blastomycosis
- related: Infectious Disease ID
- tags: #literature #pulmonology
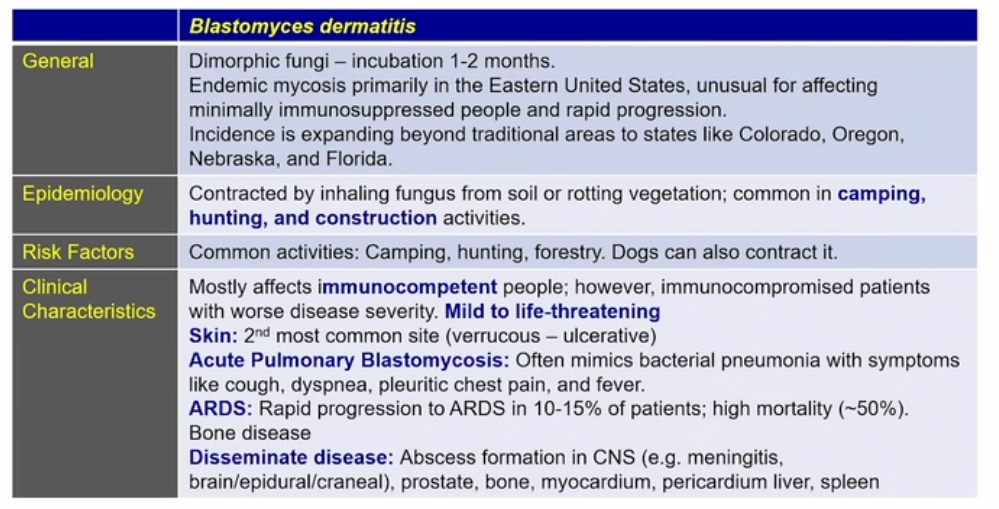
- look for hunting in the story with a dog that’s sick
- Colorado, Oregon, Nebraska, Florida
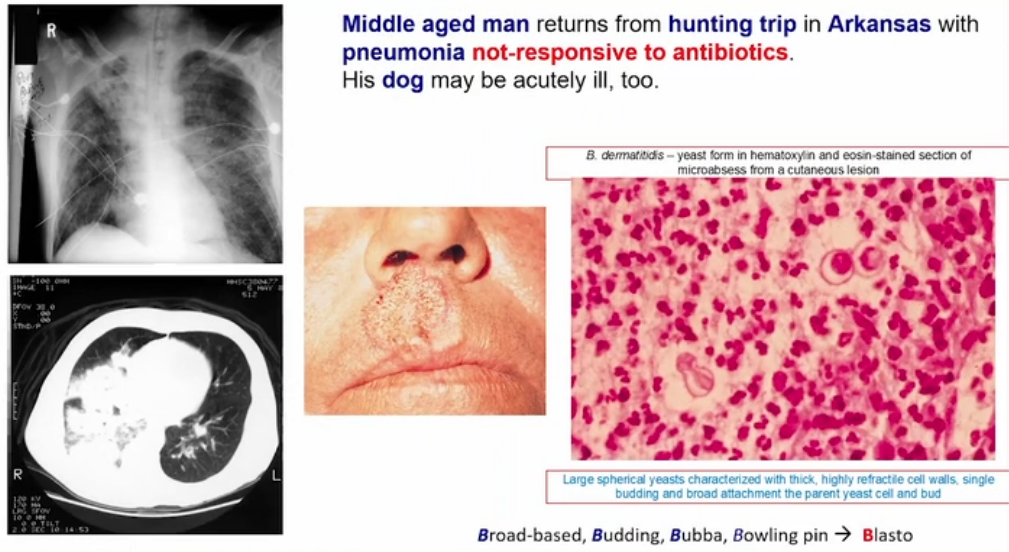

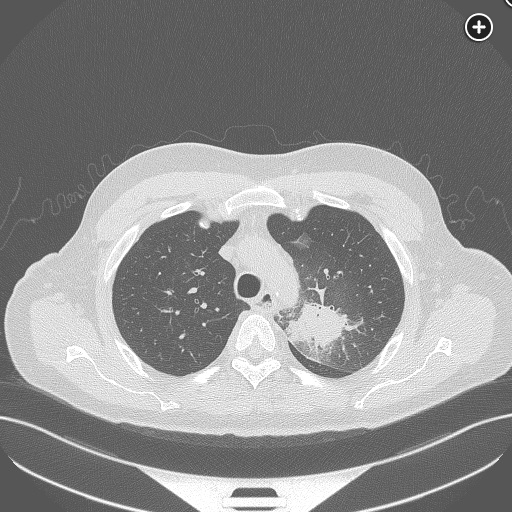
He has traveled to areas endemic of dimorphic fungi, particularly blastomycosis (Mississippi) and histoplasmosis (Arkansas) as well as some TB risk factors (travel to southeast Asia). Lack of response to treatment for bacterial community-acquired pneumonia is an early clue that dimorphic fungi or mycobacteria infections may be present. His history suggests a chronic infectious process, and his physical examination shows multiple verrucous skin lesions consistent with a fungal infections. Further, his chest radiograph and CT scan show an infiltrative and alveolar process, and the biopsy from bronchoscopy yields a broad-based yeast-like organism most consistent with blastomycosis (choice D is correct).
Blastomyces dermatitidis is a dimorphic fungus that remains in a mycelial form at ambient temperatures and grows as yeast at body temperature in mammals. It never colonizes mammals and is always pathogenic when found on biopsy or culture. Although B. dermatitidis can be found in Africa, Mexico, and Central America, it is largely endemic to North America, particularly the Ohio and Mississippi River valleys. The soil in areas endemic for blastomycosis is moist and rich with decaying organic material. Given this, periods of optimal environmental growth for B. dermatitidis can occur, leading to occasional outbreaks, usually after flooding and decay. During periods of drought, B. dermatitidis can be difficult to isolate from the environment.
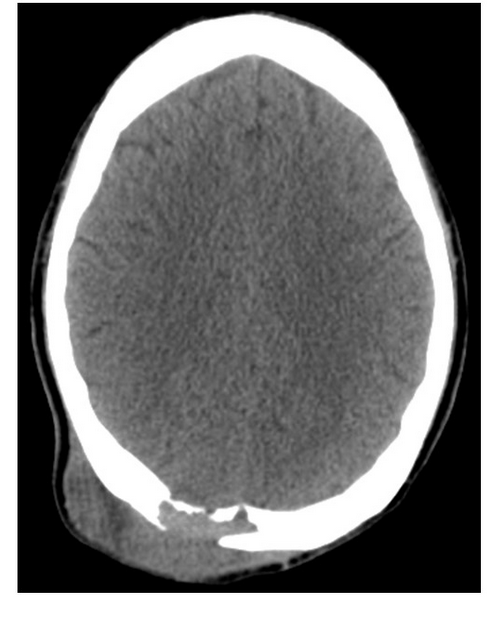
The clinical manifestations of blastomycosis include asymptomatic infection, acute to chronic pneumonia, and extrapulmonary disease. Since inhalation of conidia can lead to infection, pulmonary manifestation occurs in nearly all patients. Additional sites of infection—including skin (20%), bone, (5%), and central nervous system (2%)—occur after hematogenous spread. The incubation period from exposure to onset of pulmonary disease is highly variable but averages 4 to 8 weeks. With acute and chronic pneumonia, the symptoms are predominately cough, fever, chest pain, weight loss, and night sweats. In these cases, the patient may receive multiple courses of antibiotics without improvement, as with this patient. When seen, extrapulmonary disease occurs in conjunction with pulmonary disease and may aid in the diagnosis. The presence of skin lesions on this patient, along with travel to an endemic area, are clues that blastomycosis is present.

Extrapulmonary disease has been reported in >50% of patients with chronic blastomycosis. Following pneumonia, cutaneous lesions are the next most common manifestation of blastomycosis. The characteristic cutaneous finding is a verrucous lesion with irregular borders. Subcutaneous nodules, as seen in this patient, represent cold abscesses that can be seen in patients with disseminated disease. Osteomyelitis is the second most common extrapulmonary manifestation of blastomycosis infection and is reported in up to a quarter of patients with multiorgan involvement. A well-circumscribed lytic lesion with surrounding soft-tissue swelling or a chronic draining sinus tract are common radiographic findings. Joint infection manifested as a monoarticular arthropathy presenting with effusion results from direct extension from osteomyelitis.

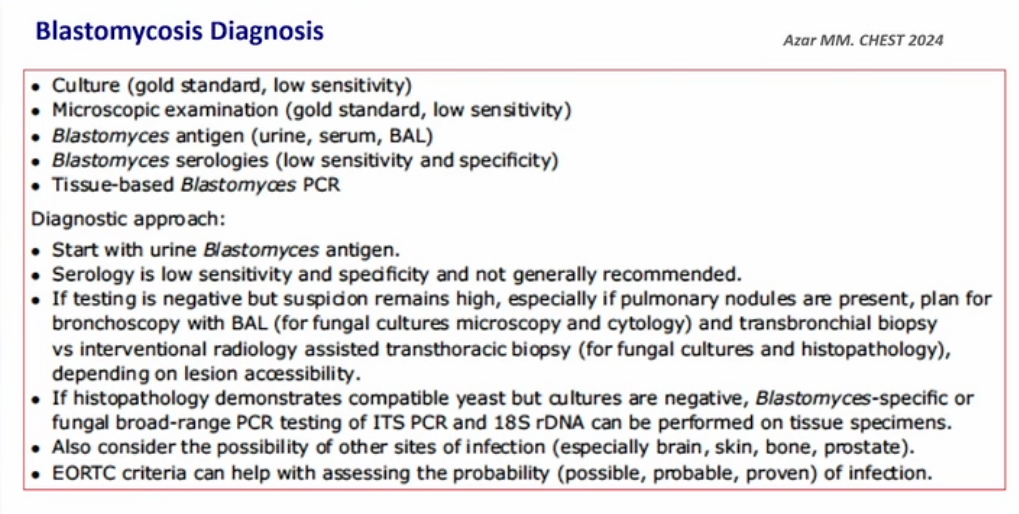
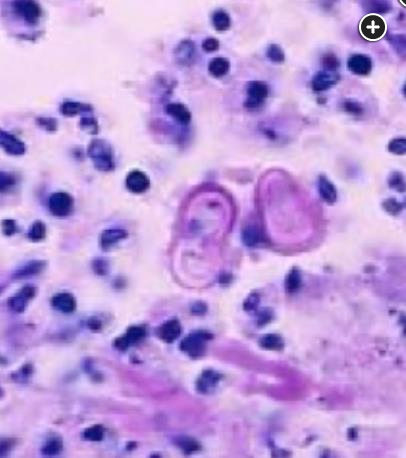
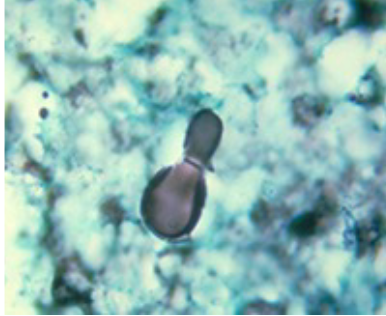
As infections with dimorphic endemic fungi can be similar, diagnosis through testing and biopsy is paramount. B. dermatitidis is easily isolated from pulmonary and other specimen sites when grown on Sabouraud agar. Growth usually takes 2 to 4 weeks for the classic mycelial form to be identified. However, reliable diagnosis is often made on direct visualization of the tissue. The yeast forms in tissue of each of these organisms are very distinct and can confirm the diagnosis. For Coccidioidomycosis, very large spherules are seen on low power (Figure 5), while with histoplasmosis, the organisms can be small and round, significantly smaller than the surrounding cells (Figure 6). Blastomycosis is larger with a thick capsule and a distinctive daughter-bud with a broad base, distinguishing it from Cryptococcus spp. (Figure 7, Figure 4). Sporothrix is small but is more cigar-shaped (Figure 8).
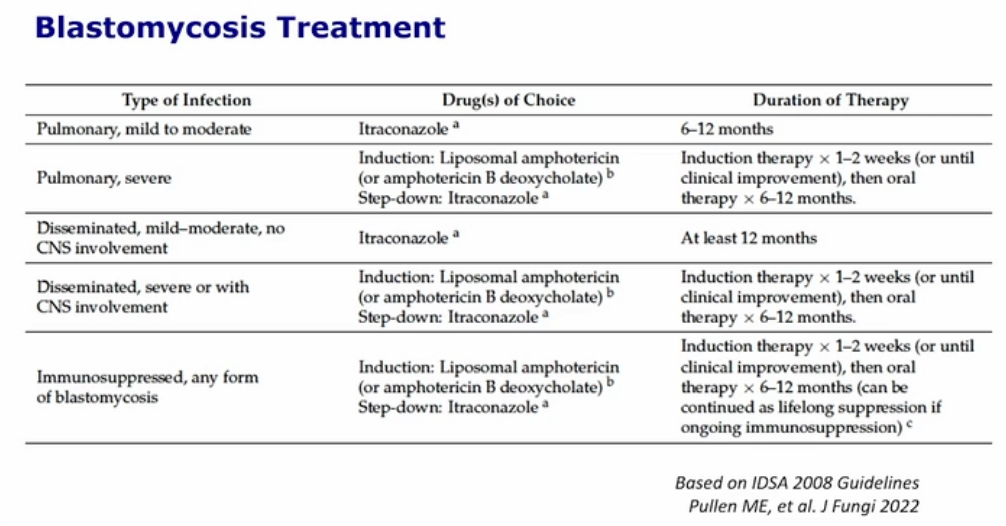
TB would appear with caseating granulomas on biopsy and is less likely in the absence of acid-fast organisms on sputum (choice A is incorrect). Coccidioidomycosis would have large spherules on biopsy (choice B is incorrect), while histoplasmosis is small, round, and often intracellular within pulmonary macrophages (choice C is incorrect). This patient improved after 90 days of oral itraconazole.1