bradycardia
- related: syncope, Cardiology, Arrythmia
- tag: #literature #cardiology
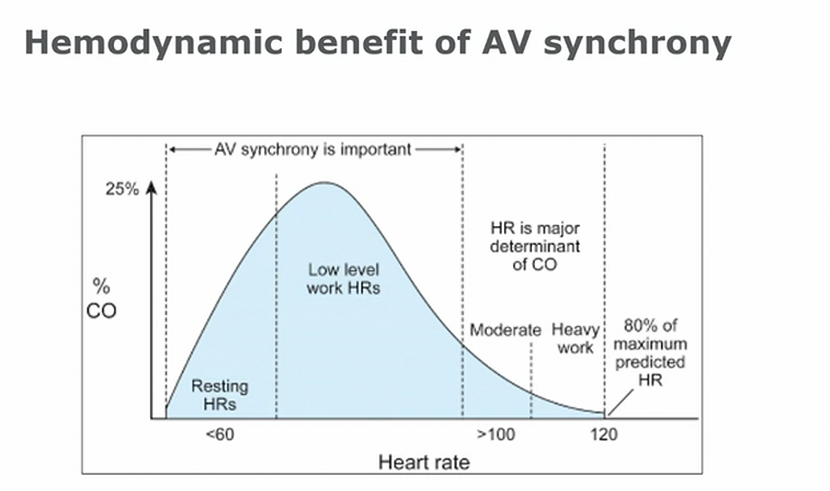
- AV synchrony can account for up to 25% of HR
- Higher HR = more heart rate response for CO
SA node dysfunction
sinus bradycardia
Other types of sinus node dysfunction
- sinus arrest, junctional escape rhythm
- sinus with pauses
- tachybrady syndrome
- sinoatrial exit block: failure of impulse to exit SA
- secondary sinoatrial exit block:
- failure of p wave to form
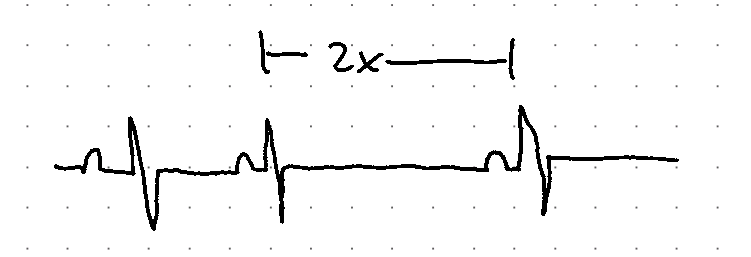
- p to p shortening, followed by drop beat
- failure of p wave to form
- Sx
- usually asymptomatic, syncope, fatigue, lightheadedness, dyspnea
- Treatment
- symptomatic patient: pacemaker
- atrial based pacing support
- most patient get RV lead for backup
- high vagal tone: very dramatic bradycardia with normal HR between episodes
- sinus slowing before bradycardia
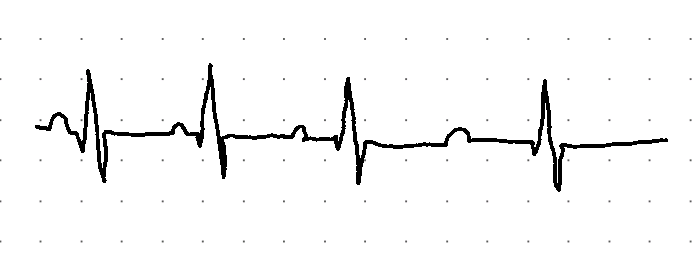
- nausea, vomiting, diaphoretic
- SA node dysfunction: lower HR at baseline
AV nodal block
Bradycardia after MI
treatment
Inpatient
Outpatient
- pacemaker indications
- symptomatic bradycardia with no reversible cause
- permanent afib with symptomatic bradycardia
- alternating BBB
- 3rd degree block, Mobitz 2, high degree AV block (>1 nonconducted P)
- treat if EF < 40%
- biV pacemaker because RV pacing alone = worse EF
- Pace RV: wide QRS, LBBB
- if RBBB develops followed by pacing: biV pacemaker
- < 30%: ICD CRT biV pacing
- CXR: pacemaker = skinny. atrial = ventricular
- icd: coil at RV insertion
- Biv: 3rd lead, RV anterior, LV posterior
Links to this note
-
- related: Cardiology, cardiac pacemaker, bradycardia
-
bradycardia can happen after MI
- related: bradycardia, STEMI treatment
-
- related: bradycardia
-
- related: bradycardia
-
transvenous pacing indications
- related: bradycardia
-
treat sinus bradycardia with medications
- related: bradycardia