restless leg syndrome and periodic limb movement
- related: Sleep and Sleep Disordered Breathing
- tags: #literature #pulmonology
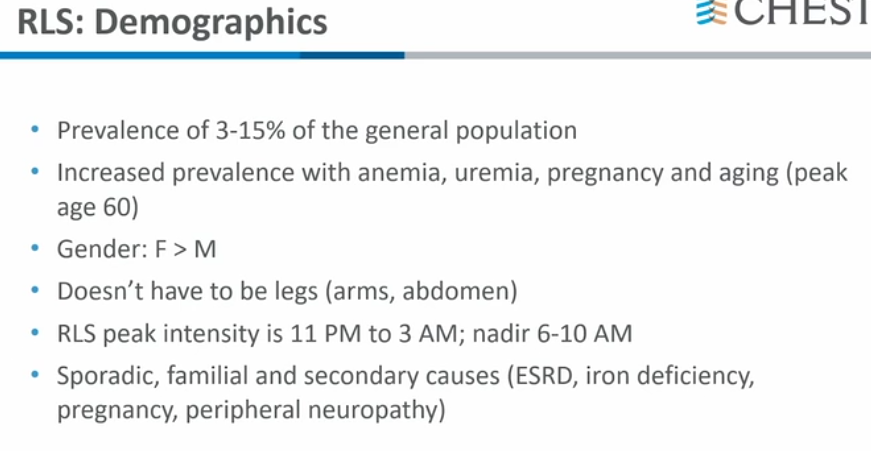
- doesn’t have to be legs
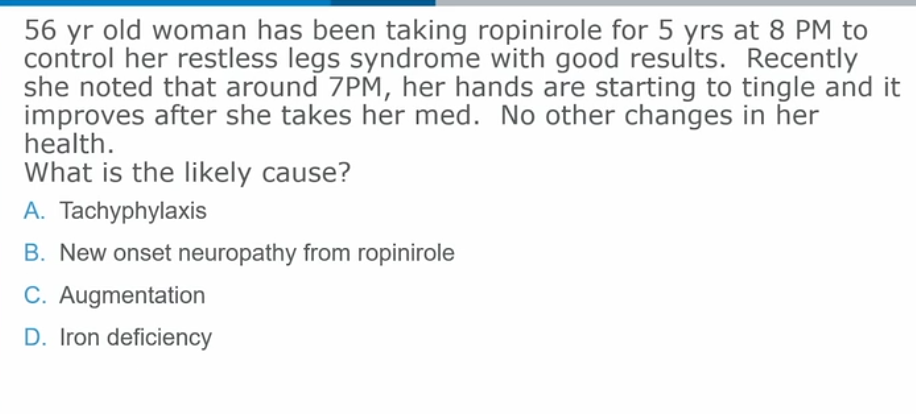
- augmentation risks:
Periodic Limb Movement
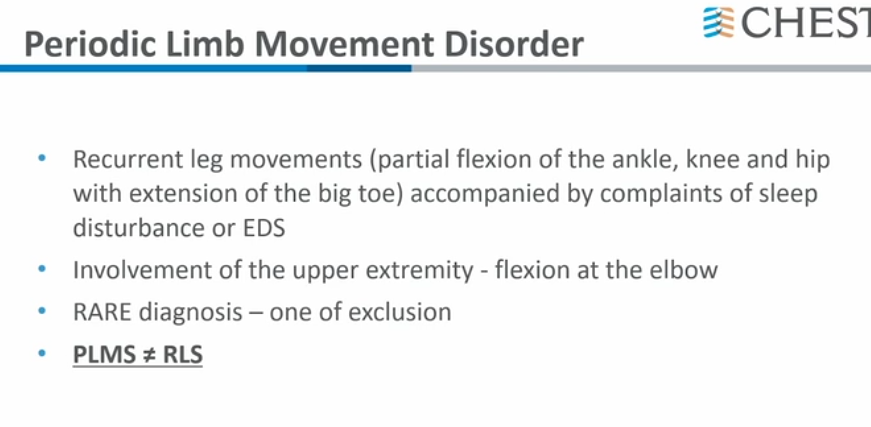
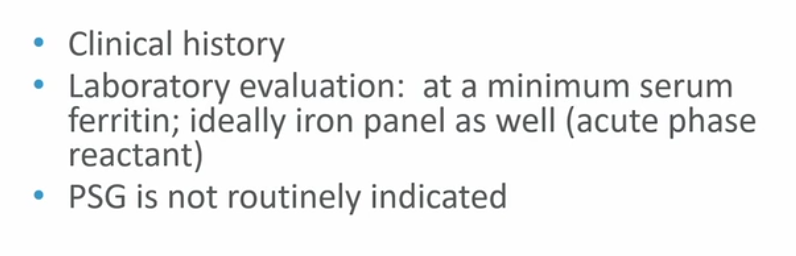
- The prevalence of PLMS in the general population increases with age and is reported to occur in as many as 57% of older adults without other neurological illnesses. Importantly, isolated asymptomatic PLMS does not require treatment. PLMD is diagnosed based on a clinical history of sleep disturbance or daytime fatigue, combined with polysomnography showing an excessive number of PLMS (above 15 leg movements per hour of sleep) and exclusion of alternative causes of sleep complaints. PLMD is a diagnosis of exclusion and cannot be diagnosed in the context of other sleep disorders associated with PLMS, including restless legs syndrome (RLS), OSA, narcolepsy, and Parkinson disease. PLMD has a much lower prevalence of 4%.
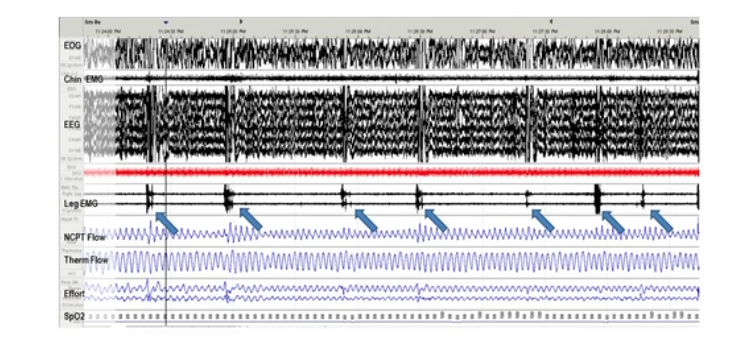
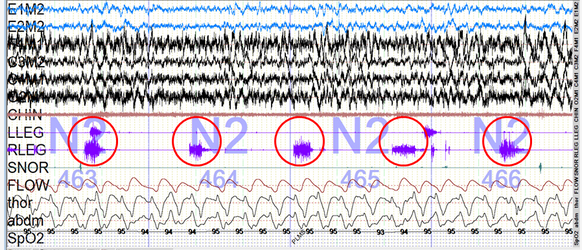
- These movements meet criteria for periodic limb movements of sleep (PLMS) because they are repetitive, highly stereotyped limb movements that are 0.5 to 10 s in duration, occur in a sequence of four or more movements, and are separated by an interval of more than 5 and less than 90s (red circles in Figure 2).
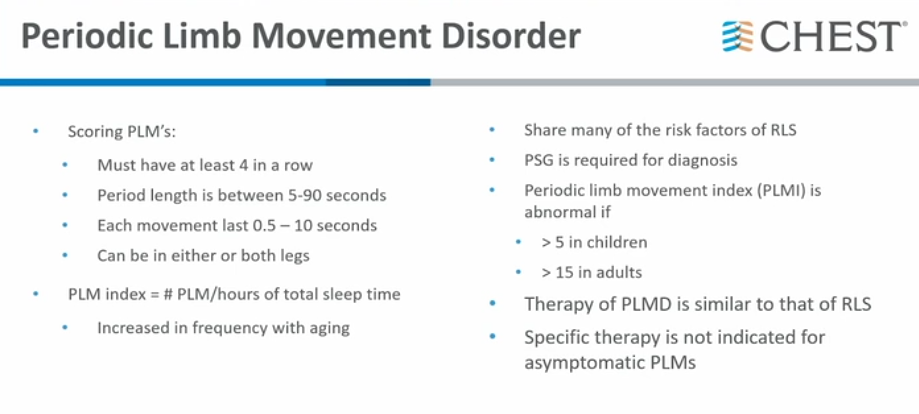
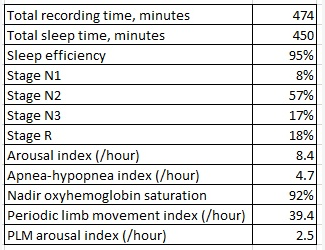
- PLMS is a polysomnographic finding that may not be clinically evident or relevant, unless accompanied by subjective sleep complaints, in which case criteria for the diagnosis of PLMD are present. In general, isolated PLMS are not an indication for further work-up. A summary of the differences between these syndromes are shown in Figure 2.
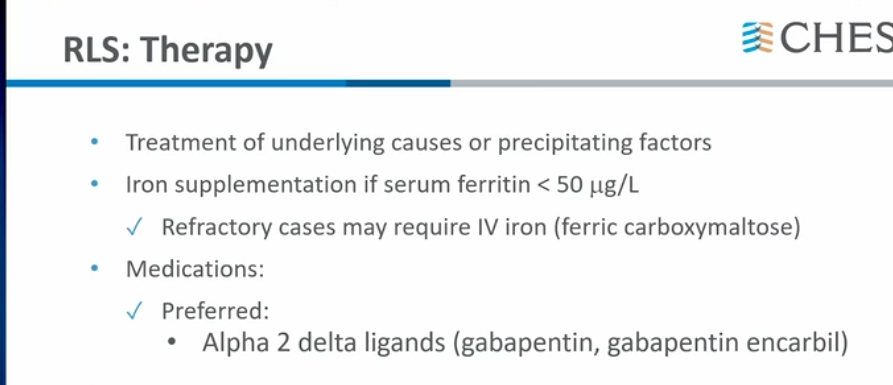
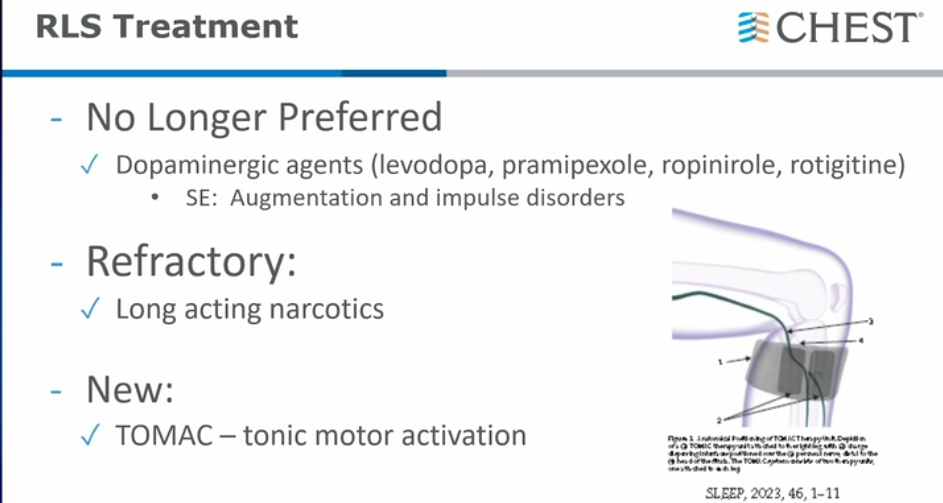
- The treatment approach to PLMD is similar to that of RLS, although most studies have been performed in patients with RLS. One of the main nonpharmacologic strategies is discontinuing or changing medications that can exacerbate RLS and PLMD. Most antidepressants can worsen RLS and PLMD, except bupropion. Sedating antihistamines and dopamine blocking agents such as metoclopramide can also exacerbate RLS and PLMD. Iron supplementation can improve RLS but has not been as thoroughly studied in PLMD. The rationale for iron supplementation, even in the absence of anemia, is based on the theory that in RLS, there is a deficit in central brain iron despite low-normal or normal peripheral iron stores. It is important not to start iron supplementation in a patient with anemia without evaluating for the underlying cause of anemia. Iron therapy should not be prescribed empirically for RLS because it may result in iron overload. Most commonly prescribed medications for RLS and PLMD are gabapentinoids (pregabalin, gabapentin, gabapentin enacarbil) and dopaminergic agents (pramipexole, ropinirole, rotigotine).1