bronchial atresia is a congenital anomaly that can cause mucous impaction
- related: pulmonary anatomy
- tags: #literature #pulmonology
Although this patient’s history and spirometry findings—which show evidence of small airway dysfunction—are nonspecific, the imaging findings are highly suggestive of bronchial atresia (BA). BA is a rare congenital developmental anomaly resulting from focal obliteration of a lobar, segmental, or subsegmental bronchus, typically complicated by mucous impaction and/or air trapping distal to the atretic bronchus. The condition likely occurs in embryonic development. The apicoposterior segment of the left upper lobe is most commonly affected. Rarely, patients may present with dyspnea, pneumonia, or bronchial asthma, but because most patients are asymptomatic, the abnormality is an incidental finding in approximately half of cases.
BA is associated with mucous impaction and hyperinflation distal to the lesion. Mucous impaction occurs because bronchial secretions are unable to be cleared into the central airways. The lack of communication from the bronchus also leads to hyperinflation; although ventilation does not occur directly through the airway, distal alveoli become distended by collateral ventilation through the bronchiole-alveolar channels of Lambert and intra-alveolar pores of Kohn. These collateral routes collapse during expiration, which leads to air trapping. Despite superficially resembling emphysema on thoracic imaging studies, hyperinflation from BA is distinct in that the damage to the alveolar walls is minimal or absent. A bronchocele (impacted mucoid secretion) is seen as rounded opacities that may contain an air-fluid level, radiating from the hilum. If filled with mucus, the mucocele is often noted as a solitary pulmonary nodule and may be misinterpreted as an arteriovenous malformation, granuloma, or metastatic lesion.

- Posteroanterior end-expiratory chest radiograph showing hyperinflation of the left upper lobe around the perihilar area of increased opacity (arrow).
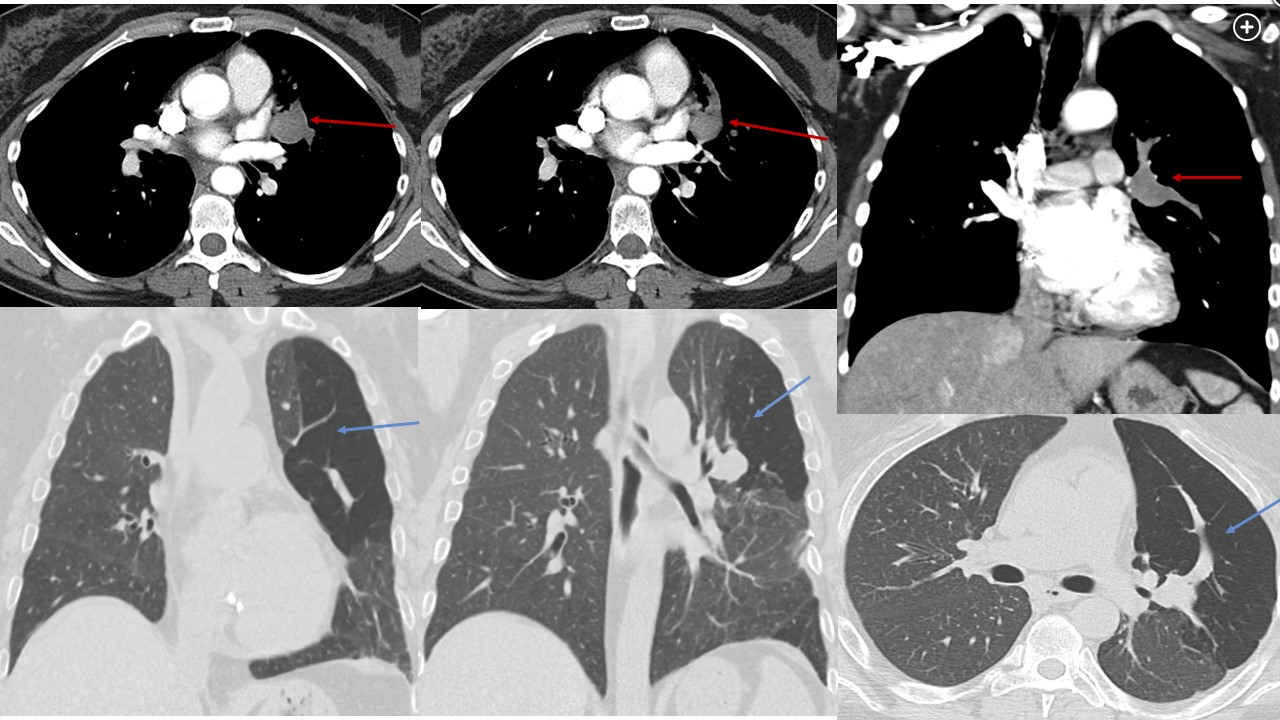
- Chest CT scans with IV contrast (axial and coronal views) show a perihilar tubular, nonenhancing lesion of the apicoposterior left upper lobe bronchus (bronchocele) (red arrows). Decreased attenuation is seen throughout the apicoposterior segment of the left upper lobe, a finding indicative of associated air trapping (blue arrows).
Chest radiography often shows a tubular area of increased opacity that extends from the left hilum into the left upper lobe. On the expiratory view, there is persistent hyperinflation of the left upper lobe around the area of increased opacity (Figure 3). The hyperlucency surrounding the area of increased opacity is indicative of air trapping. Contrast-enhanced CT shows a tubular nonenhancing lesion, a finding consistent with mucous impaction of the apicoposterior left upper lobe bronchus (bronchocele). Decreased attenuation is seen throughout the apicoposterior segment of the left upper lobe, a finding indicative of associated air trapping (Figure 4). These CT features are diagnostic of BA. Although not required to establish a diagnosis, a quantitative ventilation/perfusion scan often shows hypoperfusion of the affected segment and delayed ventilation of the affected segment with delayed washout (air trapping) (Figure 5).
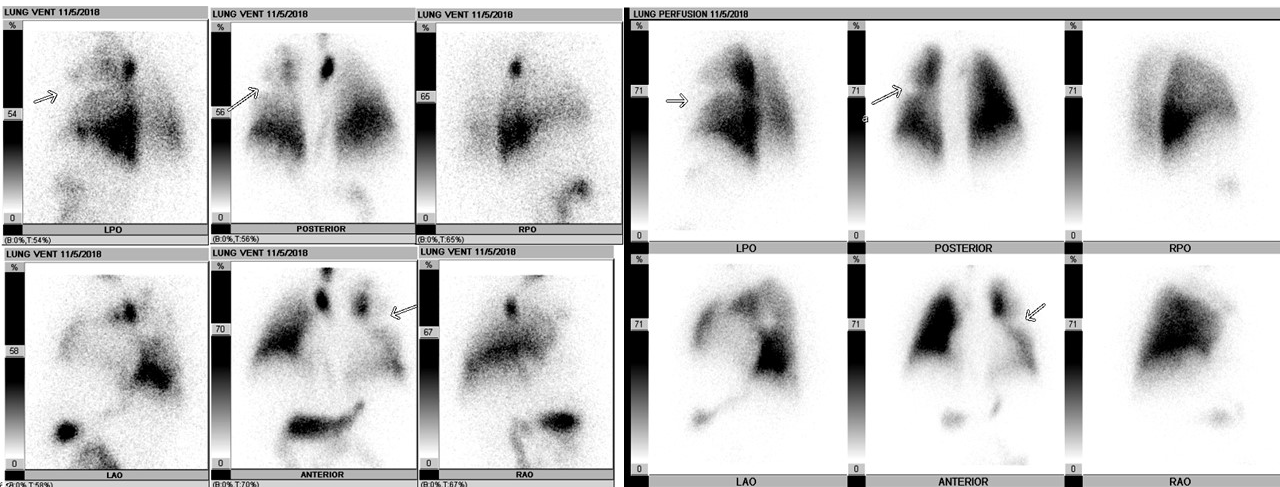
- Ventilation/perfusion scan shows a match defect with hypoperfusion of affected segment and delayed ventilation of affected segment with delayed washout (air trapping) (arrows).
Surgical excision should be reserved for patients with complications secondary to BA, such as recurrent infection or significant compromise of the adjacent lung parenchyma. Lobar resection and segmentectomy have been used with the goal of preserving as much normal lung parenchyma as possible to maintain pulmonary function.
The differential diagnosis for a perihilar tubular lesion with or without mucous impaction and hyperinflation can include congenital lobar emphysema, arteriovenous malformation, intralobar pulmonary sequestration, bronchogenic cyst, as well as mucoid impaction-associated conditions such as endobronchial lesions (ie, carcinoid), foreign bodies, cystic fibrosis, allergic bronchopulmonary aspergillosis, asthma, and TB.
Unlike BA, classic radiographic features of allergic bronchopulmonary aspergillosis include diffuse, central bronchiectasis with mucoid impaction primarily affecting the upper lung zones. Additionally, the distal lung is usually abnormal, with centrilobular tree-in-bud branching opacities. Congenital lobar emphysema is usually diagnosed in infancy with respiratory distress. Although the left upper lobe is most commonly affected, unlike with BA, there is no bronchocele. Furthermore, the hyperinflated lobe causes mass effect with a shift of the mediastinum away from the affected lobe. On contrast-enhanced CT, an arteriovenous malformation, which represents an abnormal feeding artery and draining vein, can appear tubular though will enhance with contrast. Additionally, there is no bronchial obstruction, hyperlucency, or hyperinflation.1