cor pulmonale is right heart failure from pulmonary hypertension
- related: Pulmonary Diseases
- tags: #literature
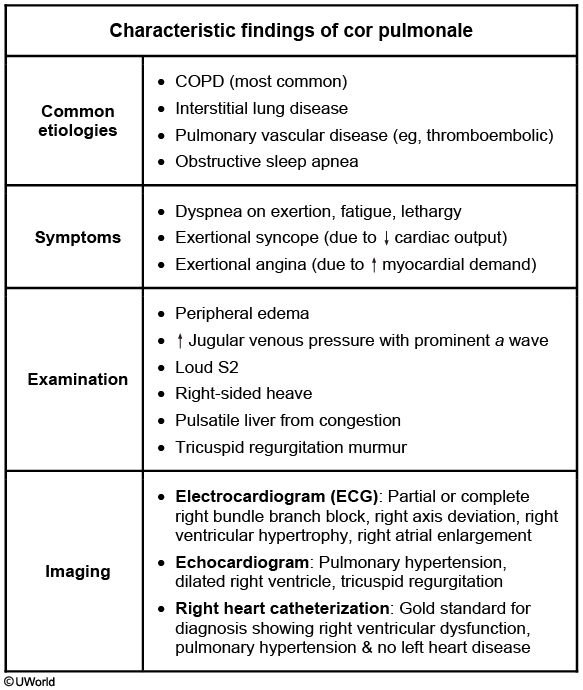
This patient’s presentation suggests cor pulmonale, defined as right-sided heart failure (RHF) from pulmonary hypertension (PH). PH may be idiopathic or due to chronic obstructive pulmonary disease (COPD), interstitial lung disease (eg, idiopathic pulmonary fibrosis), obstructive sleep apnea, pulmonary vascular disease (eg, thromboembolic), or chest wall disorders (eg, kyphoscoliosis). RHF due to left-sided or congenital heart disease is not considered cor pulmonale. COPD is the most common cause of cor pulmonale in the United States, with nearly 25% of COPD patients developing this disorder.
Cor pulmonale typically has a gradual onset but can present acutely due to a sudden increase in pulmonary artery pressures (eg, pulmonary embolism). Patients often develop exertional symptoms (eg, dyspnea, angina, syncope). Physical examination may show loud P2 (pulmonic component of the 2nd heart sound), tricuspid regurgitation murmur (holosystolic at the left lower sternal border), elevated jugular venous pressure (JVP), peripheral edema, hepatomegaly due to hepatic congestion, and possible ascites. COPD patients usually have distant heart sounds due to hyperinflated lungs. End-stage cor pulmonale may present with hypotension, tachycardia, and other signs of cardiogenic shock due to decreased stroke volume.
Chest x-ray may show enlarged central pulmonary arteries and loss of retrosternal air space due to right ventricular hypertrophy. Electrocardiogram usually shows right axis deviation, right bundle branch block, right ventricular hypertrophy, and right atrial enlargement. Right heart catheterization is the gold standard for diagnosis and typically shows elevated central venous pressure, right ventricular end-diastolic pressure, and mean pulmonary artery pressure (>25 mm Hg at rest) without left heart disease. Treatment involves optimizing right ventricular dynamics (preload, afterload, and contractility) with supplemental oxygen, diuretics, treatment of underlying etiology, and intravenous inotropes for severe decompensation.