antibiotics pharmacology time and concentration dependence
- related: Pharmacology
- tags: #literature #pharm
Time-dependent killing (a.k.a. time above MIC)
- Key idea: The antibiotic works best when its level stays above the bacteria’s MIC (minimum inhibitory concentration) for as long as possible.
- Dose strategy: Give smaller doses more often, or continuous infusion, to keep the drug level above MIC.
- Examples: β-lactams (penicillin, cephalosporins).
- Analogy: Like keeping a light on — bacteria are suppressed as long as the antibiotic level is above the “threshold”.
Concentration-dependent killing (a.k.a. peak-dependent)**
- Key idea: The antibiotic works best when the peak concentration is very high compared to the MIC.
- Dose strategy: Give large doses less frequently to get a big peak.
- Examples: Aminoglycosides.
- Analogy: Like a hammer blow — the harder the hit, the more bacteria die.
Concentration-dependent with time dependence**
- Key idea: Killing depends on both how high the concentration goes and how long the drug stays above a certain level.
- Dose strategy: Often dosed once daily or in a way that balances both peak and exposure over time.
- Examples: Fluoroquinolones, vancomycin.
- Analogy: Like filling a bucket — you need a strong pour (concentration) and enough time pouring (exposure) to get the job done.
A conceptual approach leading to insightful antibiotic prescribing in the ICU is influenced by three categories of effects based on pharmacokinetic/pharmacodynamic considerations: time-dependent killing, concentration-dependent killing, and concentration-dependent with time-dependent killing. The various categories are represented by the choices in this question. In addition, concentrations of antibiotics may be influenced by intrinsic physicochemical properties of the drugs such as hydrophilicity and lipophilicity and by pathophysiological changes associated with critical illness such as decreased renal clearance or increased volume of distribution. See Figure 1.
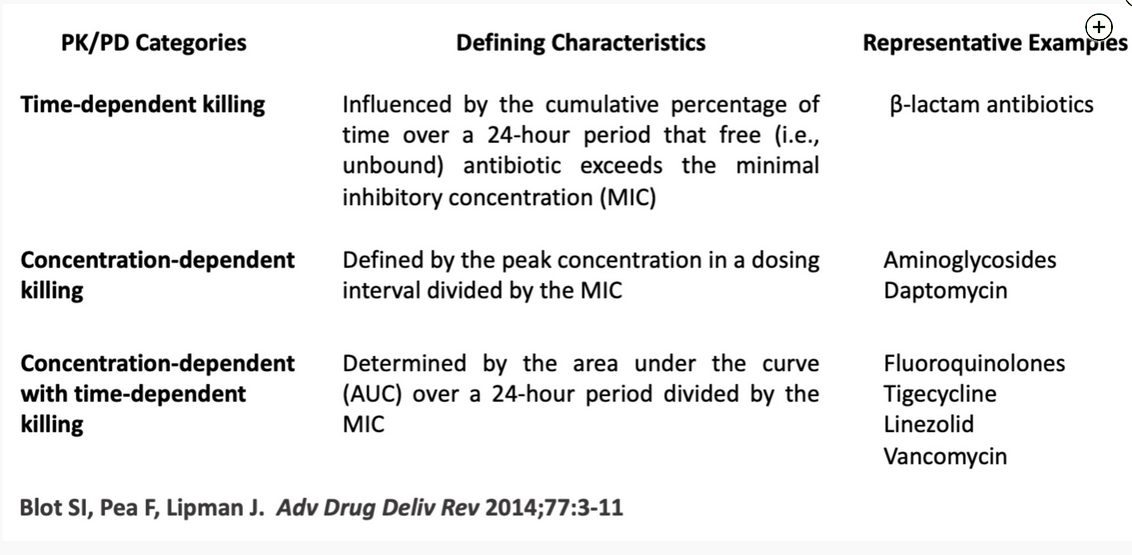
- PK = pharmacokinetic; PD = pharmacodynamic.
Piperacillin, like other β-lactam antibiotics, is hydrophilic with time-dependent killing. For more than a decade, β-lactam antibiotics have been studied as antimicrobial agents for extended or continuous infusion on the basis of the pharmacologic concept of attempting to achieve optimal bacterial killing by keeping levels of the antibiotic continuously above the minimal inhibitory concentration of the organism. Current practice conforms to the physiologic principles noted but will be tested for efficacy in the upcoming prospective phase 3 randomized controlled β-Lactam Infusion Group (BLING) III study, comparing prolonged with bolus infusion.
Vancomycin is a hydrophilic antibiotic that exhibits both time and concentration-dependent killing. The dosing interval of vancomycin is of less importance for efficacy because of vancomycin’s area under the curve. As a result of the ineffectiveness of vancomycin trough levels in predicting its efficacy, treatment guidelines published in 2020 now recommend measuring the ratio of the area under the curve to the minimal inhibitory concentration measured by broth microdilution, with a target of 400 to 600.
Linezolid is an antibiotic that is concentration dependent with time dependence. In contrast to β-lactams, vancomycin, and colistin—all of which are hydrophilic antibiotics—linezolid is lipophilic and thus is more able to pass through the alveolar epithelial cells to reach the epithelial lining fluid. In studies of linezolid, epithelial lining fluid concentrations approximated 100% of corresponding plasma values, with linezolid concentrations exceeding the susceptibility break point for Staphylococcus aureus throughout a majority of the dosing interval. On the basis of such pharmacologic properties and on clinical experience, a dose of linezolid every 12 h has been recommended in clinical guidelines for the treatment of hospital-acquired pneumonia and ventilator-associated pneumonia.
Colistin has hydrophilic properties, as demonstrated by its low volume of distribution, but it exhibits concentration-dependent killing. A major clinical challenge with colistin is that the plasma concentrations needed to achieve an antibacterial effect often overlap with the clinical levels that result in nephrotoxicity. Because of the need for efficacy without toxicity, treatment guidelines have focused on achieving a target average steady-state plasma concentration of approximately 2 mg/L for total drug.123456
Links to this note
Footnotes
-
Blot SI, Pea F, Lipman J. The effect of pathophysiology on pharmacokinetics in the critically ill patient—concepts appraised by the example of antimicrobial agents. Adv Drug Deliv Rev. 2014;77:3-11. PubMed ↩
-
Lipman J, Brett SJ, De Waele JJ, et al. A protocol for a phase 3 multicentre randomised controlled trial of continuous versus intermittent β-lactam antibiotic infusion in critically ill patients with sepsis: BLING III. Crit Care Resusc. 2019;21(1):63-68. PubMed ↩
-
Rybak MJ, Le J, Lodise TP, et al. Therapeutic monitoring of vancomycin for serious methicillin-resistant Staphylococcus aureus infections: a revised consensus guideline and review by the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, the Pediatric Infectious Diseases Society, and the Society of Infectious Diseases Pharmacists. Am J Health Syst Pharm. 2020;77(11):835-864. PubMed ↩
-
Timsit JF, Bassetti M, Cremer O, et al. Rationalizing antimicrobial therapy in the ICU: a narrative review. Intensive Care Med. 2019;45(2):172-189. PubMed ↩
-
Tsuji BT, Pogue JM, Zavascki AP, et al. International consensus guidelines for the optimal use of the polymyxins: endorsed by the American College of Clinical Pharmacy (ACCP), European Society of Clinical Microbiology and Infectious Diseases (ESCMID), Infectious Diseases Society of America (IDSA), International Society for Anti-infective Pharmacology (ISAP), Society of Critical Care Medicine (SCCM), and Society of Infectious Diseases Pharmacists (SIDP). Pharmacotherapy. 2019;39(1):10-39. PubMed ↩