simple effusion, uncomplicated, complicated parapneumonic effusion, empyema
- related: pleural effusion
- tags: #permanent
Simple effusions free flowing effusions without loculations (complex fluid on US does not equal to loculation on CT or complicated effusion).
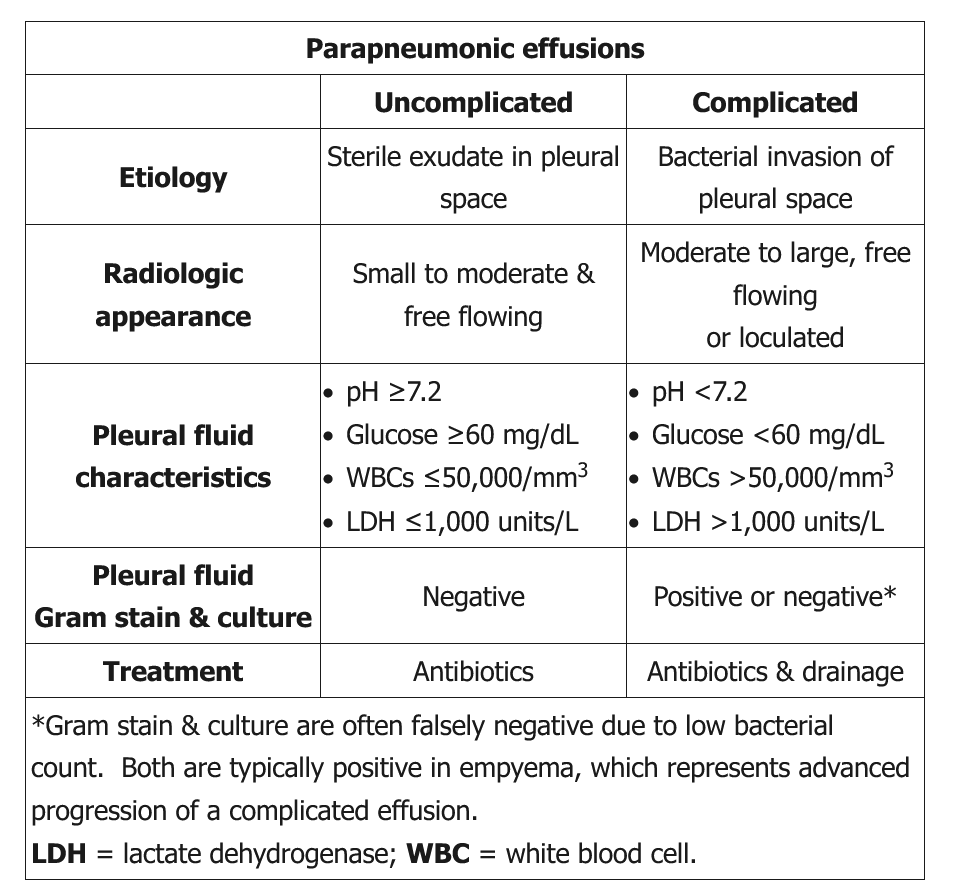
Uncomplicated parapneumonic effusion is the same as simple effusion in setting of pneumonia. Pleural fluid usually have increased WBC > 1,000/mm3 but are exudative (transudative vs exudative pleural fluid causes). On imaging, pleural fluid is usually small and free flowing.
Complicated pleural effusion are result of bacterial invasion into pleural space. This results in acidic pH, decreased glucose (used by bacteria) and increased LDH (lysis of neutrophils). On imaging fluid is usually moderate to large and can be loculated.
Empyema are complicated pleural effusion with evidence of bacterial colonization such as positive Gram stain or purulence. It’s important to note that having positive culture does not mean empyema, only positive gram stain.
Source
Parapneumonic effusion usually presents closer to the time of the presumed pneumonia with white blood cells (predominantly neutrophils) >1,000/mm3 in the pleural fluid.
Uncomplicated parapneumonic effusion refers to movement of fluid from the lung parenchyma to the pleural space due to increased hydrostatic pressure. Although the fluid is usually exudative, it typically resolves with antibiotics as the pneumonia resolves. Complicated parapneumonic effusions involve persistent bacterial invasion into the pleural space, further lowering the pleural fluid glucose (utilized by bacteria) and increasing the LDH (from lysis of neutrophils). Because bacteria can be cleared easily from the pleural space, the culture is usually negative. Some patients do resolve with antibiotics alone, but most patients also require early chest tube drainage for faster clinical recovery and hospital discharge. Observation, clinical follow-up, or repeat chest x-ray in 24 hours is reasonable for uncomplicated or complicated parapneumonic effusions treated with antibiotics.
Empyema develops due to bacterial colonization and presents with acidic pH (< 7.20), positive Gram stain for bacteria, positive bacterial culture from pleural fluid, and purulent malodorous fluid. Fluid with glucose < 60 mg/dL and pH < 7.20 does not usually resolve spontaneously and requires drainage with chest tube, sometimes with ultrasound or CT guidance. Multiple loculated collections of fluid may require multiple tubes. A chest CT should be performed within 24 hours to check tube location and assess drainage.
- Simple effusion: common, small, thin. Usually comes with pneumonia
- Conservative management, treat pneumonia, thoracentesis
- Uncomplicated parapneumonic: no septation/loculation, small to moderate sized effusion, free flowing
- Complicated parapneumonic effusion: septation, loculation, fibrinous strands from inflammatory proteins
- pH < 7.2, glucose < 40
- Thora vs chest tube (tpa, dornase)
- Empyema: worst, +culture, pus, pH < 7.2
- Chest tube or surgery
- Infection etiology
- CAP: veridans strep, pneumococci, staph aureus, anaerobes
- HAP: staph
Links to this note
-
complex fluid on US does not equal to loculation on CT or complicated effusion
-
transudative vs exudative pleural fluid causes
- Transudative fluid are normally caused by increased hydrostatic or decreased oncotic pressure. This usually happens in heart failure, cirrhosis, or nephrotic syndrome. Exudative fluid are caused by inflammation of the pleural surface and can be caused by infection (simple effusion, uncomplicated, complicated parapneumonic effusion, empyema), TB (pleural effusion in TB are exudative, lymphocyte predominant, have low glucose, and elevated adenosine deaminase), pancreatitis (elevated amylase in pleural effusion suggests esophageal rupture or pancreatitis), PE, or connective tissue disease (pleural fluid with very high LDH and low glucose are found in either empyema or rheumatoid pleurisy).
-
indications for diagnostic and therapeutic thoracentesis
- Diagnostic thoracentesis is performed to find the etiology of pleural effusions. This could be for infection workup, new onset pleural effusion without explanation, thickened parietal pleural on CT scan (pleural thickening on CT can indicate chronic inflammation or malignancy), loculation or signs of empyema (simple effusion, uncomplicated, complicated parapneumonic effusion, empyema).
-
when to place chest tube for pleural effusion
- Patients with uncomplicated parapneumonic effusion (simple effusion, uncomplicated, complicated parapneumonic effusion, empyema).