brain death exams
- related: ICU intensive care unit
- tags: #icu
Brain Death

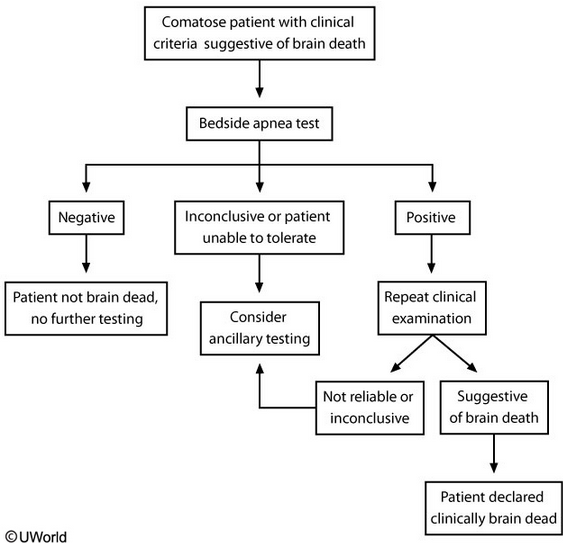
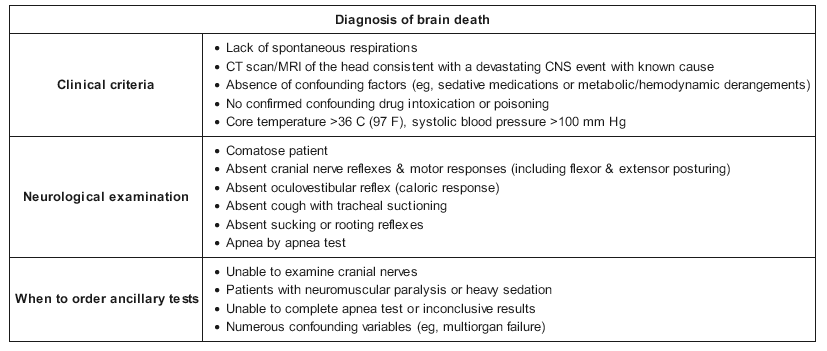
When clinical criteria suggest brain death, the best next step is apnea testing. Patients must be hemodynamically stable with a body temperature > 36 C (97 F), normal pH, and normal PaCO2/PaO2 levels. Apnea testing objectively confirms brainstem failure if the patient cannot generate spontaneous breaths or trigger the ventilator in response to elevated PaCO2 levels > 10 minutes after disabling control mode (Choice E).
Patients are first pre-oxygenated with 100% oxygen for 10 minutes using existing ventilatory support, and then mechanical ventilation is discontinued. However, they should continue to passively receive 100% oxygen while the chest and abdomen are observed for spontaneous respirations for approximately 10 minutes. If spontaneous respirations are observed, the apnea test is negative and the patient is not brain dead. A positive test is defined as no spontaneous respirations and requires another clinical brain death examination for confirmation. In addition, repeat ABG must confirm that the PaCO2 was > 60 mm Hg or that it increased > 20 mm Hg from the baseline ABG. Patients who cannot tolerate apnea testing or have inconclusive results require ancillary diagnostic tests to confirm brain death.
(Choice A) The atropine response test involves administering atropine and observing for an increase in heart rate (> 3%). Although the vagal nucleus in the medulla may be one of the last functions lost in brain death, the atropine response test provides a limited assessment and has not been well validated for confirming brain death.
(Choice C) Cerebral blood flow testing (e.g., cerebral angiogram or cerebral scintigraphy) is the gold standard test for brain death confirmation, but it is highly invasive and not used routinely as the initial step for diagnosing brain death. Cerebral blood flow testing may be used in patients with an unreliable clinical examination or bedside apnea test.
(Choice D) Current guidelines do not recommend EEG with ECI protocol for brain death confirmation, as it is susceptible to excessive artifact from other electrical devices in the ICU that make it less reliable. In addition, EEG is very sensitive to the effects of sedative medications and metabolic derangements, and therefore can be easily confounded by those variables.
This patient has a high likelihood of having evolved to irreversible cessation of brain function. Determination of brain death includes apnea testing, defined as a failure of the medulla to drive respiratory efforts despite an elevation of the PaCO2 to 60 or 20 mm Hg higher than a known elevated baseline (choice A is correct).
The need for determination of brain death by means of clinical assessment arises as a result of the growing frequency in the use of life support in the modern hospital over the past 70 years. After determination that either a direct (eg, stroke, trauma) or indirect (eg, hypoxia, cardiac arrest) insult has caused irreversible cessation of all functions of the entire brain, including the brainstem, death can be declared, with a legal basis for this determination provided in the United States by the Uniform Determination of Death Act. This process accounts for approximately 2% of hospital deaths (choice B is incorrect).
General principles that guide this determination include beginning with identification of the mechanism of brain injury and exclusion of conditions that suppress neurologic function and potentially confound determination of brain death such as hypothermia, shock, and drug overdose. In most jurisdictions, well-documented, thorough, bedside neurologic examinations can by themselves be used to diagnose brain death, although in ambiguous circumstances or when the neurologic examination is necessarily limited, ancillary testing, including imaging; EEG; and, most importantly, blood flow measurement, are used. In cases of global anoxic injury, such as that after cardiac arrest, it is generally recommended that two examinations 24 h apart be conducted; nonetheless, study results have shown that return of neurologic function at the time of the second examination is not seen after proper testing in many patients (choice D is incorrect).
The neurologic examination for determination of brain death begins by confirmation of coma by nonresponsiveness to auditory, visual, or tactile stimuli. Testing for tactile pain should include stimulation not only of arms, legs, and trunk but also of the supraorbital notch and the temporomandibular joint because high cord lesions or peripheral neuropathies may confound a more limited examination (choice C is incorrect). Testing for brainstem reflexes includes pupillary, corneal, oculocephalic, oculovestibular, gag, and cough reflexes, which all must be absent. This testing is essential to avoid interpreting high cord or low brainstem lesions producing a locked-in syndrome as true brain death.
If these indicate no cortical or brainstem function, apnea testing is conducted. The absence of respiratory effort in response to hypercarbia and acidosis is consistent with brain death. The risk of this procedure is cardiovascular collapse caused by hypoxia. Accordingly, cardiovascular stability should be established before testing is attempted, and preoxygenation to PaO2 higher than 200 mm Hg is desirable. At this point, the patient is removed from mechanical ventilation, and apneic oxygenation is provided through a tracheal catheter with an oxygen flow rate of 4 to 6 L/min. For at least 10 min, the patient is observed for respiratory efforts, the presence of which would exclude brain death. Arterial blood gases are followed, and when the PCO2 exceeds 60 mm Hg or climbs by more than 20 mm Hg in a patient with chronic CO2 retention, the test is interpreted as consistent with brain death. In cases in which severe hypoxemic respiratory failure has occurred and the patient is PEEP dependent to avoid severe hypoxemia, there may not be adequate time off the ventilator to secure a diagnosis of brain death through apnea testing.1
The determination of death by neurological criteria (DNC) is one of the most important and poorly understood evaluations in critical care. Over time, the procedure for the determination of DNC has become stereotyped and mechanical, which has led to a decrease in recognition of DNC as a diagnosis made by a clinician (similar to acute respiratory failure or acute myocardial infarction). There are three fundamental tenets of making the diagnosis of DNC in a patient who is comatose. First, there must be a mechanism that explains why the patient is in a coma (choice B is correct). There are two mechanisms by which a person who has DNC could have cessation of blood flow to the brain: (1) increased pressure in the calvarium that exceeds the mean arterial pressure (herniation) or (2) loss of metabolic demand for blood because of cessation of function of the brain at a cellular level. In some cases, the cause is obvious, such as in a massive intracerebral hemorrhage with herniation. In other cases, such as in massive insulin overdose that can lead to complete brain cessation of function on the basis of energy failure, it may be more challenging to determine. With the refinement of imaging techniques of the brain (CT scanning, MRI, PET, and single-photon emission CT scanning), it has become easier to identify the cause for cessation of blood flow. In rare cases, delaying the diagnosis of DNC may be necessary to allow the process that is affecting the brain to become identifiable.
Second, the patient must have a physical examination that is consistent with DNC. Although there is sometimes mystery about the “brain death examination,” it can be thought of simply as the neurological examination that can be completed in a patient who cannot cooperate with the examiner. To be consistent with DNC, examination findings of reactions that are mediated by the brain must be absent. The patient must not respond to attempts at arousal. The confrontational cranial nerve examination (testing functions by stimulating sensory systems) must show no response to stimulation (choice C is incorrect).
The patient must show no signs of response to painful sensory stimulation in central and peripheral locations that are mediated by the brain. Predictably, some patients who meet the conditions for the diagnosis of DNC retain spinal reflexes (because they are not mediated by the brain) like the plantar response (Babinski sign) (choice A is incorrect).
Finally, the patient must not attempt to initiate a breath when challenged by increased PCO2 (a physiological signal to initiate a breath). This is most commonly performed by discontinuation of the ventilator in a test known as the apnea test. The test is performed by discontinuation of mechanical ventilation after a period of hyperoxygenation. At intervals of 5 to 8 min, arterial blood gases are sampled to determine whether the PCO2 is sufficiently elevated to guarantee initiation of a breath in a living person. The test is discontinued and considered inconsistent with DNC if the patient initiates a breath before the PCO2 reaches the end-point level. Two common complications with this test are hypoxemia and hypotension. Both can be mitigated in most patients by ensuring adequate preoxygenation and maintaining euvolemia. In some patients who are unstable, hypoxemia or hypotension necessitates stopping the test. If the test must be discontinued, it does not invalidate the diagnosis of DNC (the patient may be dead). It means that the test does not contribute to the diagnosis (choice D is incorrect). If any of the three parts of testing (cause of coma, physical examination, or apnea test) cannot be completed, an ancillary test can be performed to help make the diagnosis of DNC by showing absence of blood flow to the brain.
Using this paradigm of diagnosis by well-trained, conscientious clinicians, there has not been a credible case of a patient being diagnosed dead by neurological criteria who has regained brain function.23
This patient sustained a catastrophic neurological injury with a clinical exam consistent with a diagnosis of brain death, and the next step in the evaluation of this patient is to complete the full clinical evaluation for the determination of brain death by conducting an apnea test (choice B is correct). To avoid the implication that brain death is distinct from other types of death, many have advocated for “death by neurological criteria” as the preferred terminology for this scenario.
An absent respiratory drive manifested by failing to trigger assisted breaths while receiving assist-control mechanical ventilation or failing to initiate breaths while on a spontaneous mode of mechanical ventilation is not sufficient to determine brain death. The elements of the apnea testing procedure are not supported by high-quality evidence, and the requirements may vary by institution. The standard, guideline-endorsed approach to the apnea test includes the following general steps: (1) the ventilator is set to 1.0 FiO2 for >10 min to maximize initial PO2 (goal >200 mm Hg); the PEEP is reduced to 5 cm H2O, and the ventilator is manipulated to achieve a PCO2 between 35 and 45 mm Hg established by a baseline arterial blood gas; (2) the patient is disconnected from the ventilator, and supplemental oxygen is provided through a cannula within the trachea, a T-piece system, or CPAP of 10 cm H2O; (3) once the patient is disconnected from the ventilator, the physician visually observes for any respiratory efforts, including gasps or other spontaneous respiratory movements; (4) a repeat arterial blood gas is obtained between 8 and 10 min. The apnea test is considered supportive of brain death if there are no observable respiratory efforts and the PCO2 rises to >60 mm Hg or increases more than 20 mm Hg above baseline.
This patient meets the prerequisites necessary for brain death determination. The prerequisites are known cause of catastrophic brain injury, no receipt of or residual effects of CNS depressants or paralytic agents, no metabolic abnormalities, normothermia, and a systolic BP ≥100 mm Hg. While this patient is receiving norepinephrine, it is important to note that it is acceptable to use vasopressors to achieve the systolic BP goal of 100 mm Hg, and this would not preclude a patient from a determination of brain death by clinical criteria or apnea testing. Once the prerequisites are met, the next step in the brain death examination is a full neurological evaluation, including confirmation that the patient is in a coma without brain-originating movement (eg, absence of seizures, decorticate or decerebrate posturing, purposeful movements, and grimacing or other motor response to noxious stimuli). The exam also includes a full brainstem reflex and cranial nerve evaluation, including absent corneal, oculocephalic, oculovestibular (cold caloric), gag, and cough reflexes and no response to painful stimuli at the supraorbital notch and temporomandibular joint. Once these findings are confirmed, like the patient described in this case, the next step is apnea testing.
Ancillary tests for brain death (including cerebral angiography and nuclear medicine cerebral perfusion scans) are used when a patient cannot undergo a full clinical evaluation (including full neurological exam) or when the apnea test cannot be successfully completed. Common reasons that ancillary tests are required include traumatic injuries to the head and neck precluding a full brainstem exam, hemodynamic instability precluding an apnea test, multiorgan failure leading to metabolic abnormalities that cannot be normalized, or chronic hypercapnic respiratory failure precluding a complete apnea test. Ancillary tests are not required for the determination of brain death in adult patients for whom the full brain death clinical evaluation can be successfully completed (choices A and D are incorrect).
High serum concentrations of neuron-specific enolase have been associated with poor prognosis in patients who have sustained cardiac arrest, but this test does not have a role in the diagnosis of brain death (choice C is incorrect).456
Links to this note
Footnotes
-
Kirschen MP, Lewis A, Rubin M, et al. New perspectives on brain death. J Neurol Neurosurg Psychiatry. 2021;92(3):255-262. PubMed ↩
-
Lewis A, Greer D. Current controversies in brain death determination. Nat Rev Neurol. 2017;13(8):505-509. PubMed ↩
-
Greer DM, Wang HH, Robinson JD, et al. Variability of brain death policies in the United States. JAMA Neurol. 2016;73(2):213-218. PubMed ↩
-
Streitberger KJ, Leithner C, Wattenberg M, et al. Neuron-specific enolase predicts poor outcome after cardiac arrest and targeted temperature management: a multicenter study on 1,053 patients. Crit Care Med. 2017;45(7):1145-1151. PubMed ↩
-
Wijdicks EF, Varelas PN, Gronseth GS, et al; American Academy of Neurology. Evidence-based guideline update: determining brain death in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2010;74(23):1911-1918. PubMed ↩