narcolepsy
- related: Psychiatry
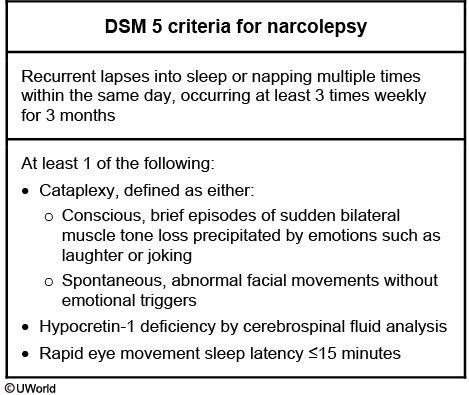
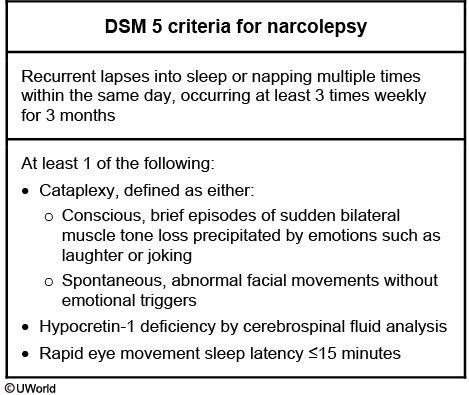
Narcolepsy is characterized by excessive daytime sleepiness leading to "sleep attacks" where patients suddenly fall asleep at inappropriate times. Cataplexy is a unique finding of narcolepsy, where sudden loss of muscle tone is precipitated by emotion or surprise. Sleep paralysis is also indicative of narcolepsy, and is a phenomenon in which patients temporarily feel "frozen" upon waking.
Patients with narcolepsy may experience hypnagogic (just before sleeping) and hypnopompic (occur during awakening) hallucinations.

Narcolepsy is caused by a deficiency in hypocretin (orexin). Hypocretin levels can be immunoassayed with a CSF sample. The pathophysiology of hypocretin neuronal loss is thought to be autoimmune, as 99% of affected individuals have a particular HLA-DQB1 allele.
Hypocretin-secreting neurons are located in the hypothalamus.
Treatments for narcolepsy center around CNS stimulants. The current 1st line therapy is modafinil, a wakefulness-promoting agent with an unknown mechanism of action. Other CNS stimulants to consider include methylphenidate and amphetamines.
The treatment of choice for cataplexy in the setting of narcolepsy is REM sleep-suppressing agents, such as venlafaxine, fluoxetine, atomoxetine. If cataplexy is not controlled with one of these medications, sodium oxybate is the next line of treatment.
- Sx include: fragmented sleep, hypnagogic hallucinations, sudden onset of sleep during day
- Population: teen to late 20s
-
Diagnosed by sleep study/polysomnography
- multiple spontaneous awakenings
- reduced sleep efficiency (total sleep time divided by total recording time)
- reduced latency of rapid eye movement (REM) sleep.
-
Polysomnography can also exclude other causes of EDS (excessive day time sleepiness) (eg, sleep apnea).
-
goal: reduced excessive day time sleepiness
-
modafinil: novel stimulant, less addictive, first line
-
older stimulants: methylphenidate, amphetamines
- effective but addictive
- bad side effects
-
nonpharmacologic:
- taking scheduled naps
- good sleep hygiene
-
sudden onset of muscle weakness
-
triggers: intense emotional episodes (eg, anger, laughing, surprise)
-
occurs in roughly 70% of patients with narcolepsy.
-
Treatment: stimulants, nonpharmacologic
-
can be treated with a serotonin-norepinephrine reuptake inhibitor (eg, venlafaxine) or selective serotonin reuptake inhibitor, and a tricyclic antidepressant can also be considered.
-
Sodium oxybate (the salt form of gamma-hydroxybutyrate) can improve nocturnal sleep, relieve excessive daytime sleepiness and has anti-cataplectic properties; however, it is rarely used due to abuse potential and restrictive regulations.