Preeclampsia
Normal BP:
- Systolic: 100 - 139
- Diastolic: 60 - 89..
Hemorrhagic stroke is the biggest concern/risk with hypertension..
Chronic Hypertension: HTN (BP ≥ 140/90 mm Hg)..
- Before pregnancy
- Before the 20th week of gestation
- Persists after postpartum period (>12 weeks post-delivery)
Hypertensive urgency and emergency
- Urgency: 220/110; HTN meds and send home
- Emergency: 220/110 and end organ damage; ER admission
Preeclampsia is a hypertensive emergency because of proteinuria, kidney damage..
Gestational Hyptertension
Pregnancy-induced hypertension that:
- Commonly presents after 20 weeks gestation, and can also be seen up to 6 weeks postpartum.
- No pre-existing hypertension
- No proteinuria or end-organ damage. Note: the abrupt onset of hypertension before 20 weeks suggests molar pregnancy..
| Gestational Hypertension | BP > 220/110 |
|---|---|
| Preeclampsia | Gestational HTN + proteinuria |
| Eclampsia | Preeclampsia + seizure |
Preeclampsia
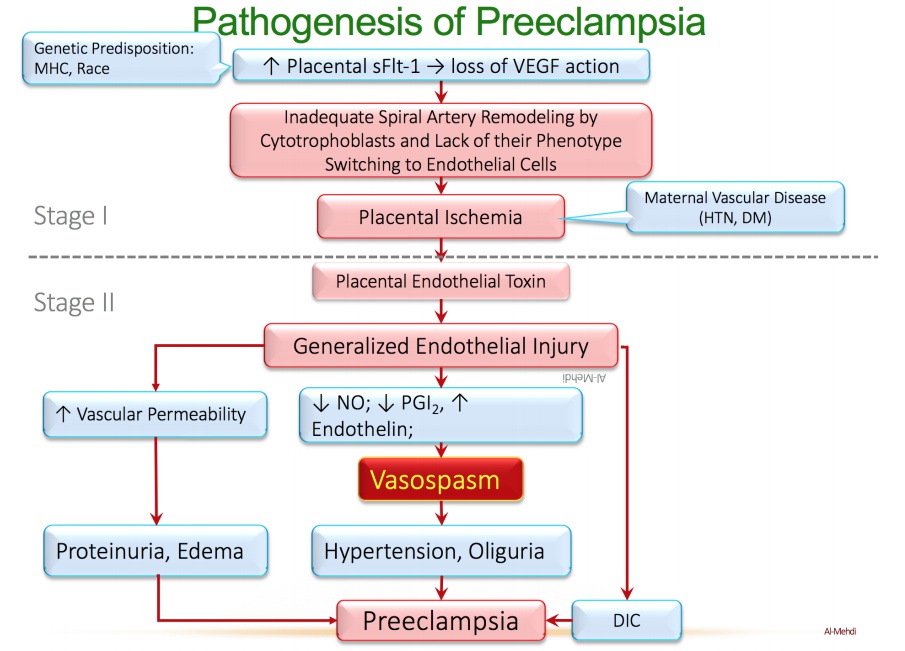
FLT
VEGF receptor in placenta. They become sFLT in soluble form
Genetic predisposes FLT to become sFLT that float around in blood stream and absorb available VEGF. This leads to loss of VEGF action that are needed to transform cytotrophoblast to endothelial cell and remodelling of spiral arteries necessary for placental growth.
This leads to toxin secretion that leads to:
- endothelial leakage resulting in proteinuria and ischemia
- increased vasoconstrictors and decreased vasodilators resulting in vasospasm and hypertension
- placental ischemia resulting in coagulation abnormalities
The clinical presentation includes the following:
- Blurred vision
- Abdominal pain
- Edema of the face and extremities
- Altered mentation
- Hyperreflexia.
There is an increased incidence in patients with:
- Preexisting diabetes mellitus
- Hypertension
- Chronic renal disease
- Autoimmune disorders (lupus)
- First pregnancy
- less than 20 or greater than 35 age.
Preeclampsia Treatment
For chronic, oral therapy of HTN in pregnancy, the recommended drugs are:
- α-Methyldopa
- Labetalol
- Nifedipine..
α-Methyldopa
Acts on α2 (Gi) autoreceptors to inhibit NE release. Has a long history of safety for the mother and the fetus.
Labetalol
α1-blocker in VSMC, causing vasodilation. Different racemic components also act as a non-selective ß-partial agonist with some ß-blocking activity as well.
Nifedipine
L-type calcium channel blocker of the vascular type.
- Stabilize the Mother with anti-HTN medications (labetalol, hydralazine, nifedipine)
- Prevent seizure with MgSO4
- Deliver the placenta.
Although methyldopa is available as a parenteral preparation, acute and accurate control of blood pressure is better with labetalol or hydralazine. However, if nothing else is at hand, it can be used. Drug choice depends on availability and experience with a particular drug by the physician.
Seizure in eclampsia is self limiting. It will go away in 3-5 minutes. You don’t need to treat that; only need to prevent it from happening with MgSO4..
Use urine output as indicator for effectiveness of treatment..
Hydralazine
Works via smooth muscle cell vasodilation:
- Blocks IP3, Ca release
- Releases NO via cGMP.
MgSO4
Antagonizes the activity of calcium. Prevents origination of seizures by reducing activity of iGlut (glutamatergic, NMDA, calcium ionotropic neurotransmission). Mg also reduces vasospasm and reverses oliguria and edema by antagonizing calcium (takes up to 2 days). However, its effect on blood pressure levels is slow via volume reduction and relief of vasospasm. That is why you need the anti-HTN drugs to quickly reduce threat of stroke from high BP.
Overdose of Mg reduces excitability of CNS, resulting in loss of patellar reflex, respiratory and cardiac arrest. First symptom is decreased capillary reflex. In overdose,MgSO4 may produce nephrotoxicity of its own because of its renal clearance. In overdose, treat with calcium gluconate IV injection. Do not use antiepileptic medications for seizure control. MgSO4 is sufficient for seizure control and prophylaxis..
Less than 28 weeks
No fetal viability
- Stabilize mother and give dexamethasone to delay pregnancy
- If mother cannot be stabilized, deliver baby.
28 to 34 weeks
- If life of mother is threatened, deliver the baby.
- Try to maintain pregnancy to at least 34 weeks, when dexamethasone is no longer needed
37 to 41 weeks
Official full term baby.
More than 41 weeks
Post term at 41 weeks. Induce labor via:
- Oxytocin drip: uterine contraction
- Dinoprostone: PGE2, cervical dilation
HELLP Syndrome
Stands for Hemolysis, Elevated Liver enzymes, Low Platelets..
A very serious complication of pregnancy-induced hypertension. It usually only occurs with severe preeclampsia. Can lead to hepatic subcapsular hematomas, which can rupture and result in severe hypotension.
- Laboratory findings show thrombocytopenia and hyperuricemia
- Peripheral blood smear shows schistocytes
- Treatment: immediate delivery
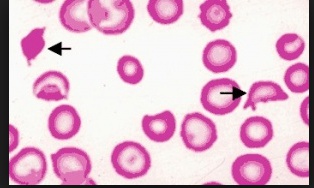
Pathogenesis
Platelet thrombosis in liver shears RBC, leading to hemolysis and low platelet counts. Resulting liver infarct from low O2 leads to increased liver enzymes.