brucellosis can be from dairy products
- related: Infectious Disease ID
- tags: #literature #id
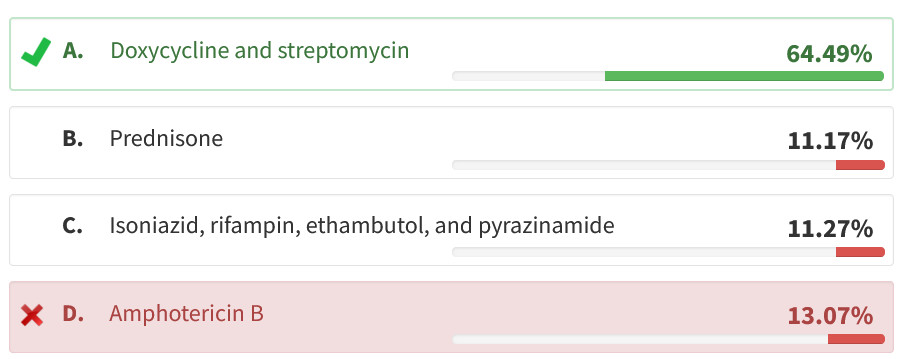
The presentation of recurring fevers, night sweats associated with pulmonary abnormalities, noncaseating granulomas on lung biopsy, and recent travel lead to a broad differential that includes TB, sarcoidosis, lymphoma, and fungal disorders. The severe leukopenia and anemia are suggestive of an intracellular pathogen, the three most common of which are Brucella, Salmonella, and Ehrlichia. The negative acid-fast bacilli smears/cultures, negative fungal stains/cultures, and a recent exposure to unpasteurized dairy in a part of the world endemic with brucellosis point to brucellosis as the most likely etiology over sarcoid, TB, or fungal infection. Treatment is often difficult, and relapse can occur (more common with monotherapy). Treatment should include a minimum of two-drug therapy with doxycycline and an aminoglycoside (streptomycin or gentamicin) (choice A is correct; choices B, C, and D are incorrect).
This case illustrates the uncommon presentation of a common disease entity. Although pulmonary nodules are a rare manifestation of brucellosis (1%-4% of cases), this disease should be suspected in patients with compatible symptoms who have traveled in endemic regions.
Brucellosis is a highly contagious zoonosis caused by ingestion of contaminated meat or unpasteurized dairy products from infected animals. It is the most common zoonosis worldwide, with a half a million cases reported annually. It is endemic in the Mediterranean basin and is also known as Mediterranean or undulant fever. Brucellosis can also be found in the Middle East, Central Asia, sub-Saharan Africa, and the Americas (Mexico, Central America, and South America). Animal-to-human transmission usually occurs via ingestion of food products (unpasteurized dairy) from animals such as cattle, sheep, goats, and camels. Clinical features of brucellosis are undulating fever, cough with mucopurulent sputum, myalgias, arthralgias, leukopenia, aminotransferase elevation, and abnormal chest imaging. Diagnosis can be difficult and requires the clinician to have a high suspicion for brucellosis based on signs, symptoms, and an exposure history (travel to an endemic area). Diagnosis is usually made from a culture of the organism from body fluids or tissue. The sensitivity of blood cultures can vary widely, and thus blood cultures can often be falsely negative (as in this case). If there is a high suspicion for brucellosis, then tissue cultures should be obtained from an alternative site. Bone marrow cultures have the highest sensitivity and are the gold standard for diagnosing brucellosis. Biopsy of the bone marrow, liver, or lung may demonstrate noncaseating granulomas (as in this case). Other modes of diagnosis include antibody titers >1:160 by standard tube agglutination test or isolating Brucella DNA on a polymerase chain reaction assay.123456
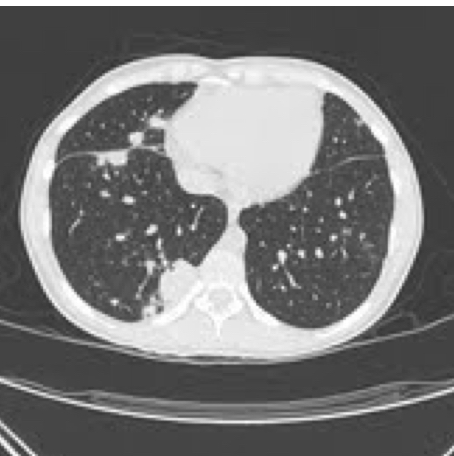
A 25-year-old, previously healthy, active duty marine presents with recurring fevers, night sweats, sore throat, cough productive of yellowish sputum, lethargy, and a dull frontal headache for 7 days. Review of the electronic medical record shows that he has had several previous visits over the last 3 weeks for respiratory symptoms, arthralgia, and loose stools that have been unresponsive to antibiotics, nonsteroidal anti-inflammatories, and metered-dose inhalers. He recently returned from Afghanistan where he was assigned to the public affairs officer and was engaged in community outreach. For his last mission, he visited a village of goat herders and drank milk offered during a meeting with local village elders. The patient appears ill and uncomfortable, complains of dyspnea, and has new right-sided pleuritic chest pain. He is soaked in sweat and is shaking in the bed. His vital signs include a temperature of 38.9°C, heart rate of 124/min, and BP of 85/40 mm Hg. There is cervical adenopathy and decreased breath sounds at the right lung base. Chest CT reveals diffuse lung nodules (Figure 1). He is started on broad-spectrum antibiotics. Labs demonstrate leukopenia, mild anemia, elevation of erythrocyte sedimentation rate and C-reactive protein, and mildly elevated transaminase values. Blood cultures, BAL bacterial cultures, BAL fungal cultures, and BAL acid-fast bacilli smears are negative. The patient remains ill with recurring fevers on a nightly basis, and oxygenation deteriorates progressively. A surgical biopsy specimen from one of the lung nodules is shown (Figure 2). What is the best therapy for his underlying condition?

Links to this note
Footnotes
-
Gotuzzo E, Carrillo C, Guerra J, et al. An evaluation of diagnostic methods for brucellosis—the value of bone marrow culture. J Infect Dis. 1986;153(1):122-125. PubMed ↩
-
Pappas G, Bosilkovski M, Akritidis N, et al. Brucellosis and the respiratory system. Clin Infect Dis. 2003;37(7):e95-e99. ↩
-
Skalsky K, Yahav D, Bishara J, et al. Treatment of human brucellosis: systematic review and meta-analysis of randomised controlled trials. BMJ. 2008;336(7646):701-704. PubMed ↩
-
Theegarten D, Albrecht S, Totsch M, et al. Brucellosis of the lung: case report and review of the literature. Virchows Arch. 2008;452:97-101. ↩
-
Yousefi-Nooraie R, Mortaz-Hejri S, Mehrani M, et al. Antibiotics for treating human brucellosis. Cochrane Database Syst Rev. 2012;(10):CD007179. PubMed ↩