domestically acquired particulate lung disease or hut lung
- related: Pulmonary Diseases
- tags: #literature #pulmonology
This patient meets the diagnostic criteria for domestically acquired particulate lung disease (DAPLD or “hut lung”), a pneumoconiosis that occurs secondary to inhalation of smoke derived from biomass fuels used for cooking in poorly ventilated huts or domestic settings. Historically, the term “hut lung” had been coined to collectively represent a constellation of clinical conditions including chronic bronchitis, chronic obstructive pulmonary disease (COPD), and interstitial lung disease associated with exposures to biomass smoke. There is a strong association between domestic exposure to household fuel combustion and the development of lung disease. Half of all households worldwide use combustion of solid fuels (dung, wood, agricultural residues, and coal) via open fires or simple stoves to cook or heat their dwellings. Women and children from lowto middle-income countries across Asia, Africa, and Latin America are disproportionately exposed to biomass fuels for cooking and heating. The following criteria are considered diagnostic of hut lung disease: 1) Individuals originating from rural dwellings; 2) exposure to biomass smoke from cooking fires, or who had ground maize; 3) No prior exposure to mining or other industry; 4) No prior exposure to, or evidence of, active tuberculosis; 5) Radiographic and histopathological evidence of pneumoconiosis.
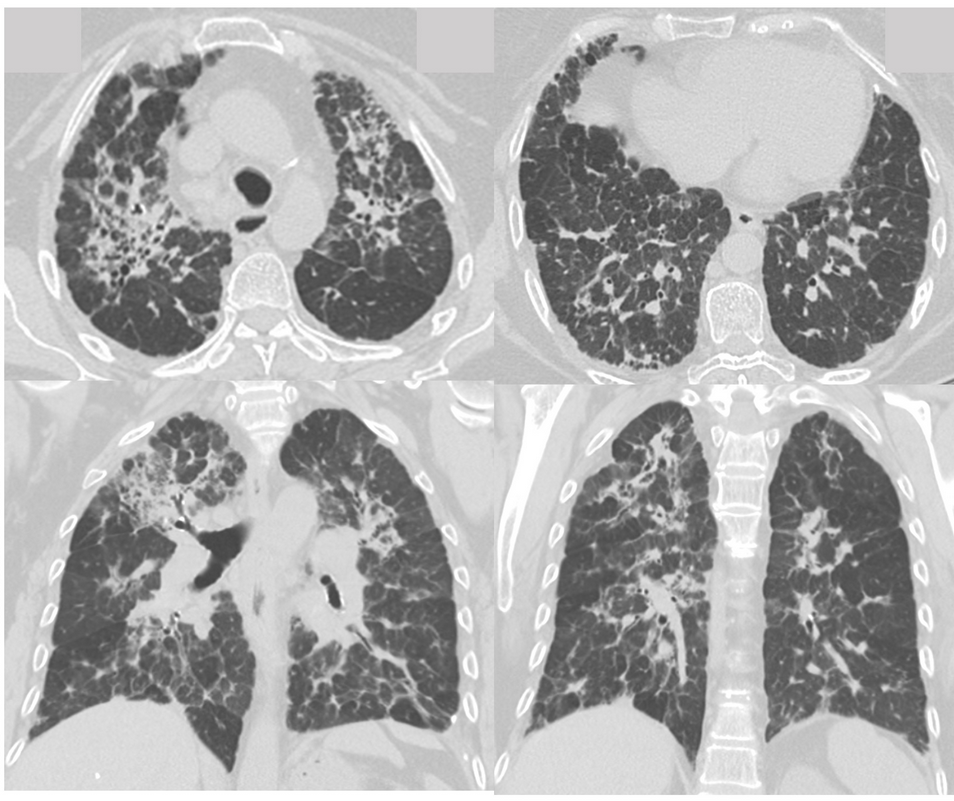
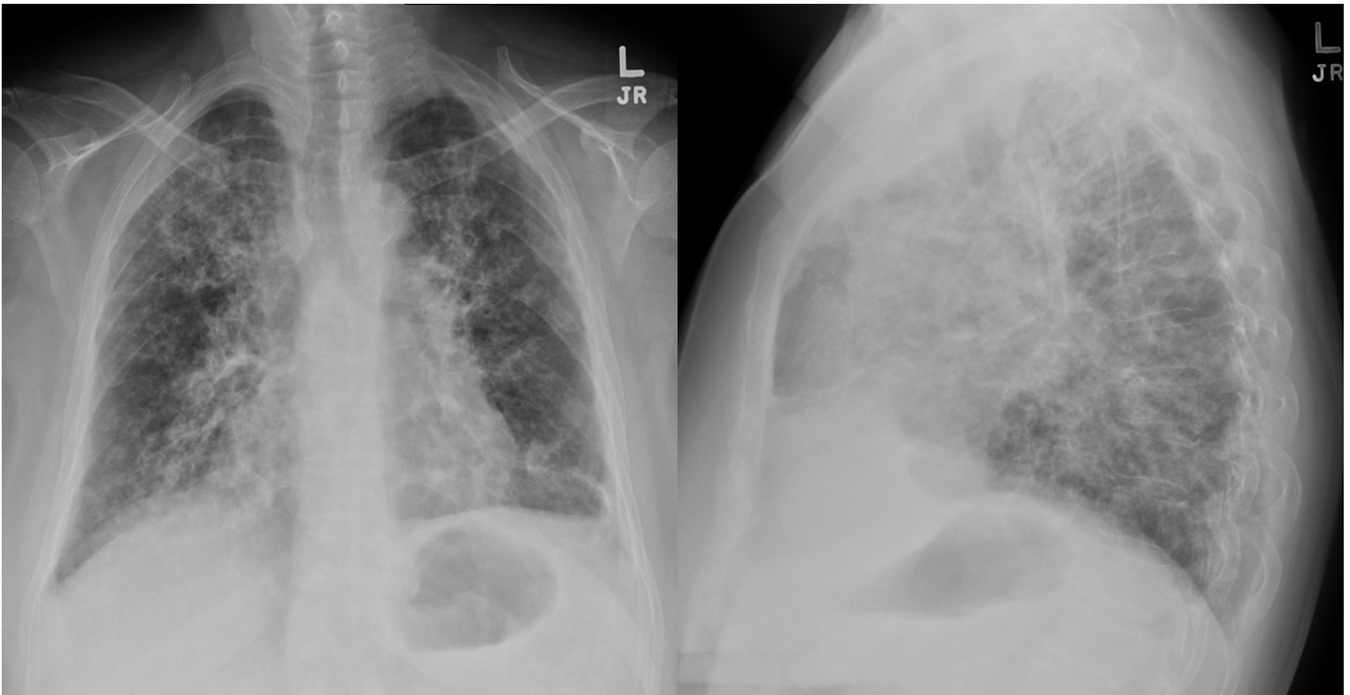
Patients with hut lung can present with a broad range of symptoms such as cough or dyspnea, to the more debilitating pulmonary hypertension and cor pulmonale. A wide spectrum of pulmonary physiologic abnormalities have been reported, ranging from normal, mild, or severe airway obstruction, reduction diffusing capacity, as well as a restrictive and mixed pattern. The chest CT pattern of women with biomass smoke exposure and a preexisting diagnosis of COPD are described as “airway-predominant” with less emphysema than women with COPD and a smoking history. The morphological characteristics of interstitial lung disease (ILD) in these patients has been poorly defined. The radiographic characteristics of hut lung disease can be distinctive from most common ILDs, such as usual interstitial pneumonitis (UIP) and nonspecific interstitial pneumonitis (NSIP). The parenchymal abnormalities seen in hut lung disease—notably mid-to-upper lung zone reticulation, bronchial wall thickening, ground glass opacities and mosaicism—most commonly resemble those seen in chronic hypersensitivity pneumonitis.
This patient’s radiographic and histopathologic findings are not consistent with the diagnosis of idiopathic pulmonary fibrosis (IPF). The cardinal radiographic features of IPF are peripheral basilar reticulation, traction bronchiectasis, and subpleural honeycombing with a craniocaudal gradient. The histologic hallmark of IPF is a heterogeneous appearance with alternating areas of normal lung, interstitial inflammation, fibroblast foci, and honeycomb change, admixed with fibroblastic foci, which are areas of active fibroproliferation.
This patient’s radiographic and histopathologic findings are also inconsistent with that of asbestosis. The radiographic manifestations of asbestosis includes basilar-predominant subpleural fibrosis with parenchymal bands, subpleural curvilinear lines, interlobular septal thickening, intralobular lines, irregular opacities, traction bronchiectasis, and honeycombing (UIP pattern). There is often concurrent evidence of pleural plaques or pleural thickening. Examination of lung tissue is rarely, if ever, needed for the diagnosis of asbestosis. For the majority of such patients, a confident diagnosis can be made on the basis of the exposure history and the CT findings.
Lastly, this patient’s clinical, radiographic, and histopathologic findings are also inconsistent with respiratory bronchiolitis-associated interstitial lung disease (RB-ILD). Virtually all patients with RB-ILD are current or former longtime cigarette smokers. Patients typically present with subacute symptoms of dyspnea, wheezing, cough, and sputum production. CT findings in RB-ILD commonly consist of patchy ground glass opacities, centrilobular nodules, and air trapping (Figure 6). The histologic hallmark of RB-ILD is the accumulation of tan-pigmented macrophages within the lumens respiratory bronchioles with associated submucosal and peribronchiolar infiltrate of lymphocytes and histiocytes.