ECMO oxygenator not working or not connected
- related: ECMO extracorporeal membrane oxygenation
- tags: #literature #icu
This patient has developed acute hypoxemia on ECMO. The differential is extensive and includes patient, mechanical ventilator, and ECMO circuit factors. In this case, the problem appears to be with the ECMO circuit. The patient does not have any increase in oxygenation across the oxygenator (ie, P1 and P2 PO2 values are almost identical). Two potential causes of this are poor functioning of the oxygenator (usually due to clot formation on the oxygenator surface) or inadequate oxygen supply to the oxygenator. The difference between the P1 and P2 pressures in the ECMO circuit gives an estimate of flow resistance across the oxygenator. The relatively normal difference between the P1 and P2 pressures (20 mm Hg pressure difference) (Figure 1) suggests that the oxygenator is functioning appropriately and is not burdened with significant clot or P2 obstruction. A pressure gradient of 70 mm Hg or more has been cited as a threshold that should prompt oxygenator exchange. Additionally, even with a failing oxygenator, some oxygen transfer should persist. In this case, the P1 PO2 of 32 mm Hg with a P2 PO2 of 35 mm Hg suggests no oxygen transfer by the oxygenator at all. This degree of oxygenator inefficiency is highly unlikely to be due to the oxygenator alone without an oxygen source issue. In this patient, the oxygen supply to the oxygenator was not reconnected to the wall oxygen source and instead was left on the portable oxygen tank that had been used while she was transported to the CT scanner. The portable oxygen tank had run out of oxygen, so the oxygenator was not receiving any supplemental oxygen.
Recirculation describes a large proportion of the oxygenated blood from the return cannula being drawn again into the ECMO circuit (via the drainage cannula), without being circulated throughout the body. The patient may become hypoxemic because of receiving little oxygenated blood from the ECMO. This can occur with high blood flows through the ECMO circuit or when the drainage and return cannulas are too close together in femorojugular venovenous configurations. It is less common when dual-lumen cannulas are used. When recirculation occurs, the blood in the P1 limb of the ECMO circuit has high PO2 levels, which are only slightly below those in the P2 limb of the ECMO circuit. This is not the case in this patient who has low PO2 values in both P1 and P2 limbs of the ECMO circuit.
Systemic oxygenation of patients on venovenous ECMO is a confluence of blood returning from the ECMO circuit and venous blood returning from the body and is directly related to the ratio of ECMO flow to cardiac output. Increasing the blood flow through the ECMO circuit will provide a larger volume of oxygenated blood to mix with the deoxygenated venous blood and should raise systemic oxygenation. However, in this patient, the oxygenator is not providing oxygenated blood due to a poor oxygen source. Increasing the blood flow in this scenario will not improve systemic oxygenation and may even worsen the patient’s hypoxemia.12345
A 45-year-old woman is being treated for ARDS due to influenza A pneumonia. She is supported with venovenous extracorporeal membrane oxygenation (ECMO) through a dual-lumen catheter via her right internal jugular vein, with 3.5 L/min of blood flow, 3 L/min of sweep gas flow, and 100% FdO2. She has been slowly improving over the last 5 days and is now mechanically ventilated on volume assist-control with a tidal volume of 350 mL (5 mL/kg of predicted body weight), respiration rate of 12/min, FiO2 of 1.0, and PEEP of 8 cm H2O. On these settings, heart rate is 94/min, and BP is 105/60 mm Hg. Pulse oximetry (left index finger) is 93%. She is awake and interactive and resting comfortably in bed, breathing at a rate of 15/min. One hour after returning from CT scanning, she develops acute hypoxemia with SpO2 of 62%. Heart rate is 145/min, and BP is 155/90 mm Hg. Respiratory rate is 32/min, and she appears distressed. Arterial blood gas analysis shows a pH of 7.22, PCO2 of 35 mm Hg, and PO2 of 47 mm Hg. Arterial lactate is 6.8 (0.5-2.0) mg/dL (0.75 [0.06-0.22] mmol/L). The blood in the drainage and return circuits of the ECMO machine appears dark red. A preoxygenator (P1) blood gas shows a pH of 7.12, PCO2 of 44 mm Hg, and PO2 of 32 mm Hg, while that after the oxygenator shows a pH of 7.15, PCO2 of 42 mm Hg, and PO2 of 35 mm Hg. Figure 1 shows the P1 and postoxygenator (P2) pressures in the ECMO circuit.
What action should be taken at this point to alleviate the patient’s hypoxemia?
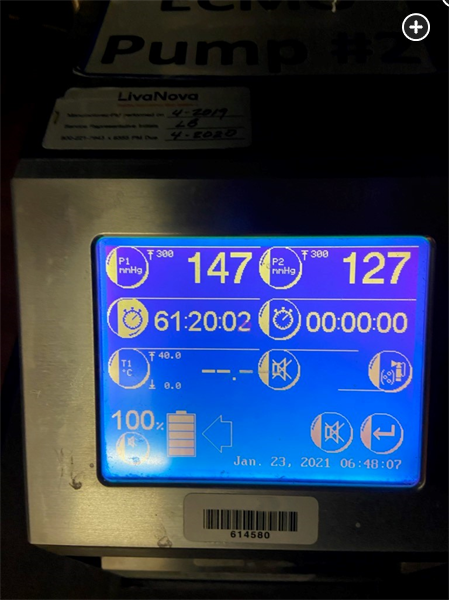
P1 represents the preoxygenator pressure (ie, the positive pressure in the circuit between the pump and the oxygenator), and P2 represents the pressure in the postoxygenator (ie, return) limb of the ECMO circuit. The difference between P1 and P2 represents the pressure gradient across the oxygenator.
Links to this note
Footnotes
-
Abrams D, Bacchetta M, Brodie D. Recirculation in venovenous extracorporeal membrane oxygenation. ASAIO J. 2015;61(2):115-121. PubMed ↩
-
Abrams D, Brodie D. Extracorporeal membrane oxygenation for adult respiratory failure: 2017 update. Chest. 2017;152(3):639-649. PubMed ↩
-
Messai E, Bouguerra A, Guarracino F, et al. Low blood arterial oxygenation during venovenous extracorporeal membrane oxygenation: proposal for a rational algorithm-based management. J Intensive Care Med. 2016;31(8):553-560. PubMed ↩
-
Patel B, Arcaro M, Chatterjee S. Bedside troubleshooting during venovenous extracorporeal membrane oxygenation (ECMO). J Thorac Dis. 2019;11(suppl 14):S1698-S1707. PubMed ↩