neonatal jaundice
Overview

- Prehepatic: mostly unconjugated
- Hemolysis: coombs, G6PD, pyruvate etc.
- Hemorrhage: cephalohematoma
- Neonate: also twin-twin transfusion
- Breast milk, breast feeding
- Posthepatic: mostly conjugated. Usually means gallstones/cancer in adults but not in kids
- Biliary atresia
- Sepsis
- Metabolic derrangements
- Intrahepatic: mixed picture. Genetic diseases
- Criglar Najar: looks like prehepatic
- Gilbert: looks like prehepatic
- Dubin Johnson: looks like post hepatic
- Rotor: looks like posthepatic
- Hepatitis: damage to liver
Bilirubin
D. Bilirubin
Direct bilirubin aka conjugated:
- has charge, water soluble, cannot cross cell membrane
- when excreted in urine: trapped in urine, turn urine dark
- cannot cross BBB: no kernicterus
Indirect Bilirubin
Indirect bilirubin aka unconjugated:
- fat soluble. Not cross glomerulus and not excreted in urine
- Does not turn urine dark
- Can cross BBB: kernicterus
Jaundice
Physiologic jaundice
Physiologic jaundice: overwhelming normal system with rate limiting conjugation. Takes time to develop. By the time for first visit, not yellow anymore
- onset: after 72 hours. Leaves newborn nursery, turn yellow
- resolution: < 1wk. < 2 wk for premature
- bilirubin: unconjugated
- rise: < 5 / day
Pathologic Jaundice
Pathological jaundice: atresia, sepsis, metabolic problems. Something is wrong
- onset: first day
- resolution: won't resolve by self
- bilirubin: conjugated
- rise: > 5 / day
Treatment
Only works for unconjugated bilirubin. For physiologic jaundice, help baby move bilirubin along. Pathologic jaundice requires surgery.
- High bili: convert unconjugated to conjugated via blue box
- Really high bili: exchange transfusion
Work up

Breast Feeding
Links to this note
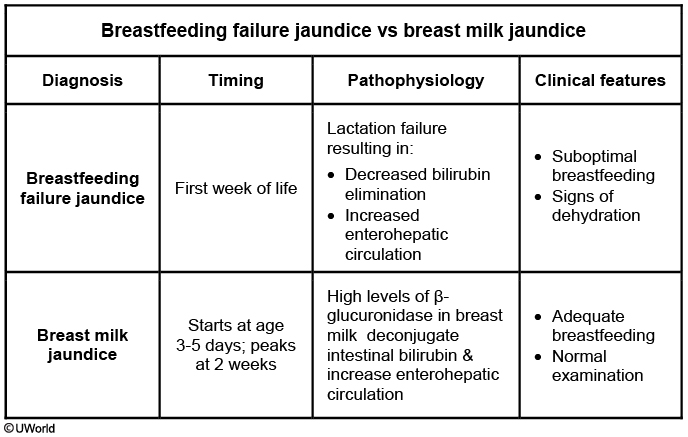
Breast feeding jaundice:
- path: lactation failure (inadequate supply, poor latch, frequent feeding) = bowel function low, bilirubin sits in colon and reabsorbed
- pt: first week of life
- lab: unconjug bili
- treatment: feed more
Breast Milk
Breast milk jaundice:
- path: enzyme in maternal milk inhibits conjugation
- pt: 1-2 weeks of life, unconjug bili
- treatment: continue breast feed
Breastfeeding failure jaundice occurs during the first week of life and is caused by lactation failure from inadequate milk supply, poor latch, or infrequent feeding. This decrease in oral intake results in decreased bilirubin elimination and increased intestinal absorption of bilirubin, thereby increasing serum bilirubin. This infant's age, normal weight, intake/output, and examination make this diagnosis unlikely.
Breast milk jaundice is a common cause of unconjugated hyperbilirubinemia in exclusively breast-fed infants that develops during the first 3-5 days of life and peaks by age 2 weeks. The etiology is thought to be due to high beta-glucuronidase activity in breast milk that deconjugates intestinal bilirubin and allows for increased intestinal absorption and enterohepatic circulation of bilirubin. Neonates are otherwise well-appearing, asymptomatic, and breastfeeding successfully.
The American Academy of Pediatrics recommends that infants with breast milk jaundice continue breastfeeding exclusively. Formula (Choice C) is not required if the mother's breast milk supply is adequate and the neonate is gaining weight and has a normal examination. Cessation of breastfeeding can accelerate the decline in serum bilirubin levels but has no clinical benefits as kernicterus from breast milk jaundice is very rare. Rather, discontinuing breastfeeding prevents the infant from receiving the benefits of breast milk, including maternal antibodies, mother-infant bonding, and immunity. Interrupting breastfeeding with bottles, especially during the first month, can decrease the mother's milk supply and the newborn's ability to latch and suck at the breast. All efforts should be made to promote and support breastfeeding. Parents should be reassured that the prognosis is good with spontaneous resolution by age 3 months.