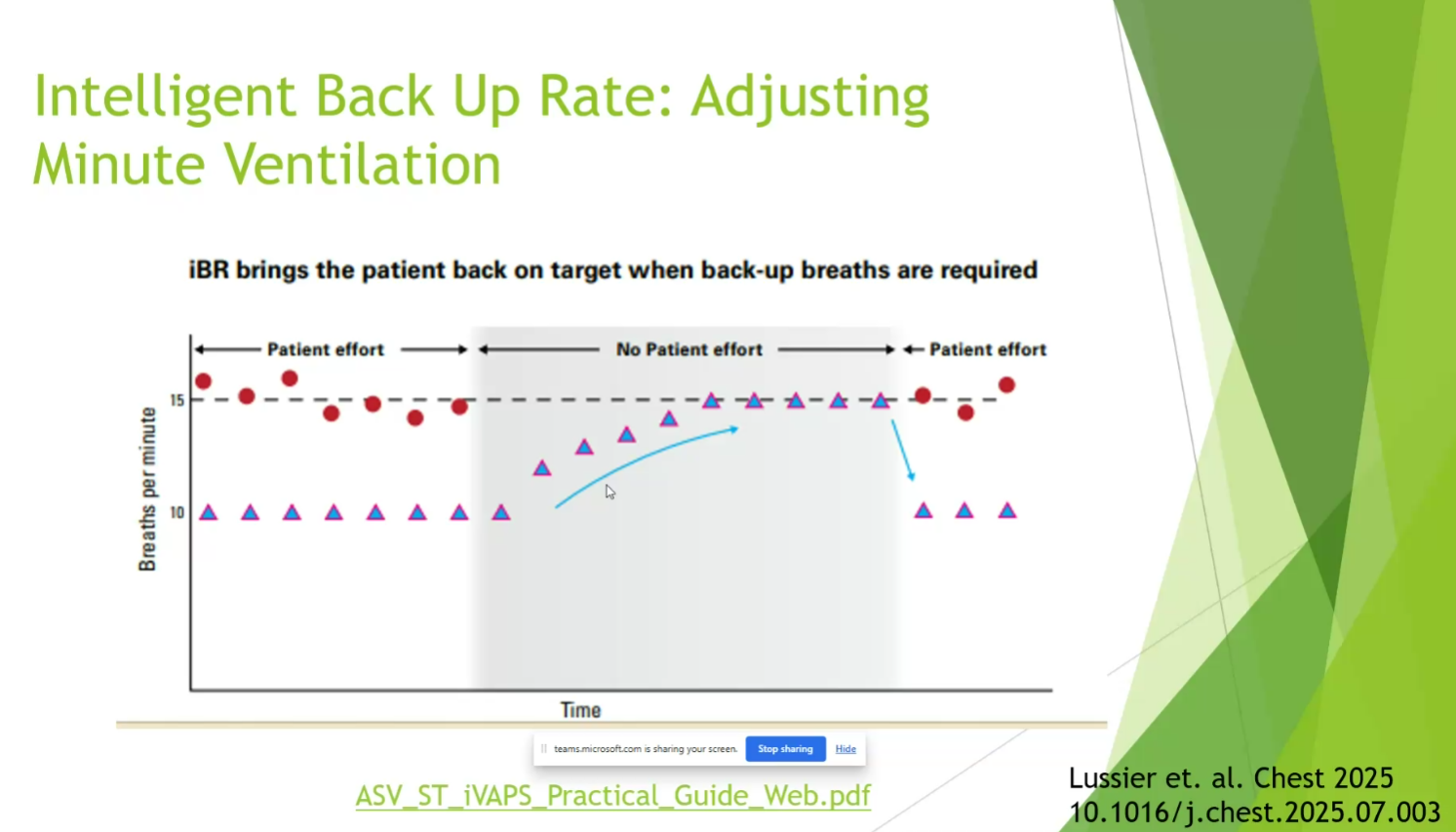
- once pressure target exceeded, respiratory rate then is increased
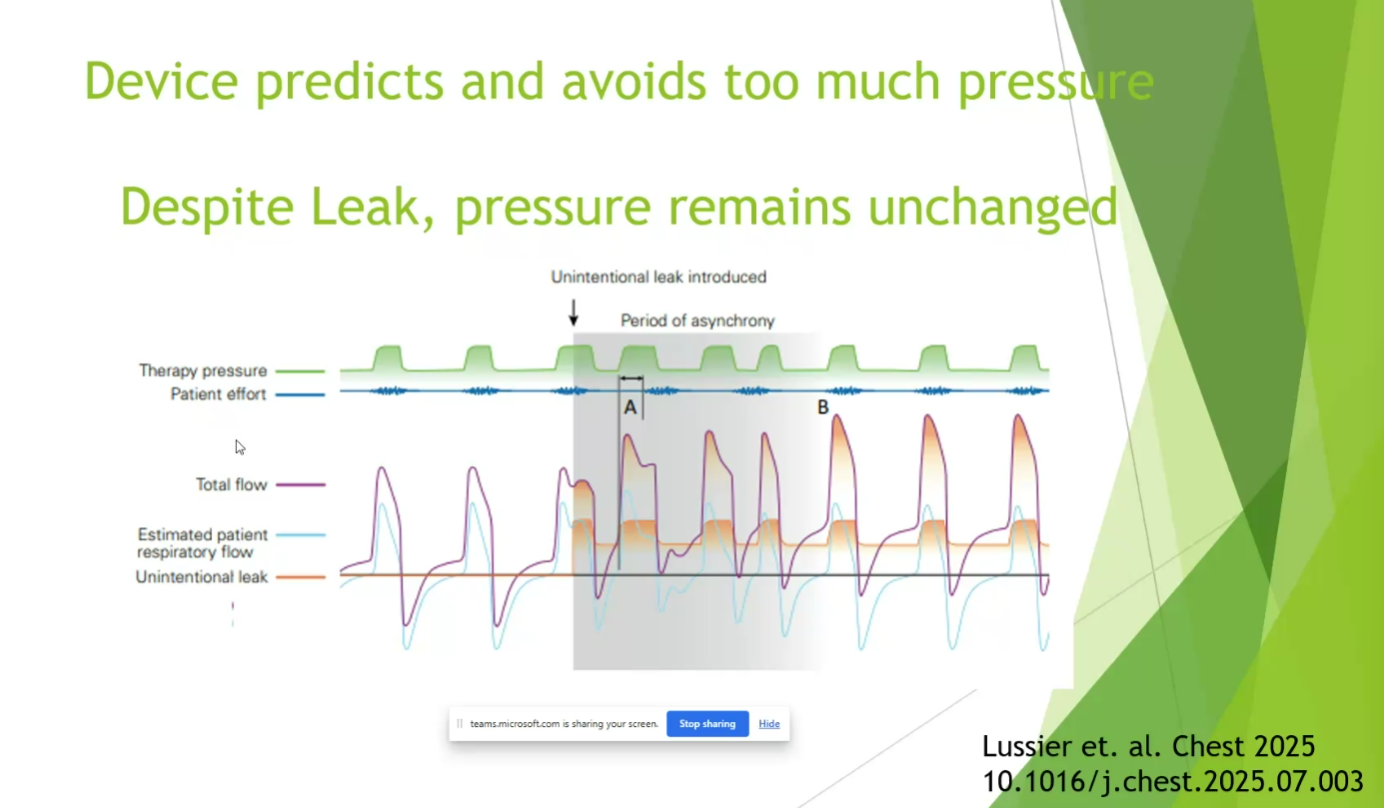
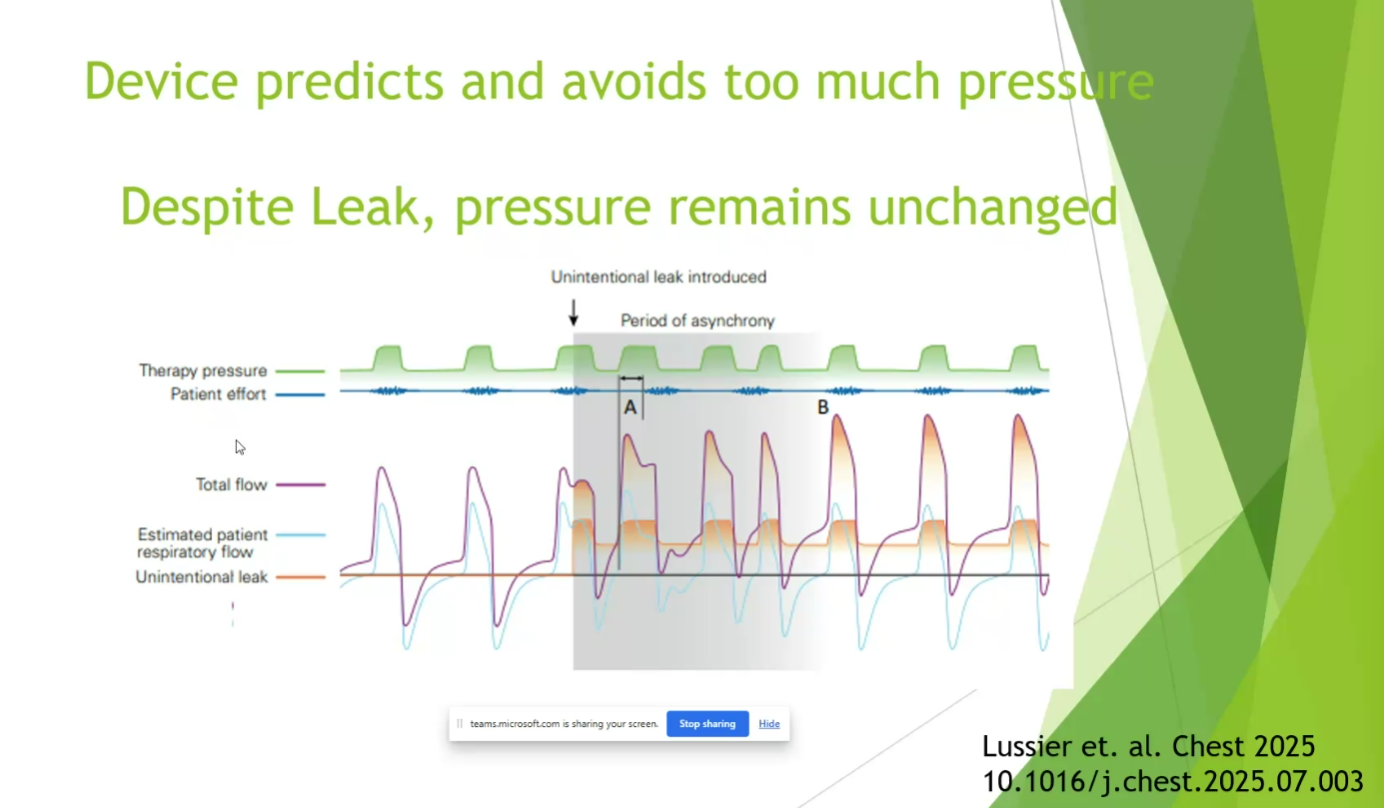
- new technology is better at adjusting pressure to not exceed pressure target with mask leaks
- send pts home with Astral devices, IVAPS
Links to this note