babesiosis babesia microti
- related: Infectious Disease ID
- tags: #literature
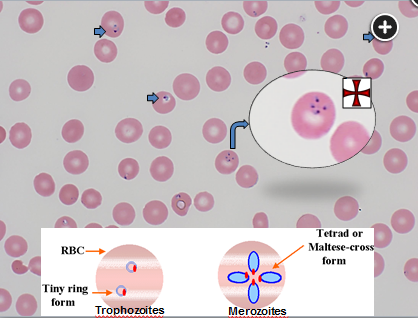 Thin blood smear with round, oval, or pear-shaped cells having a blue cytoplasm with red chromatin dots. Multiple infections per cell may be observed. Babesiosis can be distinguished from malaria by the presence of merozoites arranged in tetrads, known as a “Maltese Cross,” and this finding is uncommon but pathognomonic for babesiosis. Figure provided courtesy of Dr. Bernardo J. Selim.
Thin blood smear with round, oval, or pear-shaped cells having a blue cytoplasm with red chromatin dots. Multiple infections per cell may be observed. Babesiosis can be distinguished from malaria by the presence of merozoites arranged in tetrads, known as a “Maltese Cross,” and this finding is uncommon but pathognomonic for babesiosis. Figure provided courtesy of Dr. Bernardo J. Selim.
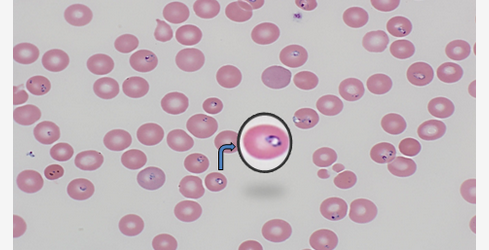
Can still have ringed looks.
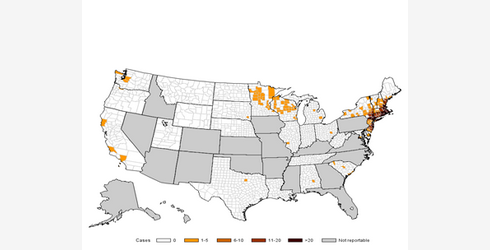
Patients with clinical manifestations of fever, fatigue, chills, sweats, headache, and myalgia in combination with laboratory features of hemolytic anemia, thrombocytopenia, and elevation of aminotransferases in the setting of a relevant epidemiologic exposure such as residents of or travelers to endemic areas, or blood transfusion in the previous 6 months should be suspected for tick-borne infections. In this case, these symptoms combined with travel to northern Minnesota and the findings of oval and pear-shaped trophozoites with a blue cytoplasm and with red chromatin dots are suggestive of infection with Babesia microti, the pathogen associated with babesiosis in the United States, particularly in the Northeast and upper Midwest where it is endemic. A graphic of geographic regions of prevalence are shown in Figure 3. Recommended treatment for babesiosis is atovaquone at 750 mg orally twice daily in combination with azithromycin 500 to 1,000 mg daily for 7 to 10 days (choice A is correct).
Complications develop in nearly half of patients hospitalized with babesiosis. The most common complications include ARDS, disseminated intravascular coagulation (DIC), and hemoglobin levels often less than 10 g/dL (100 g/L). Other complications include congestive heart failure, renal failure, and mental status changes. Most infections with B. microti are acquired by tick bites between late spring to early autumn with 75% of cases diagnosed from June through August. Risk factors for severe babesiosis include age >50, asplenism, malignancy, HIV infection, and drug immunosuppression. Ring forms of the pathogen are most common and may resemble the rings of Plasmodium falciparum seen in malaria. Babesiosis may be distinguished from malaria by the presence of merozoites arranged in tetrads (known as a “Maltese Cross”), but this uncommon finding is pathognomonic for babesiosis (Figure 4).
As many as two-thirds of patients with babesiosis experience concurrent Lyme disease, and one-third experience concurrent human granulocytic anaplasmosis, with geographic region a major determinant of coinfection. Patients with Lyme disease and babesiosis may experience a greater number of acute symptoms for a longer duration than will patients with Lyme disease alone. Patients who fail to respond to initial therapy should be assessed for coinfection.
Malaria is a life-threatening mosquito-borne blood disease transmitted to humans by the Anopheles mosquito and should be suspected in the setting of fever and relevant epidemiologic exposure to area of malaria-endemic regions and a positive malaria diagnostic test. Without travel to endemic areas where malaria is found, common treatments for malaria would not be indicated (choices B and D are incorrect).
Other forms of tick-borne illness with distinguishing features that are not found with babesiosis include erythema migrans rash (B. burgdorferi), relapsing fever (B. miyamotoi), and encephalitis (Powassan virus). Laboratory features shared by several of these infections include thrombocytopenia and elevated transaminases. The diagnosis of these diseases is established by microscopy, polymerase chain reaction, and/or serology. Treatment for many of these conditions involve use of doxycycline, which is not typically utilized for babesiosis (choice C is incorrect).1