aspiration pneumonia vs aspiration pneumonitis
- related: Pulmonary Diseases
- tags: #literature
Aspiration
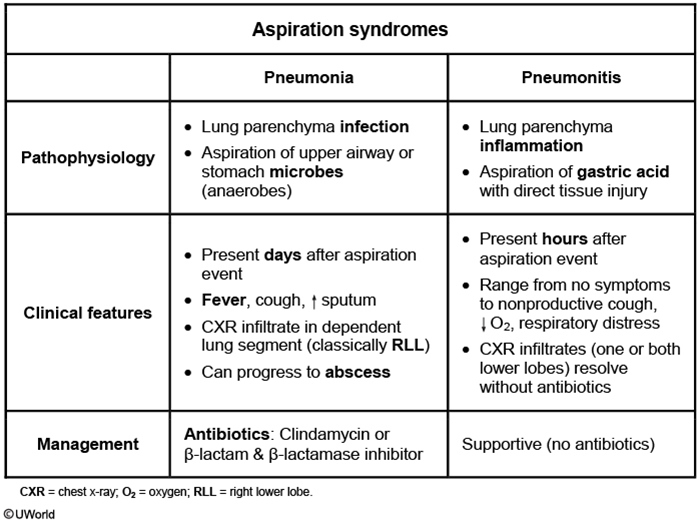
This patient had a witnessed aspiration event (vomiting during intubation that required suctioning) a few hours ago and now has profound hypoxemia with bilateral infiltrates on chest x-ray. He likely has aspiration pneumonitis, an acute lung injury due to aspiration of acidic and sterile stomach contents. The gastric acid induces a chemical burn and consequent inflammatory response, usually within hours of the aspiration event. Bilateral infiltrates can sometimes be seen on chest imaging. The symptoms (and infiltrates) usually resolve rapidly (24-48 hours) with supportive management.
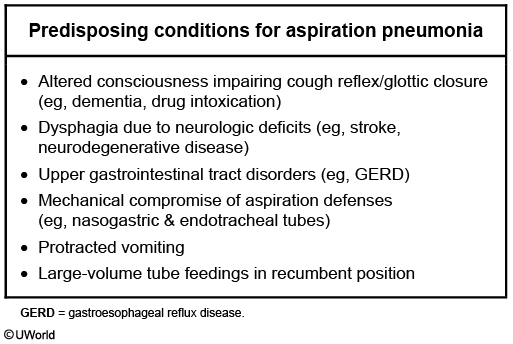
By contrast, aspiration pneumonia (Choice B), which usually occurs in individuals with impaired level of consciousness (eg, following overdose, seizure, or anesthetic use), is caused by inhalation of pathogenic bacteria that colonize oropharyngeal secretions. A typical presentation would be that of an institutionalized elderly patient who has dysphagia and develops fever and cough days (not hours) following an (often unwitnessed) aspiration event. Treatment requires antibiotics.
Patients usually present with indolent symptoms (days to weeks), foul-smelling sputum, and concurrent periodontal disease. Imaging reveals infiltrate in the lower lobes or right middle lobe (aspiration while upright) or the posterior segment of the upper lobes (aspiration while recumbent). The infectious organisms are frequently oral flora (mixed aerobic and anaerobic). Broad-spectrum antibiotics with good anaerobic coverage (eg, clindamycin, amoxicillin-clavulanate) are the mainstay of treatment.