neonatal disorders
Links to this note
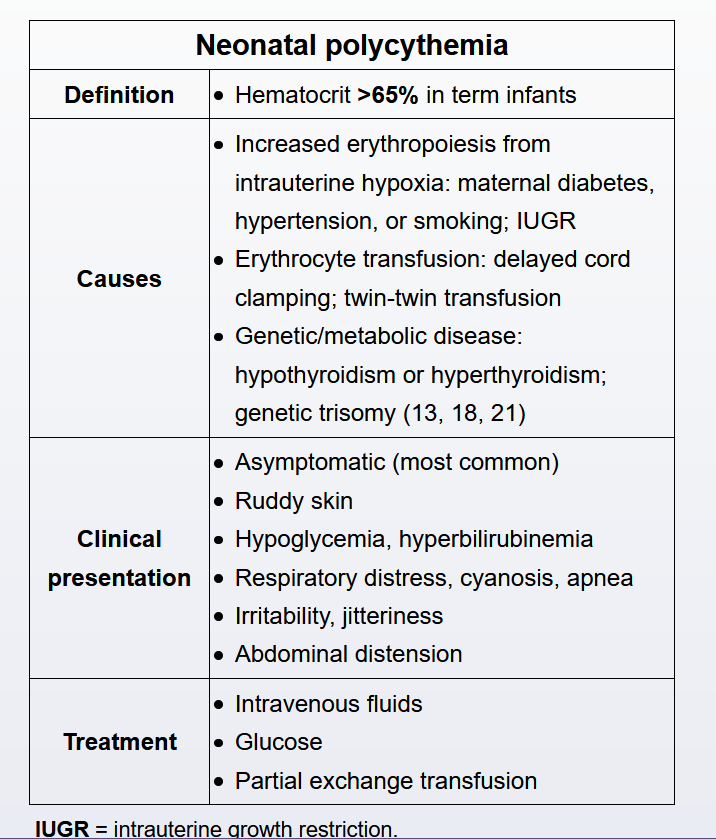
Neonatal polycythemia, which affects up to 5% of newborns, is defined as a hematocrit >65% or hemoglobin >22 g/dL. It is most often observed at 2-3 hours of life as a result of increased hemoglobin production, possibly due to unstable newborn vasomotor factors or in response to relative uterine hypoxia. Factors that contribute to the development of polycythemia include delayed clamping of the umbilical cord, gestational diabetes, maternal hypertension, and intrauterine growth restriction.
In most cases, newborns are asymptomatic and the hematocrit value declines to baseline levels within the first 24 hours of life. However, polycythemia can be associated with complications (eg, hypoglycemia, hyperbilirubinemia, hyperviscosity, hypoperfusion, tissue hypoxia), due mostly to increased red blood cell volume. There may be significant variability in measurements with capillary samples (eg, heel prick). Therefore, if the hematocrit is >65% on a heel prick, it should be confirmed by rechecking a sample from peripheral venous blood, which is more reliable, unaffected by changes in temperature and blood flow, and often up to 15% lower than a hematocrit taken from a capillary sample (Choice D).
Although the majority of newborns with polycythemia are asymptomatic, some affected patients will develop hyperviscosity, which causes complications such as hypoperfusion and tissue hypoxia. This manifests clinically in signs such as plethora, lethargy, irritability, drowsiness, poor feeding, abdominal distension, and hypotonia. Respiratory compromise may occur, resulting in apnea or cyanosis. Metabolic derangements such as hypoglycemia and hyperbilirubinemia are common laboratory abnormalities.
Asymptomatic patients can be observed clinically, as the condition usually resolves within the first 24 hours of life; however, those with clinical symptoms require treatment. Initial treatment consists of hydration and correction of hypoglycemia. If first-line treatment is ineffective, an alternate management strategy is partial exchange transfusion. This procedure consists of withdrawing blood from the infant and infusing normal saline. There are risks associated with this procedure, so it is not the first-line option; however, it improves short-term symptoms of hyperviscosity and is therefore a reasonable next step if more conservative management fails.