sick sinus
- related: cardiac arrythmia
- tag: #note
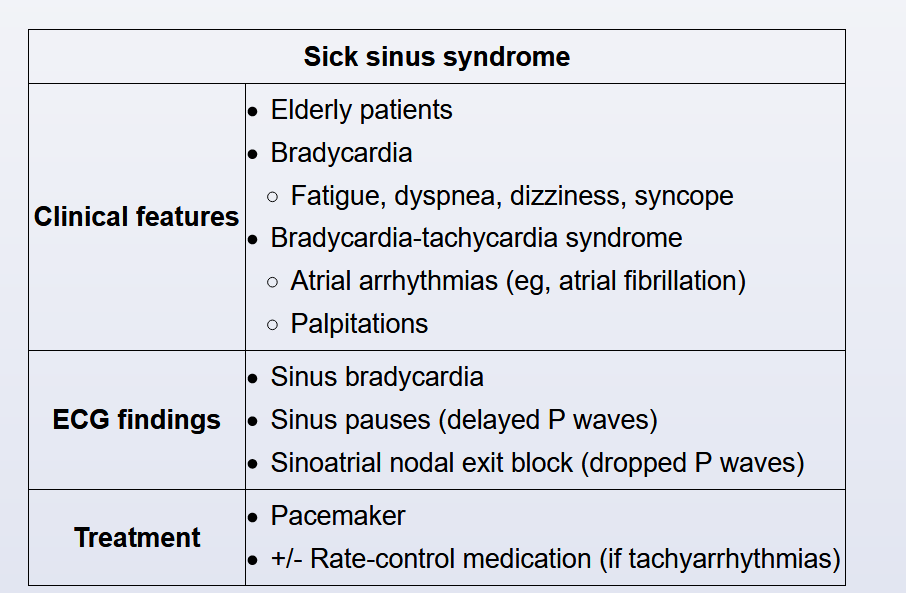
- pt: elderly
- cause: inability of SA node to generate heart rate
- pathogenesis:
- Age-related degeneration of the cardiac conduction system with fibrosis of the sinus node.
- Ischemia and infiltrative cardiac disease (eg, sarcoidosis, amyloidosis) are other potential causes.
- sx:
- bradycardia: fatigue, doe, lightheaded, confusion, syncope/presyncope
- paroxysmal atrial arrythmias from fibrosis: atrial fibrillation, bradycardia-tachycardia syndrome
- EKG:
- ECG typically shows sinus bradycardia, sinus pauses (delayed P waves), and sinoatrial nodal exit block (dropped P waves)
- In patients with bradycardia-tachycardia syndrome, a long sinus pause is typically observed on conversion from supraventricular tachycardia to sinus rhythm.
- Patients with bundle branch block are at higher risk of high-grade atrioventricular block.
- diagnose with Holter or event monitor
- treatment:
- pacemaker
- Once the pacemaker is placed tachycardia can be controlled with rate control medications.
The clue to the diagnosis of sick sinus syndrome (SSS) is this patient’s rapidly alternating supraventricular tachycardia and bradycardia, a pattern that occurs in over 50% of patients with SSS. Also known as the bradycardia-tachycardia syndrome, SSS is caused by chronic sinoatrial node dysfunction. It is defined by electrocardiographic criteria, as symptoms associated with SSS are quite variable. When patients are symptomatic, however, lightheadedness or presyncope are the most common, although dyspnea on exertion and angina are sometimes reported as well. Patients who develop SSS are typically elderly, with many medical comorbidities.
An 80-year-old woman is brought to the emergency department after an episode of near-syncope. The patient feels excessively tired and breathless on moderate exertion and has had occasional palpitations over the past 6 months. She has had several brief episodes of lightheadedness during the last 2 weeks, and while walking in a mall today, she felt extremely weak and dizzy. The patient was helped by her family and did not fall or lose consciousness. She has had no chest pain, cough, or pedal edema. The patient has hypertension and was diagnosed with paroxysmal atrial fibrillation a year ago. She takes apixaban and valsartan. Blood pressure is 156/80 mm Hg and pulse is 52/min without significant orthostatic changes. No jugular venous distension is present. Cardiac auscultation reveals regular S1 and S2 with S4 but no murmurs. Carotid pulses are full and symmetric. Breath sounds are normal with no crackles. There is no extremity edema. ECG shows sinus bradycardia and right bundle branch block. Laboratory results show normal blood count, serum electrolytes, and renal function. Which of the following is the most likely cause of this patient’s symptoms?