airway management
FiO2 and liters
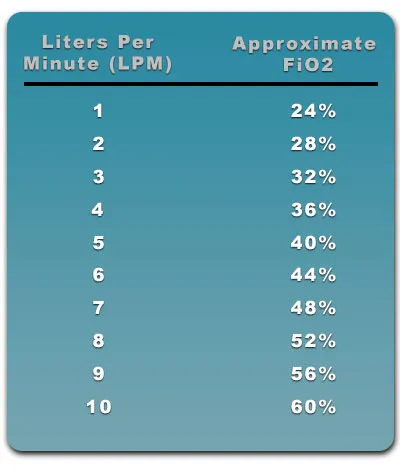
- Each liter is 4% increase
- Just remember 6L = 44%, 10L = 60%
Escalation of Oxygen Delivery
- Simple nasal cannula: up to 6L
- High flow nasal cannula: up to 15L
- Face mask: up to 15L. Use this if has nasal obstruction
- Face tent: up to 15L. Use this if claustrophobic or trauma and can’t use mask
- Optiflow: up to 60L with some PEEP
- CPAP/BiPAP
- Ventilator support
Inspiratory flow rate and minute ventilation
Inspiratory flow is the rate of gas entering the lungs during inspiration. Distressed and rapid breathing makes gas enter the lungs at a faster rate and thus a higher inspiratory flow. Patients in distress often have a high inspiratory flow rate that can range from 30 L/min to 100 L/min. Minute ventilation is the amount of gas entering the lungs over a minute and is tidal volume multiplied by the respiratory frequency.
For patients in distress, a high inspiratory flow rate is paired with a high minute ventilation because they have large tidal volumes multiple times per minute. The optimal respiratory support device should be able to accommodate a patient in distress who has a high inspiratory flow and minute ventilation. For example, when you are reading this article, you are most likely breathing 500 mL tidal volumes over 1 second and
approximately 16 times per minute. This means you have an inspiratory flow rate of 30 L/ min (500 mL over 1 second) during each breath and a minute ventilation of 8 L/min. Now, imagine a patient in respiratory distress taking 1000 mL tidal volumes over the same 1 second, approximately 30 times per minute. This equates to a much higher inspiratory flow (60 L/min) than at rest and a higher minute ventilation (30 L/min).
As you can see, the inspiratory flow and the minute ventilation of a patient in respiratory distress is greater than the 15 L/min that a non-rebreather mask (NRB) can deliver. This means that ambient room air is being inspired along with the 100% oxygen from the mask. The fraction of oxygen mixed with room air that is reaching your patient’s alveoli is dependent on the NRB flow rate, inspiratory flow, and minute ventilation. The high flow rates of up to 60 L/ min from HFNC can in many instances match the inspiratory flow of patients in distress, leading to better and more titratable oxygen delivery to the patient. In other words, the FiO2 you set on the high-flow device is close to what is actually being delivered to the patient because less ambient air is being mixed into each breath.
Patients are able to tolerate the high flow rates from a HFNC because of heating and humidification. Prior to reaching the patient’s nose, the air can be humidified to 100% and warmed to body temperature. This both improves patient comfort and preserves mucociliary function. It improves secretion management and can reduce re-intubation related to upper airway obstruction. It can also decrease the amount of energy the patient expends heating and humidifying inspired air
Simple NC
- 0.5-6L
- No point to go higher than 6L on NC as the tubing is not big enough for O2 to pass
HF NC
- 0-15L
- These are often used after simple nasal cannula
- They look exactly the same but has bigger, green tube
Face Tent
- Fixed at 15L (28-100% FiO2), but less is actually delivered because of the open system
- covers nose and mouth
- These are good for facial trauma patient, patient who are claustrophobic, patient with stuffed/broken nose
Face Mask
- 6-15L (40-60%), less is delivered because they have holes on the side
Nonbreather mask

- up to 15L (60-80%), sealed, delivers more than face mask or tent
- reservoir bag attached to the fresh gas flow
- one way valve between reservoir bag and patient -> prevents expired gas entering the reservoir bag.
- These are usually used by EMS outside hospital as optiflow is not available
Optiflow
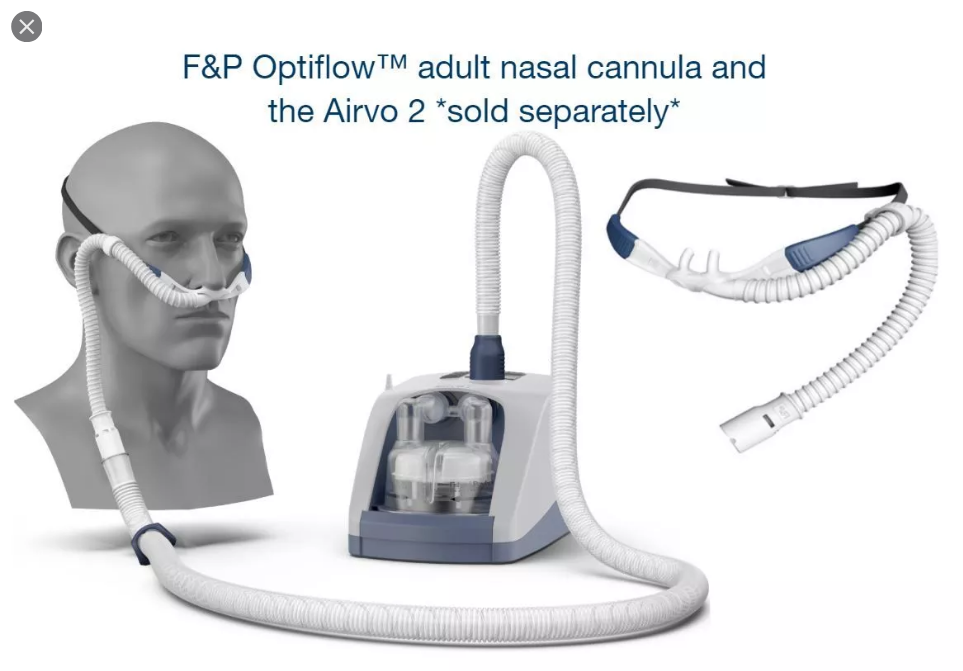
- 20-60L (up to 100%)
- Start at 40L, 40%
- Low level PEEP 2-5 cm
- active heated humidifier capable of providing 100% body humidity
- heated inspiratory circuit (avoids heat loss and condensation)
- Contraindications
- epistaxis
- base of skull fracture
- surgery to the nose or upper aero-digestive tract
- nasal obstruction; e.g. nasal fracture, tenacious secretions, tumour
Evidence
- Failure of HFNC might cause delayed intubation and worse clinical outcomes in patients with respiratory failure (Kang et al, 2015)
- The FLORALI study, a small multicenter, open-label trial found that in patients with acute hypoxaemic respiratory failure and without hypercapnia, treatment with high-flow nasal oxygen, standard face mask oxygen, or non-invasive ventilation did not result in a significantly different intubation rates. There was a significant difference in favour of high-flow nasal oxygen in 90 day mortality (Frat et al, 2015; FLORALI study)
- Preoxygenation and apnoeic oxygenation
- Compared to HFFM (high flow face mask), HFNC as a preoxygenation device did not reduce the lowest level of desaturation in an RCT (Vour’ch et al, 2015 – PREOXYFLOW trial)
- A case series of 25 patients with difficult airways undergoing general anaesthesia for hypopharyngeal or laryngotracheal surgery had mean apnoea times of 14 minutes without desaturation (i.e. SaO2 >90%) (Pateal et al, 2015; THRIVE study)
Bag Valve Mask
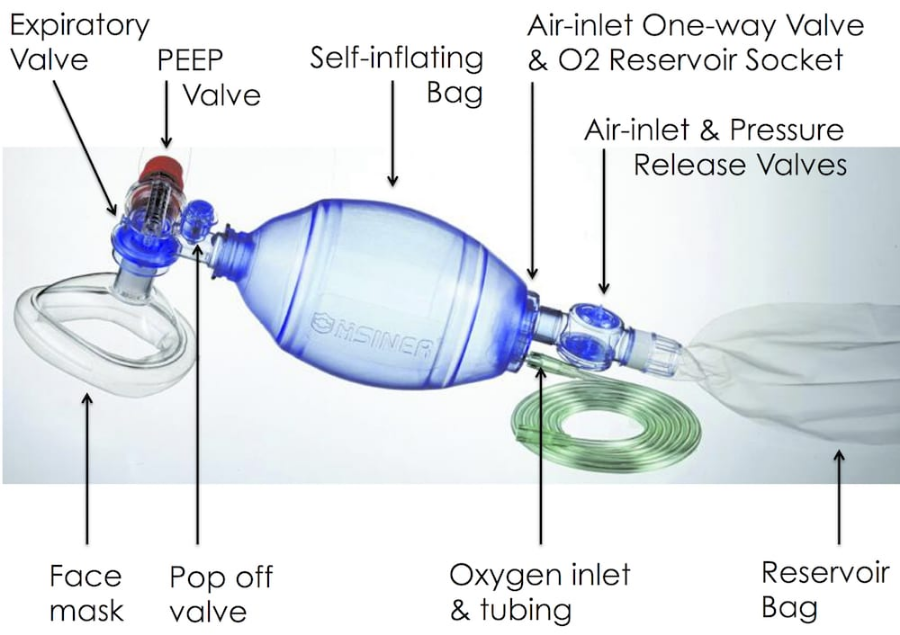
- Uses
- administration of high flow O2
- provision of PEEP (positive end-expiratory pressure)
- provision of controlled ventilation
- provision of augmentation of spontaneous ventilation
- Description
- self-inflating resuscitation device
- various sizes e.g. Laerdal 240 mL, 500 mL, 1600 mL bag sizes for infants, children and adults
- Methods
- High flow oxygen (e.g. 15 L/min) is attached to the system and it is attached to a mask or tube
- appropriate mask size
- place over mouth and nose
- tight fit
- Open airway using two-handed thumbs down technique (with an assistant bagging) in preference to the less effective one-handed C-E grip to ensure airway patency (best if OPA and NPAs in situ too)
- the bag is used to deliver oxygen to a spontaneously breathing patient or the bag compressed to manually ventilate them via a mask or tube (an assistant can provide ventilations)
- Adminstered FiO2 during spontaneous ventilation can vary greatly between devices
- Laerdal: FiO2 0.96
- Hsiner: FiO2 0.75W
- Mayo: FiO2 0.55