acute liver failure when to refer to transplant
- related: acute liver failure in the ICU
- tags: #literature #icu
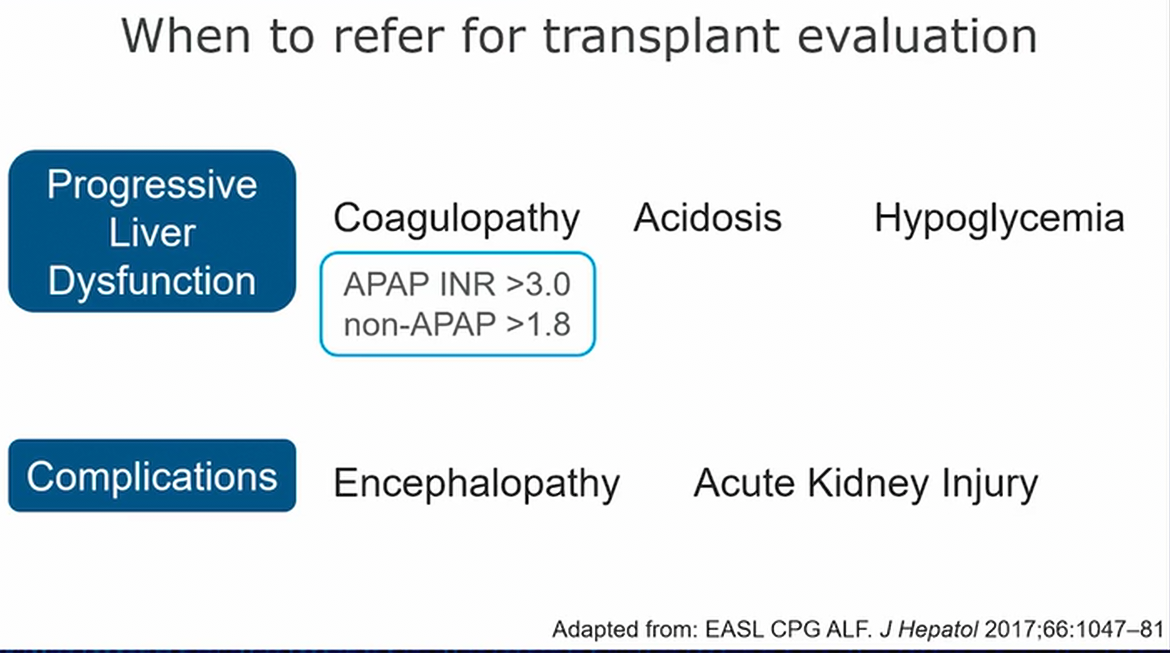
- refer when synthetic function looks bad or complications of ALF
- basically refer when there’s progression of disease, earlier than later1
Acute liver failure (ALF) is a life-threatening condition characterized by liver injury, coagulopathy (INR >1.5), and hepatic encephalopathy in patients without preexisting liver disease. This patient’s prognosis is poor based on commonly used prognostic scores, and the intervention most likely to result in survival is orthotopic liver transplantation (choice D is correct).
In North America, Japan, and Europe, the most common causes of ALF in adults include drug-induced liver injury, viral hepatitis, and cryptogenic liver failure without identifiable cause (indeterminate ALF). The incidence of indeterminate ALF varies widely in other areas of the world, and acute viral hepatitis remains the predominant etiology in resource-limited nations. Although overall and transplant-free survival has improved, associated morbidity and mortality remain high. Guidelines recommend timely referral to a liver transplant center when this diagnosis is recognized, as almost 50% of patients with ALF will require this procedure.
Massive hepatocellular injury results in a systemic proinflammatory state, subsequent expected physiologic and laboratory derangements, and rapid progression to multisystem organ failure. Concomitant infection is common, with superimposed sepsis exacerbating critical illness and its sequelae. Although prospective randomized trials (ALBIOS and ATTIRE) have not shown benefit of albumin use in decompensated liver disease, many hepatologists and transplant surgeons continue to favor its use in this setting. Guidelines recommend norepinephrine as the first-line agent for vasopressor support, often combined with vasopressin or terlipressin in cases of severe vasodilatory shock. IV N-acetylcysteine has been shown to offer a survival advantage even in cases of nonacetaminophen-induced ALF, and empiric treatment is recommended. Patients with ALF who have elevated ammonia levels are at increased risk of developing cerebral edema and intracranial hypertension. Lactulose is initiated in early encephalopathy stages to mitigate this complication, often with concomitant rifaximin, although the latter agent has not been systematically studied in this setting. Early institution of continuous renal replacement therapy (CRRT) can also effectively lower ammonia levels and has been shown to increase transplant-free survival at 21 days.
Patients with progressive encephalopathy during or despite these interventions often require intubation for airway protection. Osmotherapy with mannitol or hypertonic saline is generally initiated empirically if clinical and radiologic findings raise concern for increased intracranial pressure. The use of intracranial pressure monitoring is controversial and highly institution dependent, owing to the risk of bleeding and the lack of proven survival benefit with its use (choice A is incorrect).
The Molecular Adsorbent Recirculating System (MARSTM) is the best-known of several albumin dialysis systems (also referred to as extracorporeal liver assist devices) that allow the removal of the albumin-bound toxins that accumulate in liver failure. Unfortunately, to date, these interventions have failed to demonstrate any survival benefit except for one prospective trial in patients with acetaminophen-induced liver failure (choice B is incorrect).
Fomepizole inhibits alcohol dehydrogenase and is used to reduce the production of toxic metabolites in the setting of methanol and ethylene glycol poisoning. Hemodialysis is also an effective therapy to remove toxic alcohols and their metabolites, and the addition of fomepizole after more than 24 h of CRRT several days after potential toxic alcohol ingestion is unlikely to confer significant additional benefit for this patient (choice C is incorrect).234567
Links to this note
Footnotes
-
China L, Freemantle N, Forrest E, et al; ATTIRE Trial Investigators. A randomized trial of albumin infusions in hospitalized patients with cirrhosis. N Engl J Med. 2021;384(9):808-817. PubMed ↩
-
García Martínez JJ, Bendjelid K. Artificial liver support systems: what is new over the last decade? Ann Intensive Care. 2018;8(1):109. PubMed ↩
-
Hu W, Chen H, Ma C, et al. Identification of indications for albumin administration in septic patients with liver cirrhosis. Crit Care. 2023;27(1):300. PubMed ↩
-
Shingina A, Mukhtar N, Wakim-Fleming J, et al. Acute liver failure guidelines. Am J Gastroenterol. 2023;118(7):1128-1153. PubMed ↩
-
Vasques F, Cavazza A, Bernal W. Acute liver failure. Curr Opin Crit Care. 2022;28(2):198-207. PubMed ↩