prostatitis
- related: Infectious Disease ID
- tags: #note
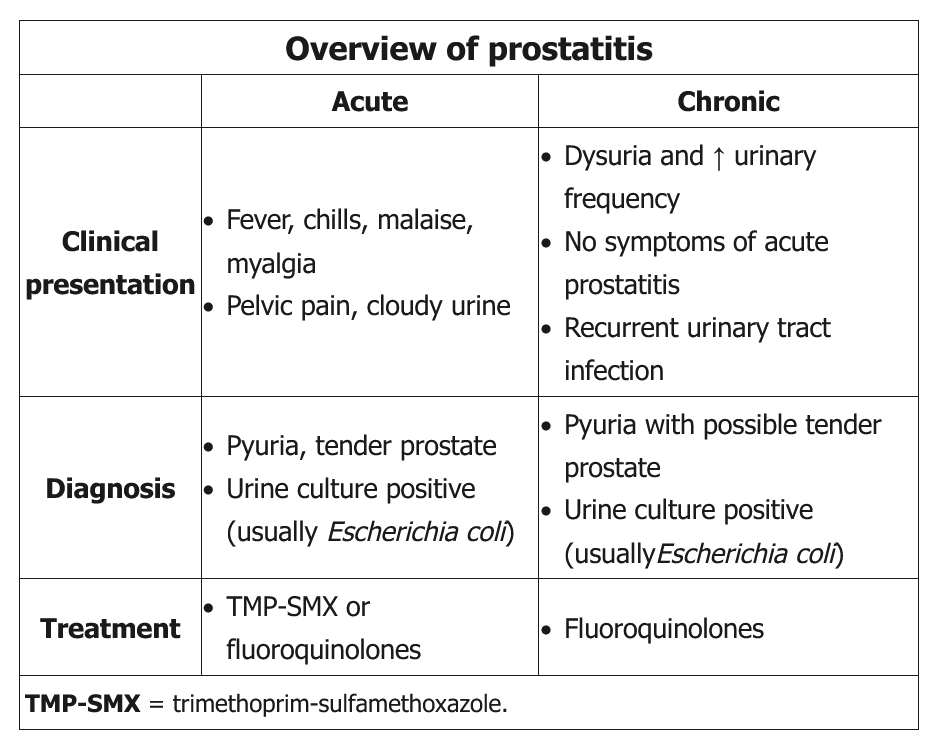
This patient’s presentation is most consistent with acute bacterial prostatitis (ABP). Most cases are due to Gram-negative (eg, Escherichia coli, Proteus mirabilis, Klebsiella, Enterobacter) organisms. Gram-positive (eg, Staphylococcus aureus, Streptococci, Enterococci) infections are less common and are usually due to remote infection elsewhere, prolonged catheterization, or recent prostatic surgery.
Patients typically present with acute urinary complaints (eg, frequency, urgency, urge incontinence), pelvic/perineal pain, cloudy urine, and systemic symptoms (eg, fever, chills, malaise, myalgia). Digital examination shows an exquisitely tender prostate that is warm and edematous. Prostate massage is not recommended, however, due to pain and increased risk of bacteremia. In addition, prostate fluid is not necessary for diagnosis.
Acute urinary retention is an infrequent complication of acute prostatitis, and bladder drainage must be done by suprapubic catheterization. Catheter insertion through the inflamed urethra into the bladder is contraindicated in acute prostatitis.
Evaluation includes urine Gram stain and culture. Empiric antibiotics that effectively penetrate the prostate (eg, oral trimethoprim-sulfamethoxazole [TMP-SMX] or fluoroquinolone) are recommended. Intravenous antibiotics are recommended for septic-appearing patients. Oral antibiotics are usually continued for prolonged periods (eg, 4 weeks) and tailored to culture results. After the infection resolves, patients usually need urologic evaluation to determine the underlying cause
Chronic bacterial prostatitis (CBP) can be a complication of ABP due to inadequate duration of treatment. CBP tends to present with less severe urinary symptoms and without significant systemic findings. Most urologists obtain urine and prostate fluid specimens after prostate massage for diagnosis. Fluoroquinolones are the preferred first-line agent. Patients usually require a prolonged course of antibiotics ranging from 6 weeks to 6-12 months in some cases.
This patient has lower urinary tract symptoms (LUTS), pyuria, and an enlarged, tender prostate consistent with chronic bacterial prostatitis (CBP). CBP can be asymptomatic or present with dysuria and increased urinary frequency. However, unlike in acute prostatitis, systemic symptoms (eg, fever, chills) are typically absent. It is usually caused by enteric gram-negative bacilli, and is a potential cause of recurrent symptoms in patients receiving an inadequate course of antibiotics for acute prostatitis. Although symptoms may be temporarily alleviated by short courses of antibiotics, the same organism can often be isolated when symptoms recur.
The diagnosis of CBP should be suspected in men with persistent or recurrent LUTS, especially if the same organism is repeatedly found on culture. Culture of prostatic secretions or urine culture following prostatic massage can confirm the diagnosis, but most patients are treated empirically. Prolonged antibiotic therapy (4-6 weeks) is recommended; fluoroquinolones (eg, ciprofloxacin) are preferred in most cases (alternate: trimethoprim-sulfamethoxazole). Treatment failure is common, and complications include prostatic abscess, bacteremia, and epididymitis.
Benign prostatic hyperplasia can cause chronic LUTS, but obstructive voiding symptoms (eg, dribbling, decreased force of stream) are usually more prominent, and this patient’s pyuria and dysuria are more consistent with CBP.
- Sx: fever, dysuria, frequency, pyuria, bacteriuria
- Ddx: UTI with cystitis vs acute bacterial prostatitis
- UTI: usually with structural problem, BPH or recent instrument
- acute bacterial prostatitis: young, middle aged men, normal anatomy with perineal discomfort or bladder obstruction
- Dx:
- Must perform digital rectal exam. Presence of prostate tenderness, edema, warmth indicates prostatitis.
- UA shows bacteruria usually gm-, e.Coli, proteus.
- Rx:
- UTI: short course cipro, bactrim
- acute prostatitis: similar abx, 6 weeks
chronic prostatitis
- ddx: either chronic pelvic pain syndrome or chronic bacterial. CPPS more common.
- dx: UA shows >20 leukocytes/hpf.
- Urine culture results then differentiate patients as having either:
- Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) - urine culture results are aseptic
- Chronic bacterial prostatitis – urine culture results show bacteriuria (>10 fold increase after prostate massage)
- rx: The underlying cause of chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) remains unclear. As a result, there is much uncertainty about the ideal approach to treatment. Most patients receive a combination of therapies including medications for prostate enlargement (eg, alpha blockers), antibiotics, anti-inflammatories, and/or psychotherapy.
After urologic procedures
This patient’s history and physical examination findings indicate acute bacterial prostatitis, and the most appropriate treatment regimen is trimethoprim-sulfamethoxazole. Patient groups at high risk for acute bacterial prostatitis include those with diabetes mellitus, immunosuppression, or cirrhosis. Risk factors include unprotected sexual intercourse, urogenital instrumentation (chronic indwelling bladder catheterization, intermittent bladder catheterization, prostate biopsy), urinary tract manipulation (prostate resection), urinary stasis (obstruction), and benign prostatic hyperplasia. The most common infectious cause for acute bacterial prostatitis is Escherichia coli or other gram-negative bacilli. Diagnosis is typically established with urine Gram stain and culture in patients with a compatible history. The treatment of choice for acute bacterial prostatitis is a prolonged course of trimethoprim-sulfamethoxazole or ciprofloxacin. Data on treatment duration are sparse, but 6 weeks is reasonable and recommended by experts. Given the prolonged duration of antimicrobial therapy required in cases of acute bacterial prostatitis, it is most prudent to select an antibiotic with appropriate coverage, while also attempting to minimize the potential for serious adverse effects. Prolonged ciprofloxacin use has been associated with QT prolongation as well as tendinopathy/tendon rupture, especially in older adults. As such, given the treatment duration needed for acute bacterial prostatitis, trimethoprim-sulfamethoxazole would be the most appropriate choice.
Amoxicillin would be an appropriate choice for patients with acute prostatitis and gram-positive cocci in chains. This finding would suggest an enterococcal infection, and treatment with amoxicillin or ampicillin would be appropriate. Neither of these antibiotics would be effective for acute bacterial prostatitis caused by E. coli or other gram-negative bacilli.
Men younger than 35 years who are sexually active and men older than 35 years who engage in high-risk sexual behavior should be treated with regimens that cover Neisseria gonorrhoeae and Chlamydia trachomatis. Ceftriaxone and doxycycline, or ceftriaxone and azithromycin, would be appropriate treatment choices in cases of acute epididymitis, specifically targeting C. trachomatis or N. gonorrhoeae. Neither regimen would be appropriate in this case.
Cephalexin would be an appropriate choice for patients with acute prostatitis and gram-positive cocci in clusters suggesting infection with Staphylococcus aureus or coagulase-negative staphylococci (Staphylococcus epidermidis or Staphylococcus saprophyticus).