PCP pneumocystis jirovecii
- related: Infectious Disease
- tags: #literature #pulmonary
Pneumocystis jirovecii pneumonia:
- usually presents as a subacute illness with fever, dyspnea, and dry cough in a patient with a CD4 cell count less than 200/µL who is not receiving prophylaxis.
- Chest radiographs most often show bilateral interstitial infiltrates; cavitation or pleural effusion is unusual and suggests another diagnosis. A normal chest radiograph does not exclude the diagnosis, and chest CT is more sensitive, demonstrating patchy “ground-glass” opacities.
- The most commonly described radiographic appearance in PCP is interstitial infiltrates (unilateral, bilateral, or diffuse), although a normal chest x-ray can be seen. Thin-walled cavitary lesions may be present. Spontaneous pneumothorax develops in approximately 5% of PCP patients. Pneumothorax is thought to develop primarily in the setting of rupture of cystic lesions that may be present in active disease or remaining from an earlier infection.
- Normal lactate dehydrogenase levels and stable exercise oxygen saturation have a high negative predictive value, but elevated lactate dehydrogenase levels and oxygen desaturation with exercise are nonspecific.
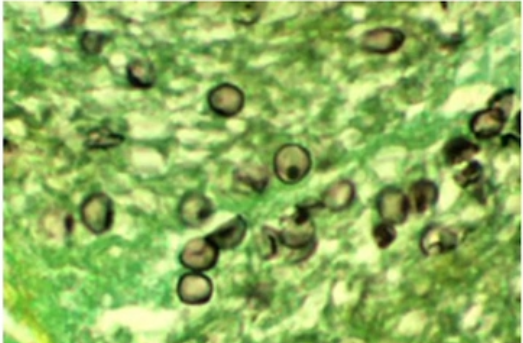
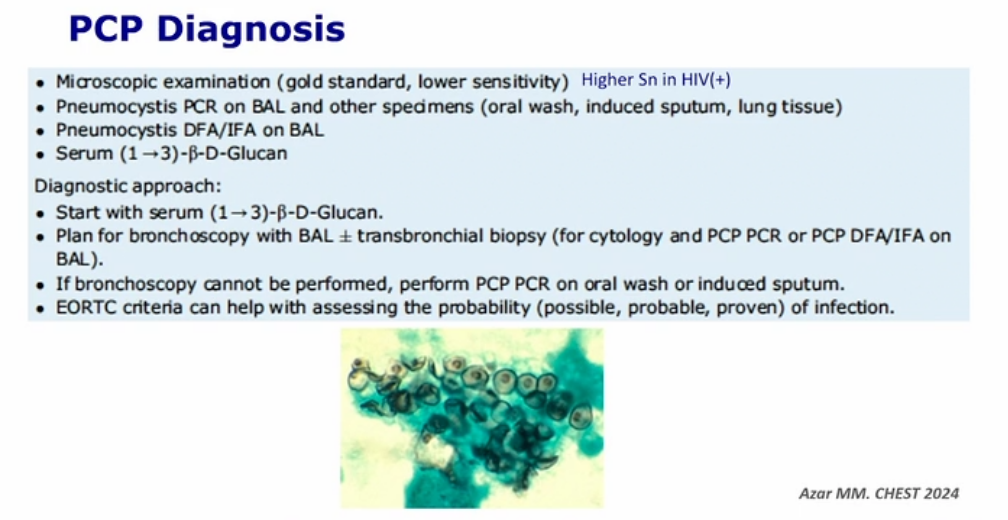
- Diagnosis depends on demonstration of causative organisms and often requires bronchoscopy.
- check for fungitell
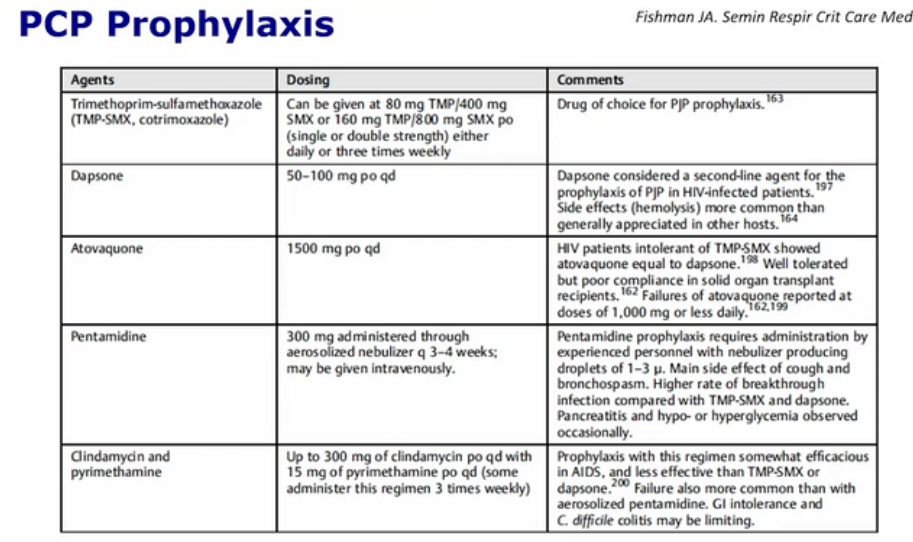
- The treatment of choice is high-dose trimethoprim-sulfamethoxazole; patients who are hypoxic at presentation should be given adjunctive glucocorticoids to prevent the worsening that may accompany initiation of treatment.
PCP Steroids when
Patients with HIV who have moderate or severe Pneumocystis pneumonia (PCP) often have respiratory decompensation during the first 2-3 days of treatment due to organism lysis, which stimulates an inflammatory response. To reduce the risk of intubation and death, corticosteroids are used in those with arterial blood gas (ABG) evidence of alveolar-arterial oxygen gradient >35 mm Hg and/or arterial oxygen tension (PaO2) <70 mm Hg (on room air). Give steroids if patient very hypoxemic.
Some research suggests that pulse oxymetry readings <92% indicate a need for corticosteroids (without ABG). However, ABG remains the standard of care and helps determine whether intravenous antibiotics and hospitalization in the intensive care unit are needed.
Links to this note